
Is Exemption from Licensing Examination a Solution for Shortfall of Medical Services?
The population density of Hong Kong ranks amongst the highest globally, which imposes a high demand on medical services. The pressure on local medical system is intensified by the progressive population aging. According to the Healthcare Manpower Projection 2020 conducted by the Food and Health Bureau, the shortfall of medical doctors is expected to reach 1,610 in 20301. To alleviate the local demand on medical doctors, the government proposed an amendment to the Medical Registration Ordinance as a pathway for non-locally trained doctors to register for private practice in Hong Kong. Nonetheless, the proposal has incurred huge controversy among local medical professionals, politicians and patients. The purpose of this article is to discuss certain major issues related to the exemption of licensing examination for non-locally trained doctors to become registered in Hong Kong.
Projected Medical Manpower Demand
Currently, there are more than 14,000 medical doctors with full registration and about 6,800 specialists registered in Hong Kong. About 51% of registered medical doctors serve in public medical system, while the remaining practise in private sector1. Similar to the cases of most developed nations, the medical system in Hong Kong is challenged by the increasing proportion of elderly population and increasing occurrence of lifestyle-related diseases2.
Over the past years, the public medical system partnered with the private practitioners in order to ensure the sustainability of local medical services. Since 1990, the per capital doctor ratio has been increasing from 1.1 per 1,000 people in 1990 to about 2 per 1,000 people (1:511) in 20191,3. However, shortfall of local medical services has been reported that the waiting time of specialty services in the Hospital Authority (HA) is extremely long. For instance, according to government report, the waiting time for routine cases in orthopaedics and traumatology can be over 100 weeks4. Based on a manpower planning study conducted by the University of Hong Kong (HKU), there would be an estimated shortfall of 6.8%, about 1,007 full time equivalents (FTEs), in the number of medical doctors by 2030 (Figure 1)1. Thus, the Hong Kong government addressed that there is an urgent need to increase the number of medical doctors.
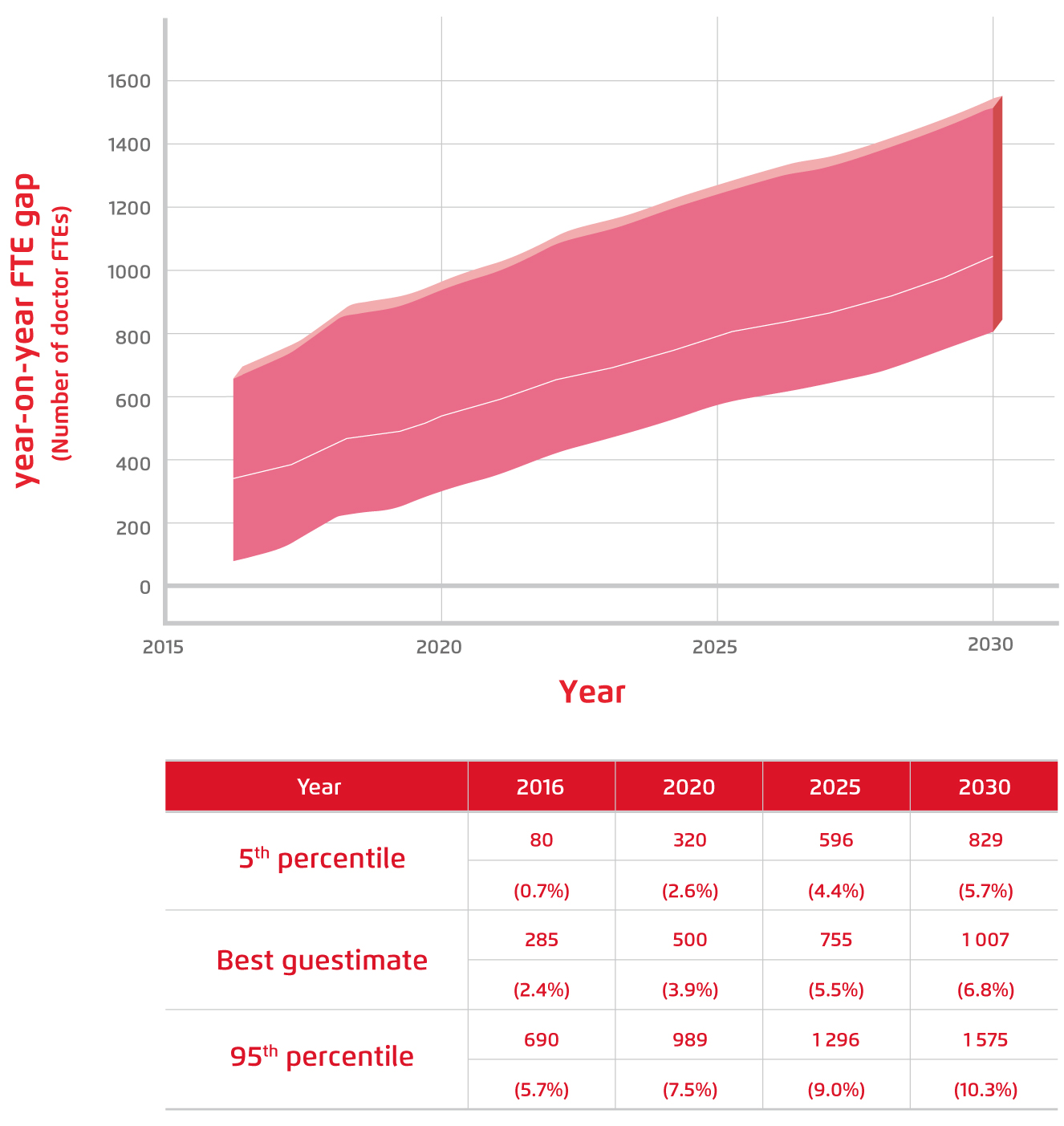
Figure 1.
