
President of International Society of Renal Nutrition and Metabolism (ISRNM)

President of International Federation of
Kidney Foundations -
World Kidney Alliance (IFKF-WKA)
The Time is Now Reconsideration on Dietary Intervention in CKD
Chronic kidney disease (CKD) affects about 10% of global population with an increasing prevalence1, and the CKD burden in Hong Kong is expected to be high. Undoubtedly, adherence to healthy diets is an important measure in the management of CKD and is recommended by international guidelines. Particularly, protein restriction has been recommended for CKD patients, but the compliance to the recommended diet is low in reality. Thus, reconsideration on the recommendations on dietary intervention and the approach for delivering kidney health information to CKD patients is urgently needed. In a recent interview, Dr. Lui Siu Fai, President of International Federation of Kidney Foundations - World Kidney Alliance (IFKF-WKA), and Dr. Wang Yee Moon Angela, President of the International Society of Renal Nutrition and Metabolism, shared their expertise on dietary intervention for patients with kidney diseases and discussed the essence of health literacy as well as its significance in improving clinical dietary advices.
The Impact of High-protein Diet on Renal Function
Ahigh consumption of proteins could be detrimental to kidney function through several mechanisms. Dr. Wang addressed that high dietary protein intake may lead to afferent arteriole vasodilatation and efferent arteriole vasoconstriction resulting in an increased intra-glomerular pressure and glomerular hyperfiltration, which in the long-term can lead to de novo or aggravating pre-existing CKD. Briefly, glomerular hyperfiltration would stimulate mesangial cell signaling to increase the level of transforming growth factor-ß (TGF-ß), which subsequently contributes to the progression of kidney fibrosis. Besides, protein-rich foods contain high levels of advanced glycation end products (AGEs), which would impair protein degradation leading to basement membrane thickening and mesangial expansion in glomerulus of diabetic kidney disease (DKD). Notably, the pathogenic response of AGEs could be mediated with the proinflammatory receptor for AGE (RAGE) presented on glomerular cells, whereas RAGE activated signals culminating in cellular inflammation and death(Figure 1)2. Dr. Wang emphasised that the impacts of high-protein diet are not limited solely in the glomeruli. “There are research works suggesting that high-protein diet increases the risk of inflammation in kidney, and diseases such as hypertension,” she noted.
