

Specialist in Obstetrics and Gynaecology
Human papillomavirus (HPV) is associated with most types of cervical cancers, and the recent increase in the incidence of head and neck cancers, particularly oropharyngeal cancer, in addition to anogenital cancers has been reported to have a link with the virus1. Considering HPV is primarily sexually transmitted, preventing HPV infection is of uttermost importance in both males and females. Remarkably, the HPV infection rates have been reduced effectively by the administration of HPV vaccination. However, the current HPV vaccine uptake rate remains suboptimal with cervical cancer still prevalent and a major cause of cancer deaths among local female population2. A better understanding of HPV and the implementation of effective strategies are required to improve the HPV vaccine uptake and screening to help reduce the disease burden. To help uncover the clinical issues of HPV, Dr. Tam Man Sum, Specialist in Obstetrics and Gynaecology, shed light on the pathophysiology of HPV and shared her expert opinion on the preventive measures taken against HPV infection locally.
Cervical cancer is the 4th most common type of cancer in females globally, accounting for an estimated 604,000 newly diagnosed cases and 342,000 related deaths in 2020. The global mortality rate from cervical cancer is high, with an age-standardised rate of 13.3/100,000 female population in 20203. The local disease burden of cervical cancer is equally significant, with 520 new cervical cancer cases diagnosed and a crude incidence rate of 12.7/100,000 female population in 2019 reported by the Centre for Health Protection (Figure 1). Furthermore, 159 females died from cervical cancer in the year 2020, constituting approximately 2.6% of female cancer-related deaths2.
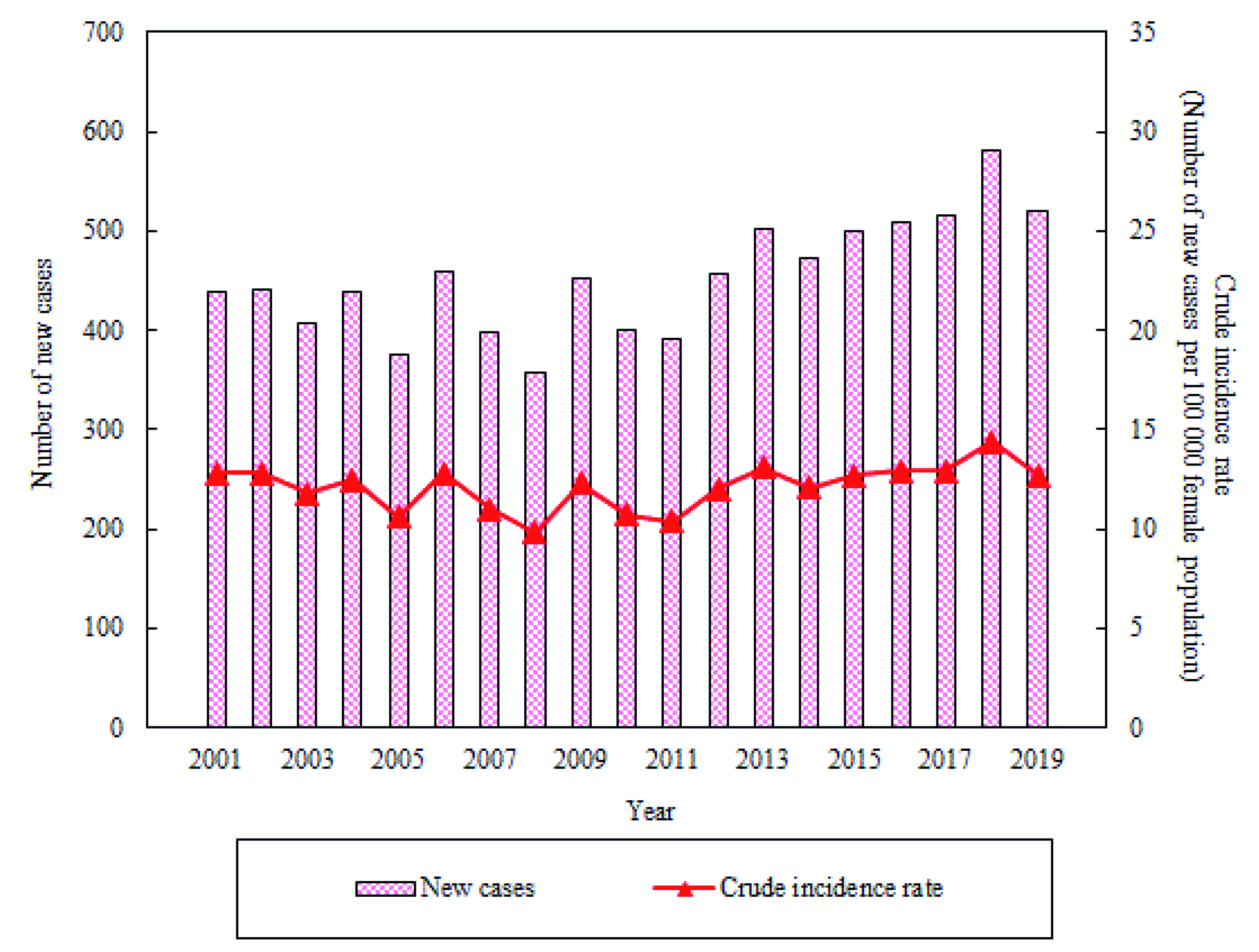
Figure 1. Number of new local cases and crude incidence rate of cervical cancer in 20192
Over 99.7% of cervical cancers are due to persistent infection with genital type high-risk HPV. In contrast to the incidence of cervical cancer, the estimated lifetime probability of acquiring HPV is unexpectedly high in both genders, with 84.6% cases reported in females and 91.3% in males4. This suggests that most sexually active males and females are infected with HPV at some point in their lives. In view of these reported statistics, Dr. Tam began by explaining HPV as a member of the Papovaviridae family, with more than 200 different HPV genotypes identified. Most HPV-related cancers are attributed to high-risk subtypes, such as HPV-16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 595. “HPV-16 and 18 are common high-risk types, accounting for approximately 70% of cervical cancer globally6,” according to Dr. Tam. She also added that most other HPV subtypes are classified as low-risk, including HPV-6 and 11, but can still cause benign diseases such as genital warts. While HPV infections are common, Dr. Tam advised that most HPV infections are asymptomatic and are usually cleared by the host’s immunity within 1-2 years after acquisition5.