Estimated manpower gap in FTEs1. Note: a positive estimate indicates shortfall
Government’s Proposal for Expanding the Pool of Doctors
There are various ways to increase the number of local medical doctors, including adopting a higher retirement age for current medical doctors, increasing local medical training capacity and recruiting non-locally trained qualified medical doctors. Particularly, in order to attract non-locally trained doctors to practise in Hong Kong, the government proposed to amend the Medical Registration Ordinance by allowing Hong Kong permanent residents who have graduated from an accredited overseas medical school and worked in a Hong Kong public health institution for at least five years to be exempted from the examination required to become registered doctors in Hong Kong. This Medical Registration (Amendment) Bill 2021 was gazetted on 21st May and was introduced into the Legislative Council on 2nd June5.
The Opinions of Local Medical Doctors
While the government expected the professionalism of the non-locally trained doctors can be proven by the accredited medical qualification and the clinical experience acquired in foreign settings as well as the 5-year practice in local public medical system, local medical doctors expressed their concerns on the professional standard of the non-locally trained doctors. The Hong Kong Doctors Union (HKDU) conducted an anonymous survey involving 193 local medical doctors on their opinions towards the government proposal on exemption from licensing examination for full registration for non-locally trained doctors.
The results revealed that most of the respondents (72.2%) agreed that current medical manpower in the public medical setting is not sufficient. However, 89.7% of the respondents replied that there is enough manpower in the private sector. Essentially, 75.3% did not support the proposal on exempting licensing examination for the non-locally trained doctors (Figure 2). Besides, the government proposal suggested allowing only graduates of the world top-100 medical schools to apply for the exemption. Nonetheless, only 35.2% of the respondents in favour of this suggestion, whereas 53.9% thought that other criteria had to be included in the assessment (Figure 3).
As a major point of controversy, more than 90% of respondents did not agree with the proposal on allowing exemption from licensing examination upon 5 years of clinical practice in the local public medical system. 62.9% supported that licensing examination was a must for full registration, whereas 27.3% expressed that the duration of 5 years was too short and longer training period would be required.
