RSV, An Opportunistic Assassin
Respiratory syncytial virus (RSV) is a single-stranded, ribonucleic acid (RNA) virus that was first discovered in chimpanzees in 1955, and subsequently confirmed in humans1. The virus is highly infectious virus and is one of the leading causes of lower respiratory tract infections (LRTIs) in children2. Moreover, RSV infection occurs seasonally, with an annual peak of infection reported during rainy seasons in the tropical climates and the cold seasons in the temperate climates. Notably, RSV infections affect an estimated 24.8 million individuals, globally, and are attributed to 76,000 deaths2. Furthermore, approximately over 3 million annual hospitalisation seen in those under the age of 6 is attributed by the RSV; thus labelling RSV as an “opportunistic killer,” since it typically targets children with premorbid conditions3. Contrary to this, symptoms of RSV infection are usually absent or mild in older children and adults2.
Of note, RSV spread via respiratory droplets with an incubation period after inoculation from 2 to 8 days1 and causes significant damage to bronchiolar epithelial cells leading to small airway obstruction, hyperinflation and atelectasis4. Most concerning feature of RSV is related to a lack of effective antiviral treatment or vaccine to combat the virus, particularly in high-risk children. Moreover, despite prophylaxis use of palivizumab, a humanised monoclonal antibody that was designed to inhibit an epitope at the A antigen site of the F-protein of RSV subtypes A and B, the mortality rate, adverse events, or length of hospital stay related to RSV has not significantly improved5. However, this is about the change with Nirsevimab, a recombinant human immunoglobulin G1-kappa monoclonal antibody.
RSV is More Than Just a Flu
RSV typically manifests as an upper respiratory illness and may involve the lower respiratory tract. What if the virus is limited to the upper respiratory tract (URT), then what are the symptoms? RSV affecting the URT may cause rhinorrhoea, nasal congestion, cough, sneezing, and sometimes fever and myalgia. Those with lower respiratory tract (LRT) involvement may present with tachypnoea, accessory muscle use, wheezing, and prolong expiration, all of which are classical findings of bronchiolitis1. So, what is RSV same as influenza, how to differentiate between them? Well both RSV and influenza are highly contagious respiratory viruses. However, influenza virus often causes myalgia, fatigue, and pyrexia. Patient rarely experience dyspnoea when infected with influenza unless they have underlying respiratory illness. Contrary to this, patients with RSV often present with wheezing, dyspnoea, pyrexia, and cough6. Furthermore, it is often difficult to distinguish between the two until a formal laboratory assessment is performed6.
The differences in severity and clinical outcome of RSV versus influenza in adult hospitalised with acute respiratory illnesses was assessed by a study by Begley et al., (2023)7. The study involved 10,311 hospitalised adults, 6% tested positive for RSV (n=622) and 18.8% for influenza (n=1,940). Congestive heart failure (CHF) or chronic obstructive pulmonary disease (COPD) was more frequent with RSV than influenza (37.3% case of CHF in RSV patients and 28.8% in patients with influenza, p<0.0001; COPD: 47.6% vs 35.8%, p<0.0001)7. Furthermore, the results showed patients with RSV experienced frequent and longer hospital admissions (odds ratio [OR], 1.38; 95% confidence interval [CI]: 1.06-1.80] for stays >1 week) and required mechanical ventilation (OR 1.45; 95% CI: 1.09-1.93) compared to patients with influenza. The conclusion drawn from the study suggested those with RSV has a worse outcome compared with influenza and frequently have cardiopulmonary conditions7.
Nirsevimab May Help Crack the RSV Reign
Considering RSV is a leading cause of childhood acute LRTI, and a major cause of hospital admission globally resulting in substantial global burden8, an urgent treatment is warranted. The availability of nirsevimab may change this trend, particularly in vulnerable populations. But what is so special about this drug? Nirsevimab is a monoclonal antibody that binds to the F1 and F2 subunits of RSV fusion (F) protein at a highly conserved epitope and locks the RSV F protein in the prefusion conformation to block viral entry into the host cell8. The safety and efficacy of nirsevimab was tested in MELODY study, a randomised controlled trial that included a total of 1,490 infants randomised to receive either nirsevimab or placebo before the start of RSV season. The primary efficacy end point was medically attended RSV-associated LRTI through 150 days after infection. The second efficacy end point was hospitalisation for RSV-associated LRTI through 150 days after the injection8. The results showed medically attended RSV-associated LRTI occurred in 1.2% in the nirsevimab group and in 5.0% in the placebo group (Figure 1). Patients treated with nirsevimab reached a staggering efficacy of 74.5% (95% CI: 49.6-87.1; p<0.001) for nirsevimab. In addition, the hospitalisation for RSV associated with LRTI was only seen in 0.6% of nirsevimab group compared to 1.6% in placebo group (p=0.07). The study concluded that a single injection of nirsevimab administered prior to RSV season protected health late-preterm and term infants from medically attended RSV-associated LRTI8. In summary, RSV is a contagious virus that has detrimental effects on patients; thus, early vaccination against RSV may prove to be an effective approach in
long-run.
