Migraine as the second most disabling disease contributes to significant prevalence at 18% in women and 9% in men. Despite maybe 4 out of 10 migraine patients could potentially benefit from migraine preventive medicines, but the utilization of and adherence to such treatment have been found low as 3 to 13%. Given the little knowledge about the comparative effectiveness among different preventive medicines, ranging from established to newly available, a Norwegian research team filled the knowledge gap with defined analysis of prescription data from nationwide prescription database. Treatment retention and effectiveness were the primary outcomes measured in the analysis. The former was defined as the duration of uninterrupted treatment periods, whereas effectiveness was approximated by measuring the reduction in a patient¡¦s triptan use which is indicated for improving migraine symptoms. Comparisons against beta blockers were performed among the following medicines recommended for migraine prophylaxis by clinical guidelines and/or in common use for this indication in Norway other than beta blockers: candesartan, lisinopril, topiramate, CGRPabs (calcitonin gene-related peptide pathway antibodies), BtA (botulinum toxin A), clonidine, and simvastatin. With 104,072 migraine patients identified, BtA, CGRPabs and simvastatin showed the highest proportion of patients remaining on treatment at 1 year after the first prescription at a rate of >20% (Figure 1). More than half of the patients achieved a 30% or greater reduction in triptan use with those medicines; patients on amitriptyline, CGRPabs and simvastatin were more likely to achieve clinically significant reduction in triptan use during the first 90 days of treatment. Amitriptyline and simvastatin are established medicines principally used for other conditions, while CGRPabs are developed and used specifically for migraine that may require additional healthcare cost. Therefore, a peek into brief cost-effectiveness profile among different migraine prophylaxes can somehow be obtained from this study in this sense.
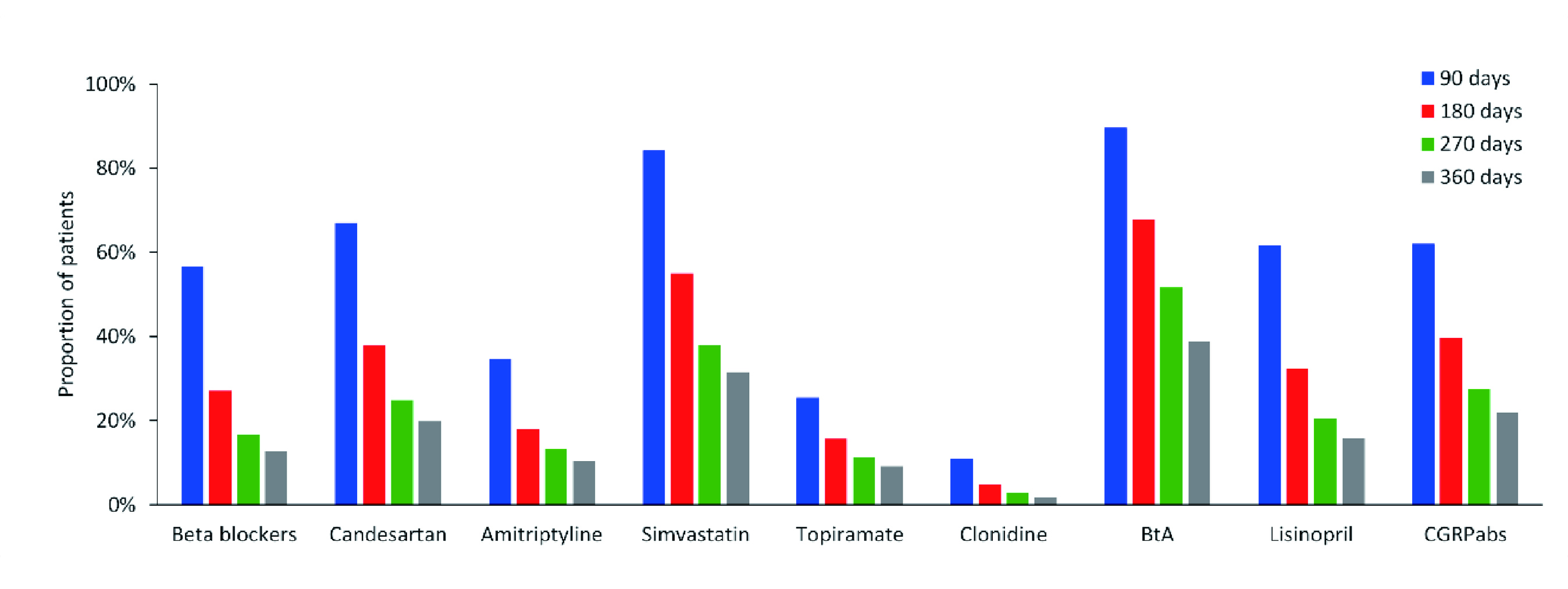 Figure 1. Proportion of patients still on preventive migraine therapy after 90, 180, 270 and 360 days Adapted from Bjørk MH, et al. 2023.
Figure 1. Proportion of patients still on preventive migraine therapy after 90, 180, 270 and 360 days Adapted from Bjørk MH, et al. 2023.
References
Bjørk MH, et al. Eur J Neurol. 2023 Sep 27