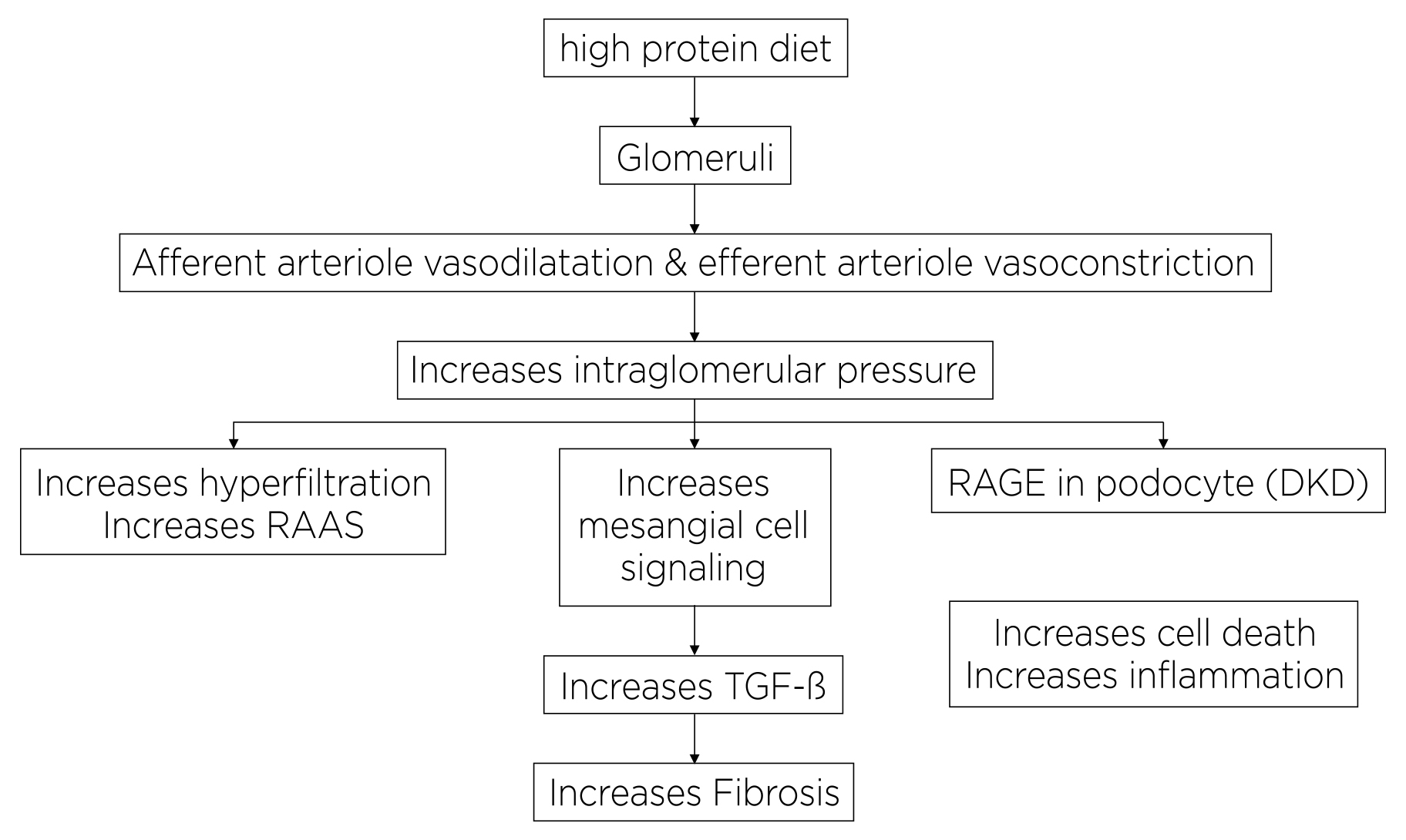
Figure 1. Possible mechanisms of high dietary protein intake on kidney health2, RAAS: renin-angiotensin-aldosterone system4
Low-protein Equals Renoprotective?
Low-protein diet has been suggested to provide many advantages in the management of CKD patients by reducing nitrogen waste products and decreasing kidney workload through lowering intra-glomerular pressure. Low-protein diet is also reported to induce favorable metabolic effects that can preserve kidney function and help to control uremic symptom3.
The Modification of Diet in Renal Disease (MDRD) study is considered the largest randomised control trials (RCT), involving 840 patients with various chronic renal diseases, investigating the impacts of restricting protein intake and controlling hypertension on the progression of renal disease.
In the MDRD study, a slower decline in renal function started four months after the introduction of a low-protein diet was observed among patients with moderate renal insufficiency as compared to the usual-protein group (Figure 2). However, the result indicated that a very-low-protein diet did not significantly slow the progression of renal disease among patients with more severe renal insufficiency as compared to a low-protein diet4.
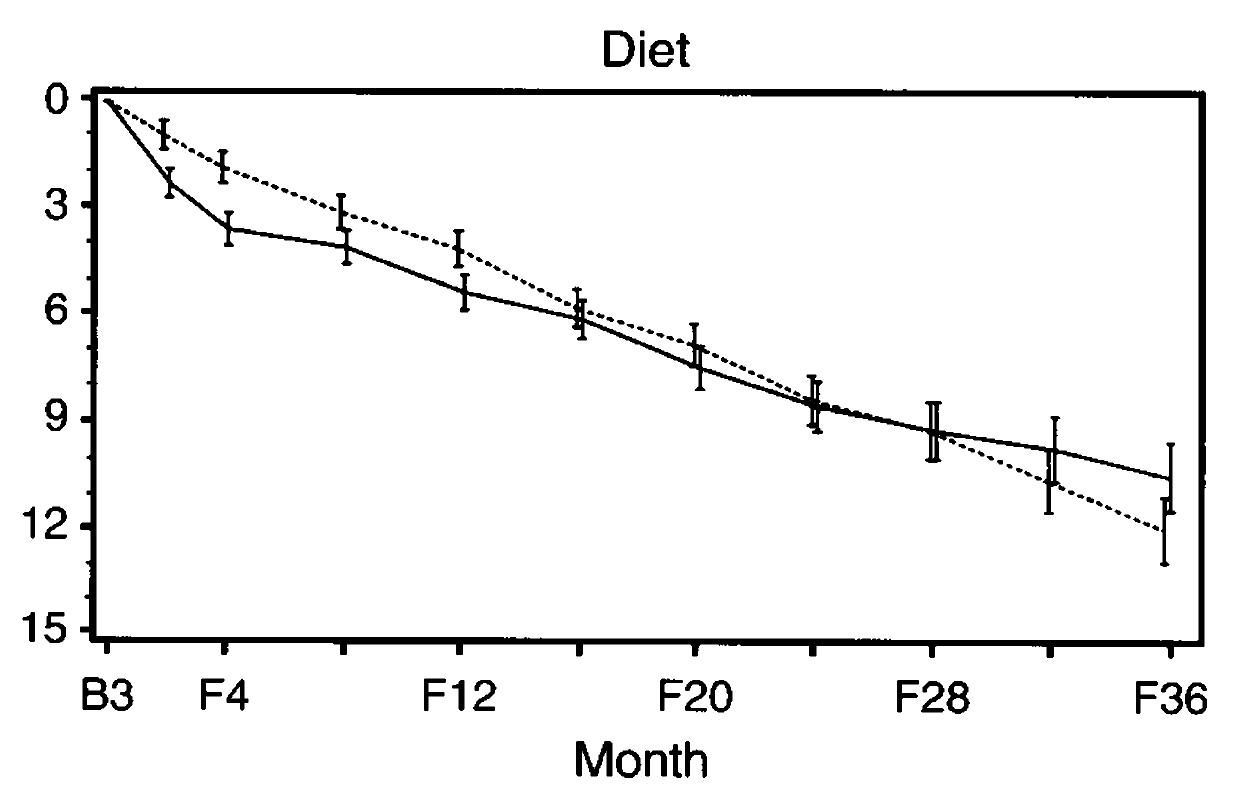
Figure 2. Estimated mean decline in the glomerular filtration rate from base line (B) to selected follow-up times (F)4, dashed line: usual-protein diet; solid line: low-protein diet
In view of the benefits demonstrated, a low-protein diet (0.55-0.6g protein/kg bw/day) is recommended in the Kidney Disease Improving Global Outcomes (KDIGO) Guideline for adults with stage 3-5 CKD who are metabolically stable. Notably, the Guideline also addresses the very-low-protein diet (0.28-0.43g protein/kg bw/day) with additional keto acid/amino acid analogs3.