Dr. Tam highlighted that high-risk HPV types have acquired several mechanisms to avoid detection and trigger host immune response. “The viruses are latent in general and keep a very low profile by maintaining a low number of HPV genome copies in the infected host basal cells. Thereby, these viruses can remain dormant in the host cells for a prolonged period of time; therefore, HPV-related cancers or pre-cancer lesions can take up to 10 years before it develops after acquiring initial infection,” Dr. Tam explained. In addition, the HPV cycle is exclusively intraepithelial and not lytic, therefore, preventing the activation of associated pro-inflammatory signal5.
HPV is primarily transmitted through sexual contact and is often discussed in the context of women’s sexual health due to its association with cervical cancer. Subsequently, the risk of HPV infection among sexual minorities is often overlooked. For instance, a cross-sectional study performed by Pelullo et al. (2012) in Italy involved a random sample of 1,000 lesbians, gay men, and bisexual women and men concluded that the mean value of perceived personal risk of contracting HPV infection on a scale of 1-10 was 6.2, and only 10% realised their risk and concerned regarding the issue7.
According to Dr. Tam, the risk of HPV-related diseases, such as anal cancer, was higher among homosexual males compared to the heterosexual counterpart. These findings were elaborated by Chidobem et al. (2022) that gay, bisexual, and men who have sex with men (MSM) were 17 times more likely to acquire anal cancer compared to heterosexual men8. Furthermore, a review by Meites et al. (2022) reported that the anal prevalence of high-risk HPV subtypes among MSM was 41.2% versus 6.9% among males who have sex with women. In addition, the review reported further prevalence of anal, penile, oral and urethral HPV infections among MSM were 78.4%, 36.2%, 17.3%, and 15.4%, respectively9.
Sexual minority females, such as lesbians and bisexual females, may perceive themselves less susceptible to HPV infection compared to heterosexual females7. Contrary to this belief, recent studies reported similar prevalence of HPV infection among both sexual minority and heterosexual females10.
Practically, HPV can be spread through skin-to-skin contact and by sharing fomites, such as sex toys during vaginal, anal and oral sex10. Of note, the presence of high-risk HPV subtype is necessary but may not be enough for cancer development. In fact, it is also dependent on certain factors that act in conjunction with the oncogenic HPV types. Remarkably, Dr. Tam highlighted that there is an increased risk of acquiring HPV infection among tobacco smokers. “Tobacco smoking generally weakens the host’s immunity, therefore impairs their ability to clear HPV,” according to Dr. Tam. Her comment was substantiated by a study performed by Xi et al. (2009) suggesting that active smokers exhibited a higher baseline HPV-16 and HPV-18 DNA load compared to the ex-smokers and non-smokers11.