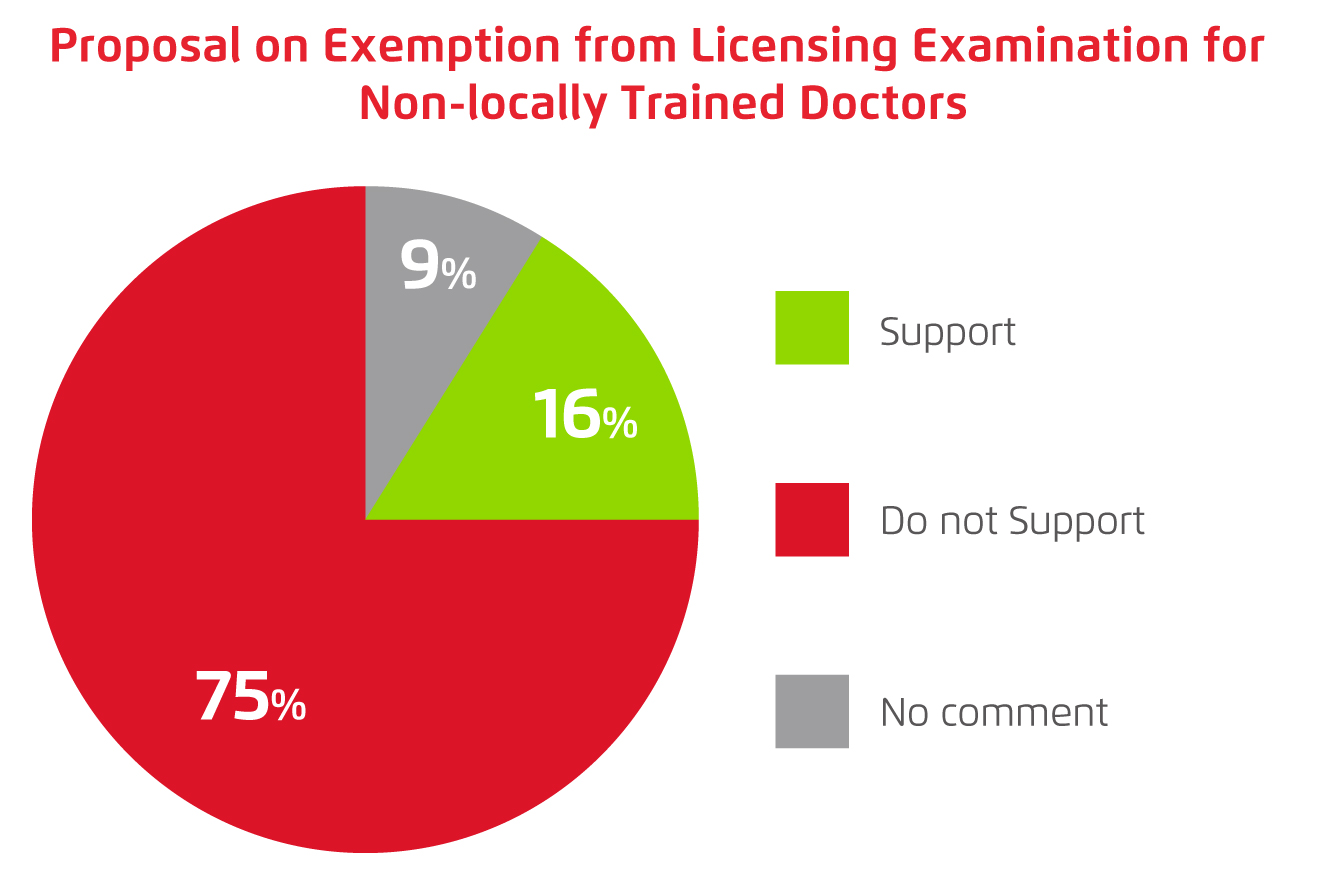
Figure 2.
Opinion on exemption from licensing examination by local medical doctors (data from HKDU)
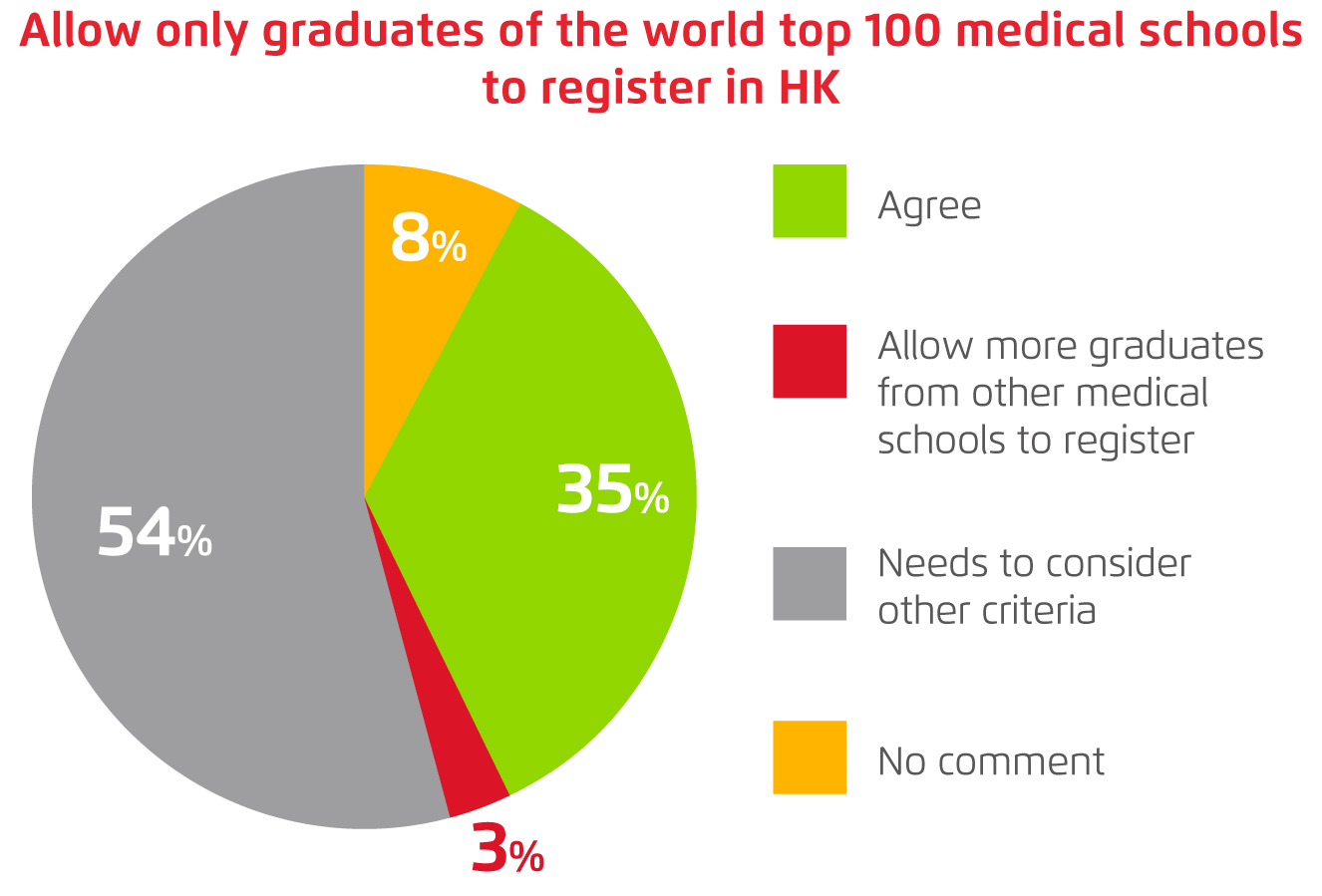
Figure 3.
Opinion on allowing only graduates of top-100 medical schools to apply for the exemption (data from HKDU)
Licensing Examination as the Door Guard
Based on the estimation by HKU, it is obvious that local medical manpower is insufficient and the shortfall is expected to be intensified with population aging and the increasing trends of various chronic diseases. However, the findings of the HKDU survey provided a more comprehensive view on the nature of manpower shortfall, which occurs mainly in the public medical system but not in the private sector. Notably, the areas in public medical system with serious shortfall are mainly specialty care services. Hence, expanding the pool of doctors in private sector might not be the right solution addressing the shortfall of medical services.
As reflected by the HKDU survey, most of the doctors concern about the professional quality of the non-locally trained doctors. Holtzman et al (2014) evaluated the country-to-country variation in performance of medical candidates by analysing the demographic characteristics and component scores of the United States Medical Licensing Examination. The results suggested that country-to-country differences in relative performance were present for both clinical discipline and task scores6.
More recently, a study by Pattinson et al (2019) evaluated the differences in clinical performance in specialty training between international medical graduates and local graduates in the United Kingdom demonstrated that theoretical versus real-life clinical experience was one of the major difficulties faced by the international graduates. Moreover, the results also highlighted that cultural barriers, including language barrier, played a significant role affecting the performance of the international graduates7.
