
Treatment on Antibiotic Resistance in Helicobacter Pylori
Helicobacter pylori (H. pylori) is a bacterium that infects more than half of the worldwide population.
H. pylori infection is the main cause of chronic gastritis and the etiological agent for gastric cancer and peptic ulcer disease1. One of the recommended regimens against H. pylori infection is clarithromycin-based triple therapy2. However, the rate of resistance in H. pylori to clarithromycin has been steadily increasing3. Recently, a study has reported that bismuth quadruple therapy achieves a better eradication rate against H. pylori compared with triple therapies in regions with high clarithromycin resistance4. This article briefly discusses the selection and effectiveness of treatments countering clarithromycin resistance in H. pylori.
More than half of the population in Eastern Asia was infected by H. pylori
As of 2015, a majority of the global population (approximately 4.4 billion) was infected by H. pylori1. A meta-analysis published in 2017 revealed that the prevalence of H. pylori infection varied among geographic regions, ranging from 24.4% in Oceania to 70% in Africa. In Eastern Asia including China, Taiwan, Japan and Korea, the prevalence rates of infection were reported as 51.7-55.8% (Figure 1)1. In Hong Kong, the prevalence was reported as 58.4%, whereas the local data has not been updated since 19991,5.
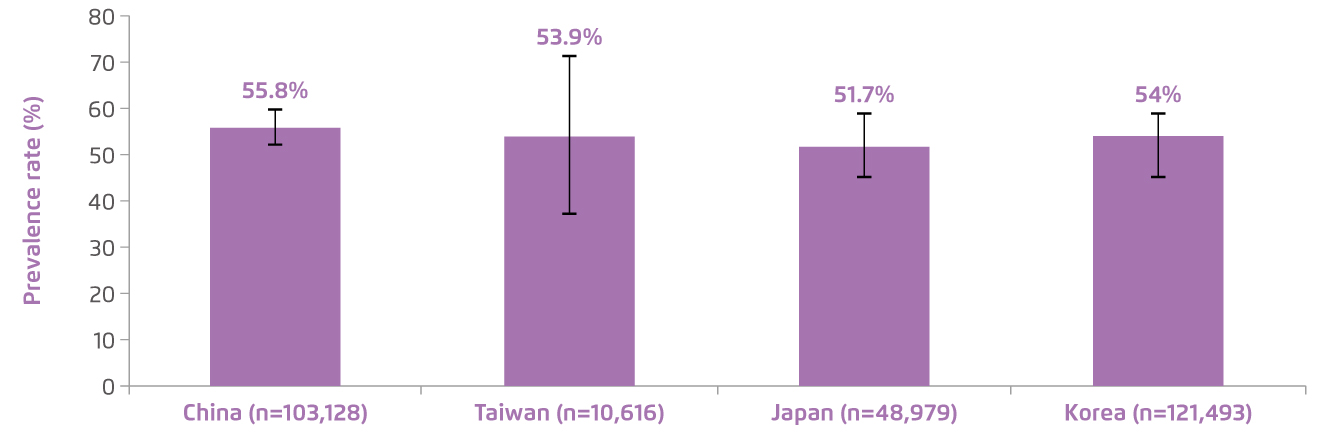
Figure 1. Pooled prevalence of H. pylori infection among Eastern Asia regions from 1970-20151. Error bars indicate 95% confidence interval.
Resistance to clarithromycin is steadily increasing
The resistance to clarithromycin has been identified as one of the major factors affecting H. pylori eradication success. A meta-analysis demonstrated that the overall resistance rate of clarithromycin in H. pylori was increasing over time, from 7% before 2000 to 21% in 2011-15 in the Asia-Pacific region (Figure 2)3. In China, the clarithromycin resistance was reported as 26%, leading to unacceptable eradication results of clarithromycin-based triple therapy (67-75%). Despite the fact that low resistance to clarithromycin was reported in Hong Kong (7.8% in 20066 and 10% in 20173), the findings suggest that clarithromycin resistance in H. pylori is steadily increasing over time and further study should be conducted to track the primary antibiotic resistance and guide the treatment selection.