Aside from smoking, Dr. Tam reminded us that HPV is primarily sexually transmitted, therefore, the age of first sexual intercourse, engaging in unprotected sexual intercourse, and sexual promiscuity increase the likelihood of acquiring HPV and related infections. Interestingly, the meta-analysis by Liu et al. (2015) reported a non-linear relationship between the number of sexual partners and the non-malignant cervical disease as well as invasive cervical carcinoma, regardless of HPV infection (Figure 2)12. Therefore, these findings suggest that multiple sexual partners being a potential independent risk factor for cervical cancer.
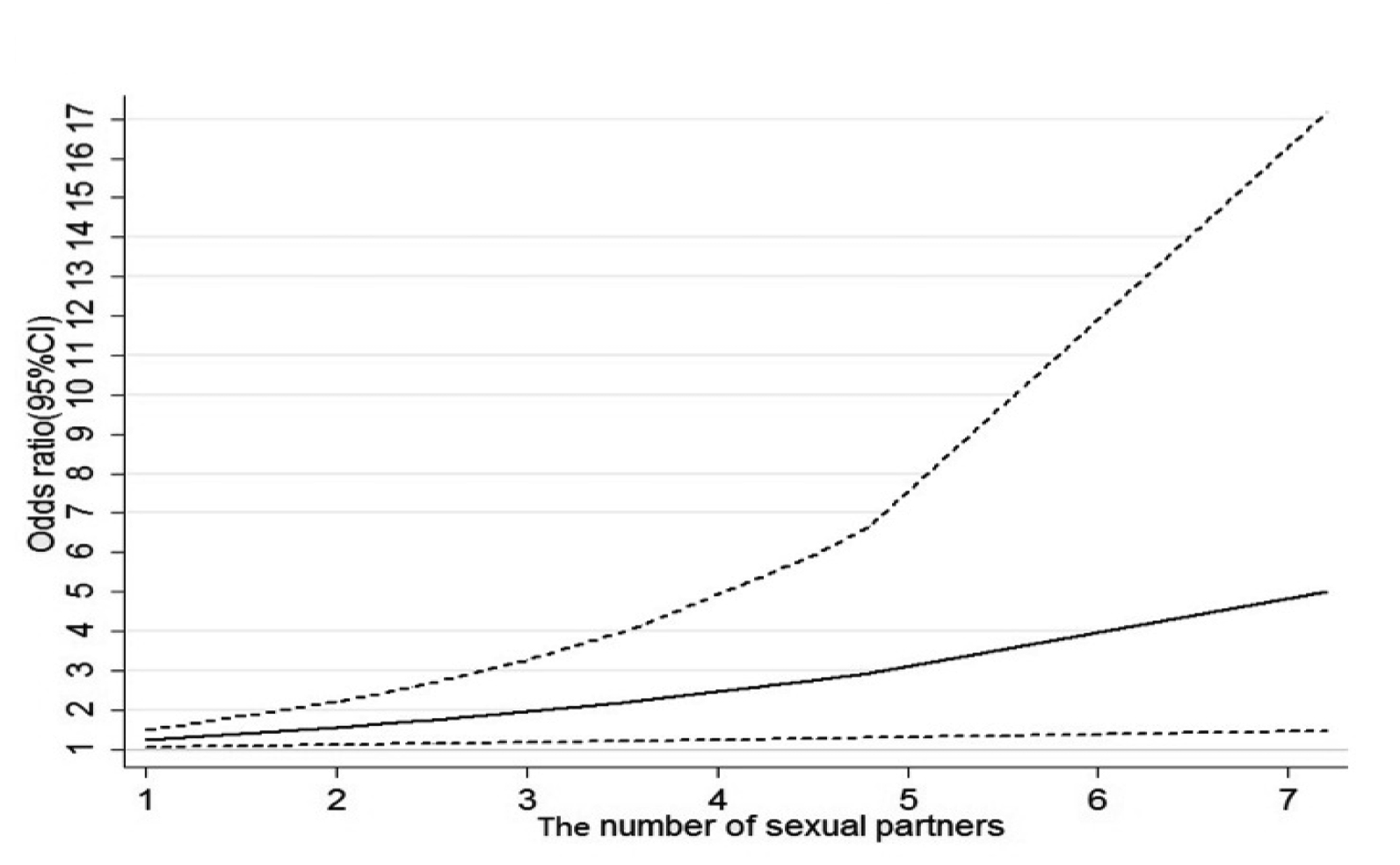
Figure 2. Combined relative risk of invasive cervical carcinoma after controlling for HPV infection12
Considering the disease burden among males and the potential risk of transmission to women, HPV infection in males is of clinical concern. Despite frequently overlooked, the lifetime risk of contracting HPV in males is comparable with that seen among females4. Dr. Tam reported that high-risk HPV infections are associated with various cancers seen in males, including anal, a subset of penile, and oral cancers, while low-risk HPV subtypes were associated with warts in the genital area or oral cavities. She added that the symptoms were dependent on the infection sites.