The findings in former studies highlight the variations in clinical performance between international medical doctors and those locally trained. The possible explanations for the differences include differences in learning outcomes and curriculum emphasis of the medical training in different countries, variations in clinical experience, standards of care and cultural factors. Undoubtedly, a licensing examination tailored for the local clinical setting would likely be an effective way to govern the standard of clinical performance of the non-locally trained medical doctors. To solve the shortfall of medical services, besides expanding the pool of medical doctors, it is crucial to allocate additional resources on medical facilities such as hospital beds and operating rooms, as well as manpower on nursing and allied health professionals. Last but not least, in order to meet the actual needs in public medical services, further resources for specialist training are highly desirable.
Acknowledgement
The survey data reported in the current article is kindly provided by the Hong Kong Doctors Union (HKDU).
References
1. Food and Health Bureau. Strategic Review on Healthcare Manpower Planning and Professional Development. 2020. 2. Non-communicable Disease Branch, Centre for Health Protection of the Department of Health. Non-Communicable Diseases Watch November 2019 - Diabesity: A Lifestyle-related Epidemic. 2019 http://www.chp.gov.hk (accessed May20, 2021). 3. Department of Health. Health Facts of Hong Kong - Population and Vital Statistics. 2019. 4. Hong Kong Government. Admission of non-local doctors crucial. News.gov.hk.2021. 5. Hong Kong Government. Doctor registration pathway mooted. News.gov.hk 2021. 6. Holtzman et al. Acad Med 2014; 89: 1558-62. 7. Pattinson et al. BMJ Open 2019; 9: 30341.