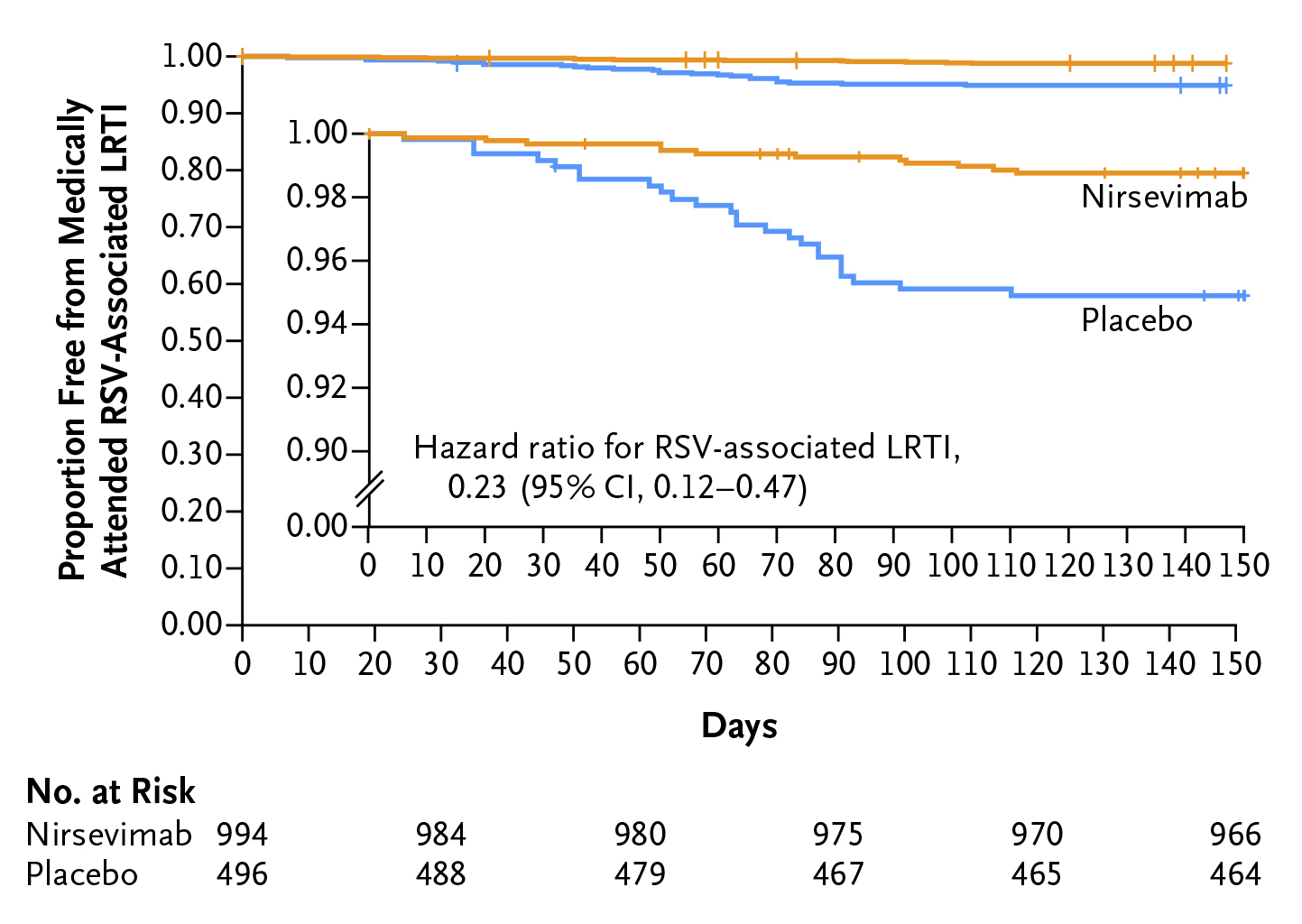
Figure 1. Lower respiratory tract infections (LRTIs) associated with the respiratory syncytial virus (RSV). Kaplan-Meier curve from a time-to-event analysis of the proportion of participants in the intention-to-treat population who were free from a medically attended RSV-associated LRTI8.
References
1. Jain H, et al. 2023 StatPearls Publishing 2. Du Y, et al. International Journal of Infectious Diseases 2023; 135: 70-6. 3. Caballero MT, et al. Pediatr Pulmonol 2018; 53(5): 664-7. 4. Miller S. et al. Journal of Pediatric Nursing 2010; 25(6): 551-4. 5. O'Hagan S, et al. Drug Healthc Patient Saf 2023; 15: 103-12. 6. Diseases NFfI. How to Tell The Difference Between Flu, RSV, COVID-19, And The Common Cold (accessed 12/01/2024). 7. Begley KM, et al. Clinical Infectious Diseases 2023; 76(11): 1980-8. 8. Hammitt LL, et al. New England Journal of Medicine 2022; 386(9): 837-46.