The HIM (HPV Infection in Men) Study is a prospective cohort study that provided an insight into the prevalence of HPV among males of different ethnicity and socioeconomic status. It compared the natural history of HPV in males from the United States, Mexico, and Brazil. Among the 4,292 men included, HPV infection was detected in 65.2% of participants, with 12% high-risk HPVs and multiple infections by both high-risk and low-risk HPVs in 17.8% of participants. HPV-16, 51, and 59 were the frequent high-risk HPV subtypes detected, while HPV-84, 62 and 6 were the most prevalent low-risk subtypes. Notably, the median time to clear any-HPV infection in males was 7.5 months, with 66% and 90% of infections clearing within 12 and 24 months, respectively13. Apart from the epidemiological data, the HIM study also addressed the relationship between HPV infection and clinical consequences in males, in addition to the associated risk factors at each anatomic site.
Due to the disease burden in both males and females, preventive measures against HPV infection are crucial. Vaccination is the first-line defence against HPV infection and related diseases. The Hong Kong College of Obstetricians and Gynaecologists (HKCOG) advocated that prophylactic HPV vaccines are the most effective in females with no prior exposure to the virus6. Nonetheless, vaccination after HPV exposure only protects in approximately 50–60% of cases14. Dr. Tam stated that HPV vaccination is currently recommended for females from the age of 915.
Currently, there are 3 types of HPV vaccines available locally: the bivalent against HPV-16/18, the quadrivalent against HPV-6/11/16/18, and the nonavalent against HPV-6/11/16/18/31/33/45/52/58. A recent nationwide study by Lei et al. (2020) involving health registers of 1,672,983 females in Sweden aged 10-30 demonstrated that the cumulative incidence of cervical cancer was 47 cases per 100,000 persons among females who were vaccinated and 94 cases per 100,000 persons among those who had not been vaccinated. The age-adjusted incidence rate ratio for the comparison of the vaccinated population with the unvaccinated population was 0.51. The results therefore confirmed that HPV vaccination is associated with a substantially reduced risk of invasive cervical cancer at the population level (Figure 3)16.
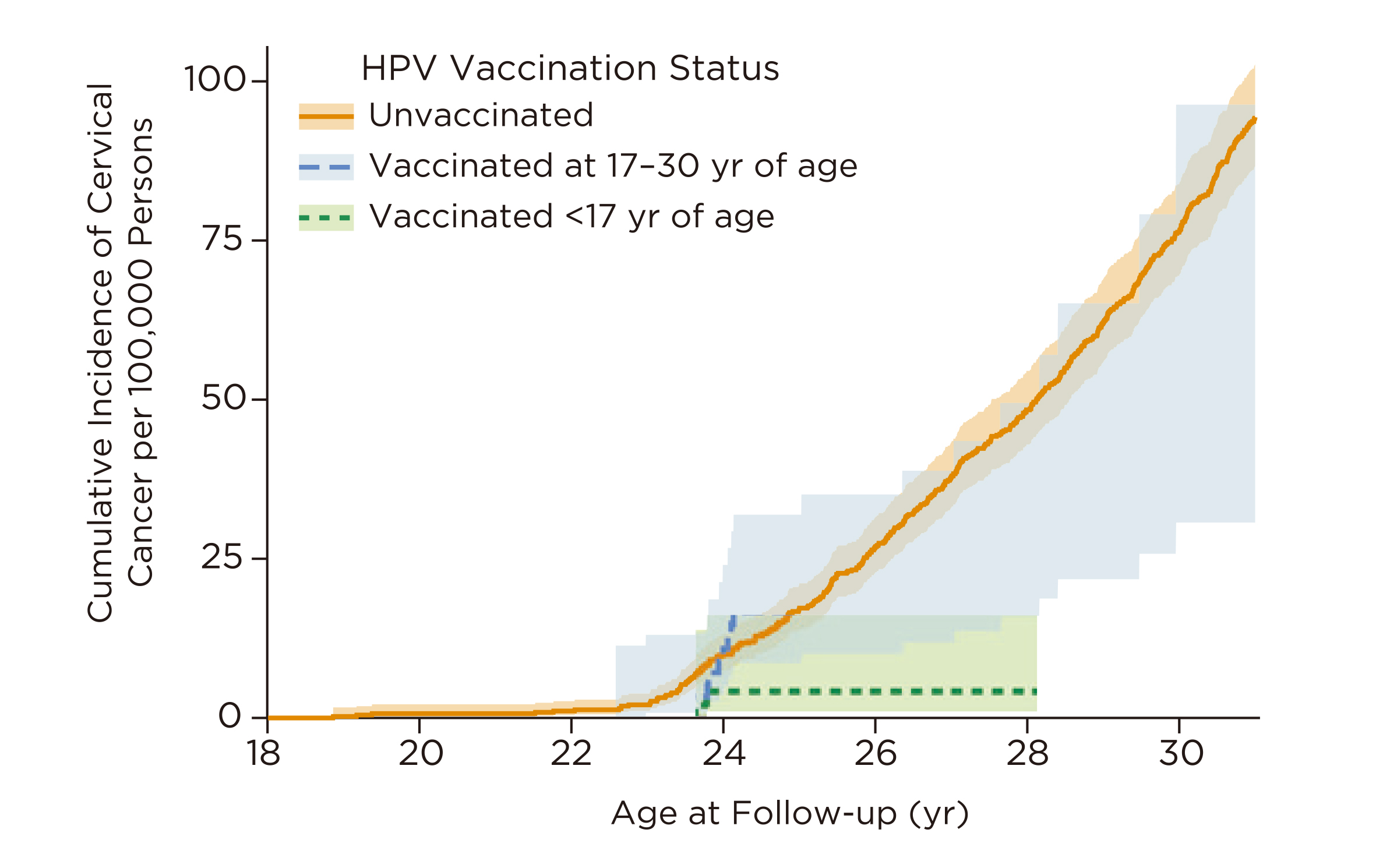
Figure 3. Cumulative incidence of invasive cervical cancer according to HPV vaccination status16