Dr. Wang highlighted 2 issues about the recommendations. Firstly, the numeric value of “0.55-0.6g protein/kg bw/day” can merely be a reference value for dietitians but difficult to be applied by patients in real life. “It is difficult to tell how much meat should actually be eaten based on the values,” she expressed. Besides, she also doubted that how many patients can really comply with the recommendations, especially the very-low-protein diet.
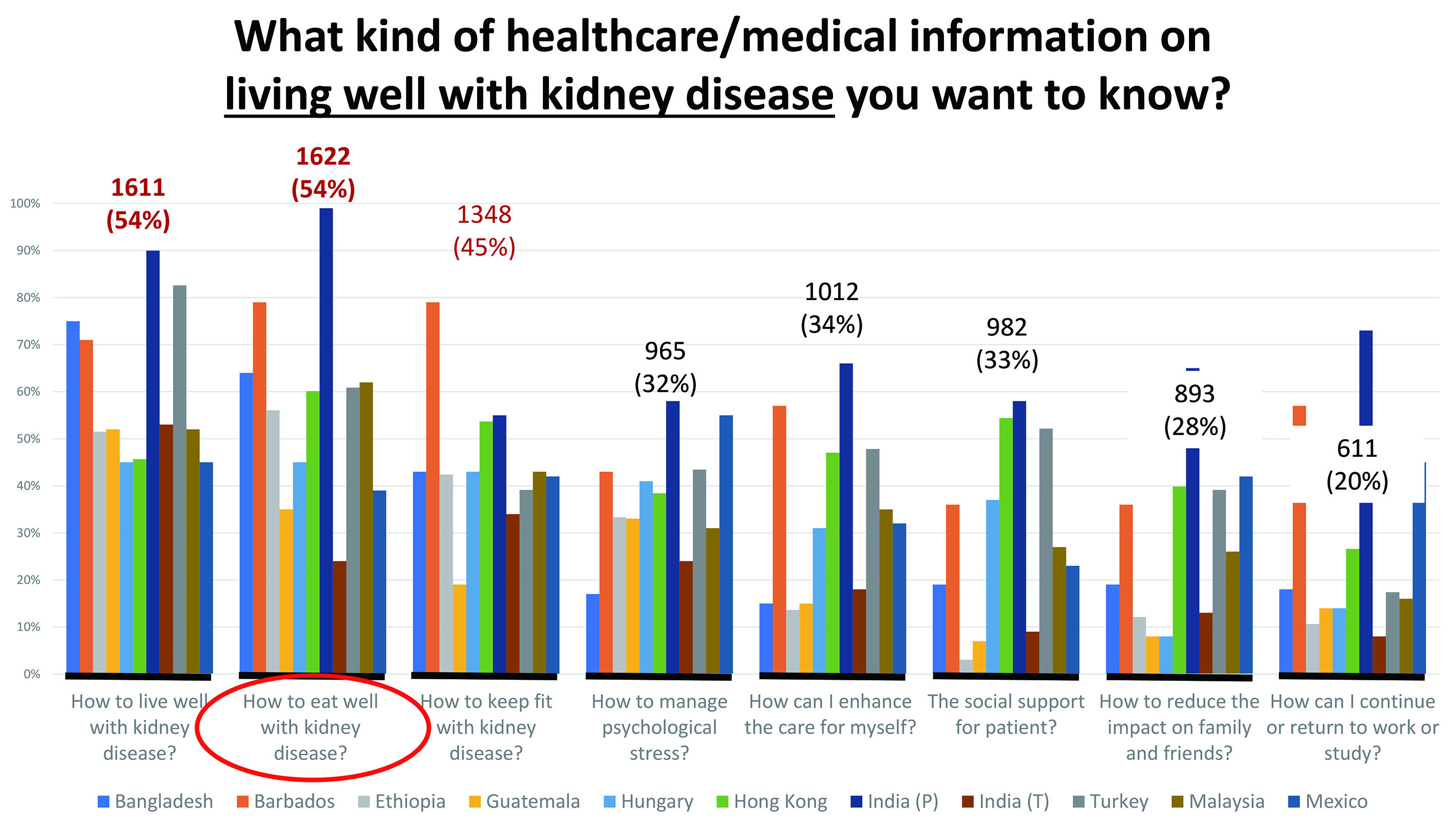
Figure 3. Key healthcare/medical concerns among patients with kidney diseases (data provided by Dr. Lui)
Healthy Dietary Pattern Matters
Apart from the amount of protein intake, Dr. Wang emphasised the importance of adopting a healthy dietary pattern. She noted that current clinical recommendations tend to take patients’ outcomes, quality of life, and sense of wellbeing into account instead of focusing on the dietary restriction on a single nutrient.
Dr. Wang advised to intake more vegetables and fruits and less meats, especially the processed ones. Indeed, the benefits associated with vegetables and fruits have been reported extensively. While metabolic acidosis in CKD is aggravated by the high consumption of meat and refined cereals, increasing the dietary acid load, the intake of fruits and vegetables is able to neutralize the acidosis and its deleterious consequences5. However, based on Dr. Wang’s observation, more than 50% of patients in her clinic have not taken enough plant-based proteins with health benefits, but having too much processed meat.
On the other hand, Dr. Wang reminded to notice the patients’ salt intake. Remarkably, she highlighted that high dietary potassium is associated with a decrease in blood pressure, particularly in the presence of a high-sodium diet6.
“Allowing patients to living well with kidney diseases is essential, while the key point is to adopt a healthy dietary pattern,” Dr. Wang said. She stressed that the healthy dietary pattern has to be adopted as soon as possible, but not after diagnosis of kidney disease is documented.
The Role of Health Literacy
Recently, the IFKF-WKA conducted an online survey among patients with kidney diseases worldwide, the results revealed that the information on how to eat well with kidney diseases is a core concern for the participants (Figure 3).
