
Risk Prediction and Preconception Counselling on Adverse Pregnancy Outcomes in Systemic Lupus Erythematosus
Pregnancy is challenging for both women with systemic lupus erythematosus (SLE) and their treating physicians as it is associated with an increased risk of adverse pregnancy outcomes (APOs) including prematurity, intrauterine growth restriction (IUGR), preeclampsia and foetal loss, maternal morbidity and mortality as well as syndrome of neonatal lupus1. In general, a multi-disciplinary team, consisting of a rheumatologist, an obstetrician and other healthcare professions are required to manage the care of pregnant patients with SLE. Although significant improvement in pregnancy outcomes of SLE patients have achieved with the recent obstetric advancement, APOs are still common with reported incidence of 19-58%2. Because of the obstetric complications, pregnancy has been discouraged in SLE patients especially when SLE is active. Thus, identifying pregnant SLE patients at an increased risk of APOs and appropriate preconception counselling would likely optimise their obstetric outcomes.
The Impact of Disease Activity during SLE Pregnancy
One of the major issues in SLE pregnancy is the risk of disease exacerbation. Although it is generally agreed that pregnancy may lead to higher rates of disease flares, widely variable flare rates of between 25-65% have been reported3,4. However, the responses to pregnancy vary among different organ systems. For instance, flares in musculoskeletal system are less common whereas renal and haematologic flares are more common5. Previous cohort study reported that majority of disease flares in SLE pregnancy are mild-to-moderate, while only small proportion of patients develop severe flares6.
Risk Factors and Predictive Models for APOs in SLE
Improvements in SLE treatment bring better quality of life for patients suffering from the disease and allow pregnancies in them. Yet, the pregnancy outcome is still unfavourable. The maternal and foetal risk in SLE patients is significantly higher as compared to healthy women, whereas lupus flare, hypertension, nephritis, preeclampsia, prematurity and IUGR are common maternal complications7. Former efforts have identified numerous risk factors for APOs in SLE patients. For instance, increased risk of pregnancy loss by 2.6 to 3.3 times in the first-trimester has been reported in patients with proteinuria and thrombocytopenia consecutively8. Essentially, disease activity at the time of conception would indicate the pregnancy outcomes that high SLE activity would lead to APOs9. Thus, good pregnancy plan for SLE patients is crucial that all pregnancies in SLE patients should ideally be planned during periods of disease control.
As clinical data identifying risk factors for APOs in SLE pregnancy is emerging, predictive models for APOs in SLE pregnancy have been developed in recent studies. Wu et al (2019) analysed foetal loss in a Chinese cohort of 338 SLE pregnancies retrospectively. The results suggested that unplanned pregnancies, hypocomplementemia C3 and an elevated 24 hour-urinary protein level were independent risk factors for foetal loss, whereas a scoring system was constructed to classify the foetal loss risk based on the regression coefficients of the 3 variables10.
Besides, in a recent retrospective cohort study by Palma dos Reis et al (2019), 157 pregnancies in 128 SLE patients were analysed. The study determined the key risk factors for each of the main APOs in the cohort. The results revealed that the main risk factors for foetal loss were maternal age and the presence of antiphospholipid antibodies (aPL). Lupus nephritis was predictive of a preterm delivery and preeclampsia, whereas renal involvement and lupus flares during pregnancy were risk factors for foetal growth restriction. In general, the main risk factor for APOs was lupus flares during pregnancy11.
Although further assessment on the external validities of the predictive models developed is needed, these models may help clinicians in identifying SLE patients with high risk pregnancies and stratifying risk for specific APOs, thereby carrying out effective counselling, monitoring and management for improving foetal outcomes.
Preconception Counselling and Assessment in SLE Pregnancy
There is well-established evidence proving that active SLE at the time of conception is the strongest predictor of APOs9,11. Hence, all pregnancies in SLE patients should ideally be planned during periods of disease control. However, former reports commented that natural and barrier methods of contraception have a high failure rate and may not be sufficient in a patient with active disease9. While the safety of oral contraceptives has been documented in previous clinical trials, patients with severe active disease were excluded from the studies12,13. Besides, oestrogen-containing contraceptives should be avoided in patients with aPL due to the high risk of thrombosis14. Based on the considerations on safety and effective contraception, an intra-uterine contraceptive device is suggested for SLE patients13.