“HPV vaccines are safe in general. The side effects are mild, while the most common side effects include headache, dizziness, fatigue, and swelling at the injection site,” as per Dr. Tam. Furthermore, a recent report suggested that the quadrivalent HPV vaccine may reduce the incidence of external genital lesions and persistent infection with HPV 6/11/16/18 in males17.
Despite the promising efficacy, the suboptimal uptake of vaccines is still an issue since vaccine hesitancy remains a global clinical challenge in preventing HPV, and other diseases. Dr. Tam suggested that lack of awareness of the potential outcomes of HPV infection and the cost of vaccination may hinder the uptake of vaccines. “Since the implementation of the Hong Kong Childhood Immunisation Programme (HKCIP) from the 2019-20 school year, eligible female primary school students are provided with HPV vaccine18. The coverage of HPV vaccination is expected to increase,” according to Dr. Tam.
The underlying reasons discouraging HPV vaccination in local settings were visualised in the previous survey by Yuen et al. (2018), which involved 1,229 schoolgirls aged 9-14 and their parents. Among the respondents, those who decided not to vaccinate primarily concerned about the side effects and safety profile of the vaccine. In addition, parents who had never heard about the HPV vaccine were more reluctant to vaccinate their daughter19.
Interestingly, the survey also found that acquiring protection against cervical cancer and having a clinician recommendation are the major encouraging reasons for HPV vaccination uptake19. This highlighted the important roles of health education and promotion of HPV and its preventive measures. Furthermore, support from healthcare professionals in delivering healthcare information is essential. Dr. Tam suggested that active involvement in health talks and educating patients during consultation facilitate the dispersal of correct information regarding HPV and helps avoid misconceptions regarding the HPV vaccine.
Apart from vaccination, diagnostic screening forms a vital part of reducing the risk of cervical cancer. Cytology test (Pap smear) is the primary screening test available for cervical cancer. “It may take up to 10 years from HPV infection to cause cervical cancer, during which, precancerous changes can readily be picked up through regular cervical cytology,” as per Dr. Tam.