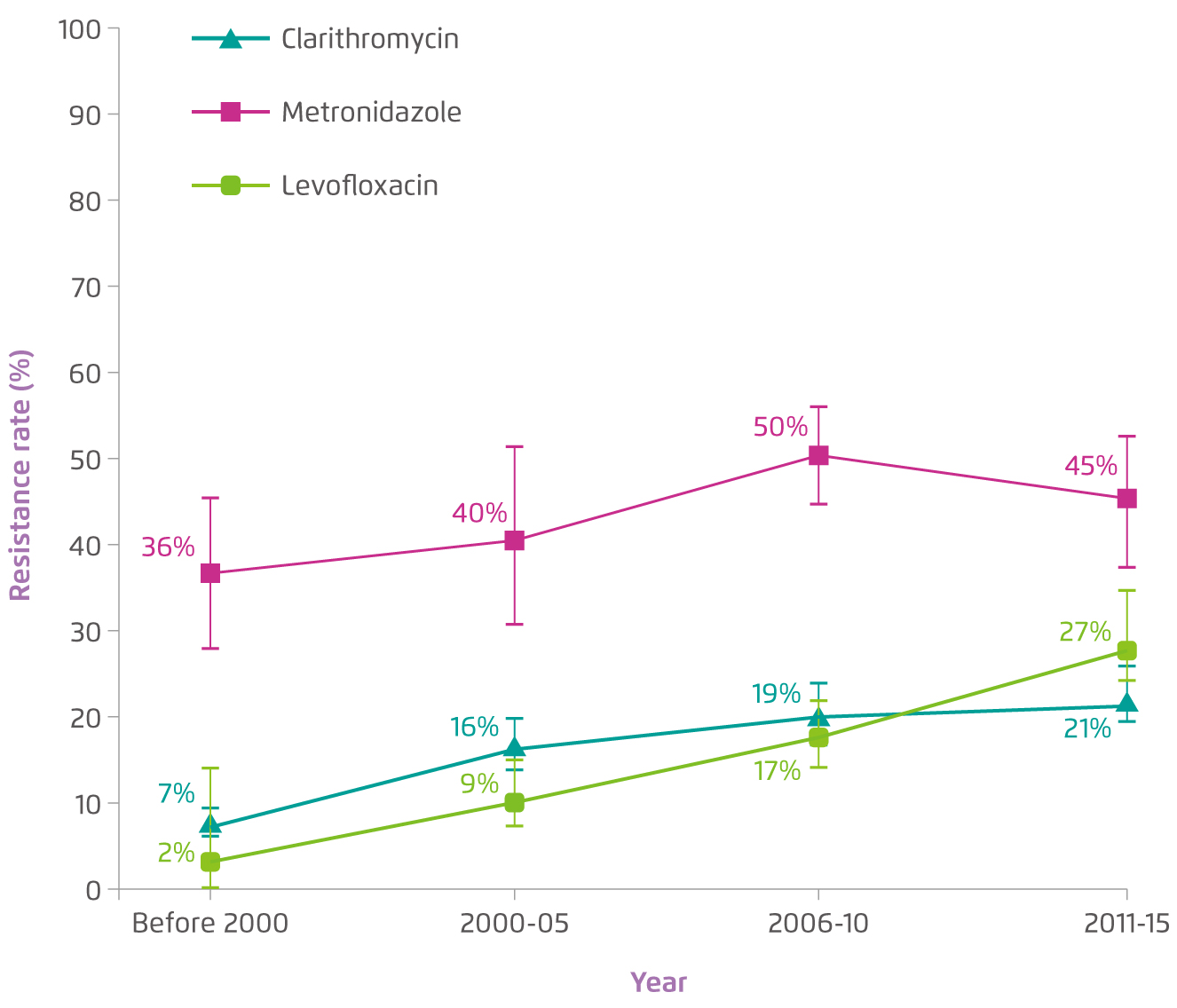
Figure 2. Overall resistance rate of primary antibodies in H. pylori over time in the Asia-Pacific regions3. Error bars indicate 95% confidence interval.
Treatment selection regarding clarithromycin resistance
According to the American College of Gastroenterology (ACG) Clinical Guideline, clarithromycin therapy in combination with amoxicillin and a proton pump inhibitor (PPI) has been listed as the first recommended treatment for H. pylori infection in patients without prior use of antibiotic treatment for the infection7. This regimen, in line with the expert’s consensus, should be employed in the region with a low resistance rate to clarithromycin (<15%)8,9. While in areas with high clarithromycin resistance rate (>15%), traditional bismuth quadruple or concomitant non-bismuth quadruple therapies are recommended7-9. In order to improve the eradication rate, the treatment duration is highly recommended to last for 14 days7-9.
Treatment trend and their effectiveness
A recent study, which included more than 30,000 patients from European countries, evaluated the trend and eradication rate of first-line empirical H. pylori treatments starting from 20134. The rate of pretreatment resistance was 23%, 32%, and 13% to clarithromycin, metronidazole, and both, respectively. Up to 2017, although clarithromycin-based triple therapy was the most commonly prescribed treatment, the trend was decreased from more than 50% in 2013/15 to less than 32% in 2017/18. In addition, the overall eradication rate of triple therapy was reported as 81.5% while 10-day bismuth quadruple or 14-day concomitant treatments achieved over 90% of eradication4. These findings suggest that bismuth quadruple therapy may be a reliable alternative for the treatment of H. pylori if the local clarithromycin resistance reaching the threshold.
To conclude, H. pylori is a common gastrointestinal infection in Asia, and undoubtedly, the resistance to antibiotics in H. pylori is developing and steadily increasing in many regions. In order to improve eradication rate, alternative treatment strategies should be adapted based on resistance patterns. Moreover, further analysis on antibiotic resistance should be conducted in order to provide insights on appropriate treatments.
References:
1. Hooi JKY, et al. Gastroenterology. 2017;153:420-429. 2. Cheung S & Tang AKY. Hong Kong Pract. 2018. Available at: https://www.hkcfp.org.hk/Upload/HK_Practitioner/2018/hkp2018vol40Sep/Internet.html (accessed on 6 Jan 2021) 3. Kuo Y, et al. Lancet Gastroenterol Hepatol. 2017;2:707-715. 4. Nyssen OP, et al. Gut. 2021;70:40-54. 5. Wong BCY, et al. J Gastroenterol Hepatol. 1999;14:120-125. 6. Gu Q, et al. Digestion. 2006;73:101-106 7. Chey WD, at al. Am J Gastroenterol. 2017;112:212-239. 8. Malfertheiner P, et al. Gut. 2017;66:6-30. 9. Fallone CA, et al. Gastroenterology. 2016;151:51-69.