In order to improve pregnancy outcomes in SLE patients, preconception assessment is an essential component of pregnancy planning and an overview of the risk assessment in SLE patients is listed in Table 115. The major objectives of the preconception assessment are to assess functions of the major organs and disease activity, to obtain a comprehensive autoantibody profile, especially aPL and anti-Ro antibodies, and to review the medications prescribed9.
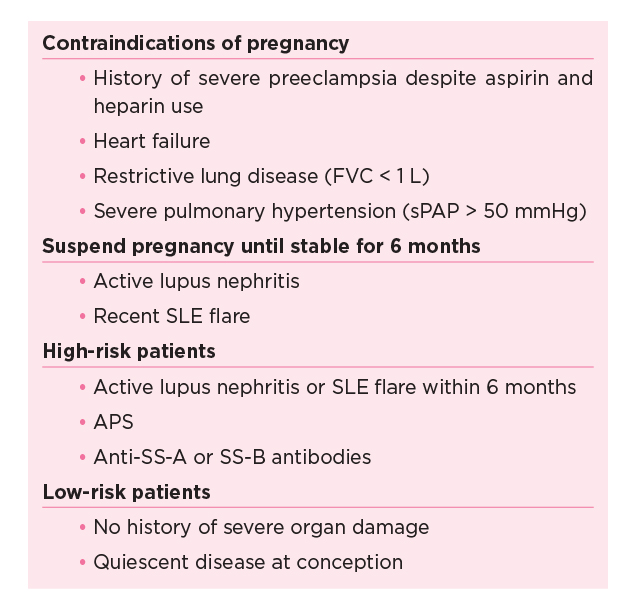
Table 1. Preconception risk assessment for SLE patients
SLE: systemic lupus erythematosus; FVC: forced vital capacity;
sPAP: systolic pulmonary artery pressure; APS: antipholipid syndrome
While patients often concern about foetotoxicity, they should be informed that discontinuation of medication may activate SLE and lead to pregnancy complications. Nonetheless, medications of the patients have to be reviewed and adjusted in order to minimise its effects on the foetus while controlling disease for the mother. Importantly, evidence-based recommendations on pharmaceutical management of SLE pregnancy have been addressed in international guidelines16,17.
Summary
Despite substantial improvement in success rates, pregnancy in SLE patients is still a high risk condition involving high maternal and foetal morbidity and mortality. Multidisciplinary care with close monitoring remains the core in management of SLE pregnancy. The development of predictive models and identification of risk factors facilitate early detection of threats to maternal and foetal well-being. Moreover, the information not only helps clinicians optimise management protocol in SLE pregnancy but also provide evidence support for effective patient counselling.
References
1. Marder. Curr Opin Rheumatol. 2019;31(6):650-658. 2. Buyon et al. Ann Intern Med. 2015;163(3):153-163. 3. Ruiz-Irastorza et al. Br J Rheumatol. 1996;35(2):133-138. 4. Carvalheiras et al. Clin Rev Allergy Immunol. 2010;38(2-3):302-306. 5. Petri. Rheum Dis Clin North Am. 2007;33(2):227-235. 6. Petri et al. Arthritis Rheum. 1991;34(12):1538-1545. 7. Hamijoyo et al. Acta Med Indones. 2019;51(2):102-109. 8. Clowse et al. Am J Obstet Gynecol. 2008;199(2):127.e1-6. 9. Lateef et al. Best Pract Res Clin Rheumatol. 2013;27(3):435-447. 10. Wu et al. BMJ Open. 2019;9(2). 11. Palma dos Reis et al. Clin Rev Allergy Immunol. August 2019. 12. Petri et al. N Engl J Med. 2005;353(24):2550-2558. 13. Sánchez-Guerrero et al. N Engl J Med. 2005;353(24):2539-2549. 14. Lateef and Petri. J Autoimmun. 2012;38(2-3). 15. Yamamoto and Aoki. Int J Womens Health. 2016;8:265-272. 16. Gordon et al. Rheumatology (Oxford). 2018;57(1):e1-e45. 17. Fanouriakis et al. Ann Rheum Dis. 2019;78(6):736-745.