Even though cervical cytology is simple and effective, the subjective nature and relatively low sensitivity have prompted the development of better testing modalities with a higher sensitivity20. Therefore, HPV DNA testing and, more recently, HPV mRNA testing have been introduced. Both of these testing methods are more sensitive in detecting HPV than cervical cytology21,22. The cervical cytology has high specificity, up to over 98%, if they are performed well and have the ability to detect high-grade precancerous cervical intraepithelial neoplasia (CIN) and cancer according to Dr. Tam23. She highlighted that solely HPV DNA test might remain inconclusive in excluding high-grade CIN or cancers, therefore, a biopsy is often required. Notably, treatment is administered based on the stage of disease, but not when HPV DNA is detected. Thus, the co-test of cervical cytology and HPV DNA/mRNA test is a potential optimal tool for diagnostic purposes.
The availability of HPV tests allows individuals to perform the self-sampling test. A local survey by Wong et al. (2020) reported that respondents prefer HPV self-sampling tests to conventional screening. The results also suggested that HPV self-sampling test would enhance health awareness and promote the cervical cancer screening uptake rate, especially among the under-screened or never screened populations24. Dr. Tam noted that HPV self-sampling test may offer a convenient way for HPV detection and may also encourage medical advice-seeking among the high-risk population. Nonetheless, a clear and concise instruction by healthcare professionals on conducting the HPV self-sampling test is often required to avoid inaccurate or false negative results.
HPV is a common pathogen responsible for promoting carcinogenesis and other cutaneous and anogenital diseases in both males and females. The availability of effective vaccines and diagnostic tests makes HPV-related diseases largely preventable. However, further health education and promotion are essential to enhance public awareness and understanding of HPV infection. In conclusion, Dr. Tam advised that lifestyle interventions, including smoking cessation and safe sex practices, are essential in controlling the risk of acquiring HPV infection. For high-risk populations, particularly those who engage in unprotected sex, regular screening tests for HPV are highly recommended.
References
1. Szymonowicz et al. Cancer Biol Med 2020; 17: 864–78. 2. Centre for Health Protection - Cervical Cancer. https://www.chp.gov.hk/en/healthtopics/content/25/56.html. 3. World Health Organisation.Cervical cancer. 2022. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer. 4. Chesson et al. Sex Transm Dis 2014; 41: 660. 5. de Sanjosé et al. Best Pract Res Clin Obstet Gynaecol 2018; 47: 2–13. 6. HKCOG.Guidelines for Cervical Cancer Prevention and Screening. HKCOG Guidel No3 2016. 7. Pelullo et al. PLoS One 2012; 7. DOI:10.1371/JOURNAL.PONE.0042856. 8. Chidobem et al. Vaccines 2022, Vol 10, Page 604 2022; 10: 604. 9. Meites et al. Hum Vaccin Immunother 2022; 18. DOI:10.1080/21645515.2021.2016007. 10. Piróg et al. Diagnostics 2022, Vol 12, Page 843 2022; 12: 843. 11. Xi et al. Cancer Epidemiol Biomarkers Prev 2009; 18: 3490. 12. Liu et al. Asian Pac J Cancer Prev 2015; 16: 3893–900. 13. Sichero et al. Acta Cytol 2019; 63: 109–17. 14. Cheng et al. Vaccines 2020; 8: 1–15. 15. WHO updates recommendations on HPV vaccination schedule. https://www.who.int/news/item/20-12-2022-WHO-updates-recommendations-on-HPV-vaccination-schedule. 16. Lei et al. N Engl J Med 2020; 383: 1340–8. 17. Kamolratanakul et al. Vaccines 2021; 9. DOI:10.3390/VACCINES9121413. 18. Centre for Health Protection - About human papillomavirus (HPV) vaccination. https://www.chp.gov.hk/en/features/102146.html. 19. Yuen et al. PLoS One 2018; 13. DOI:10.1371/JOURNAL.PONE.0194159. 20. McGraw et al. World J Clin Oncol 2014; 5: 744. 21. Ratnam et al. J Clin Microbiol 2010; 48: 2779. 22. Dockter et al. J Clin Virol 2009; 45 Suppl 1. DOI:10.1016/S1386-6532(09)70009-5. 23. Pankaj et al. Indian J Gynecol Oncol 2018 163 2018; 16: 1–5. 24. Wong et al. Int J Environ Res Public Health 2020; 17: 1–15.