Dr. Lui further addressed that healthcare professionals are a trusted source of healthcare information for the patients. Therefore, he noted that it is the responsibility of healthcare professionals to facilitate patients to find the right information at the right platform in the right format. Of importance, the information has to be understandable for patients. This highlights the essence of improving health literacy, which refers to the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions7.
Apart from individual health literacy, organisational health literacy defines the role of healthcare organisations in making health information and services easy to understand and access8. In this regard, the “Kidneys Talk” webinar series, which aim to provide information on kidney health and treatment options and healthy diets for CKD patients have been launched in 2021. The webinar series are broadcasted at various online and mass media platforms.
Making Sense of Renal Dietary Advice With the right information and platforms, the healthcare information has to be in the right format which is understandable and, more importantly, applicable for patients. In the context of renal dietary advice, Dr. Lui emphasised that the information has to be simple and layman. “The prerequisite to use the refined dietary intervention (the “World Kidney Recipes”) is the patients’ basic knowledge of nutrition and diet for kidney disease. They also need to be aware of their own condition,” Dr. Lui addressed. When using the World Kidney Recipes, patients are expected to amend their own recipes to meet their recommended dietary requirements.
Translating the scientific data into applicable information is essential for allowing the patients to follow the dietary recommendations. Dr. Lui commented that the numeric data in traditional dietary recommendation would be rather confusing. Hence, he proposed to classify the levels of nutrients with indicators such as “high”, “medium”, and “low” in addition to numeric values. He added that the indicator is only a relative measure that needs to take into account the patient’s conditions, such as body weight and biochemistry and stage of kidney failure.
Moreover, Dr. Lui suggested the use of exchange portions in designing the recipes. For instance, 1 exchange portion denotes 7g of protein, which also denotes 15g of carbohydrates. Practically, patients do not need to have a different recipe for different stages of kidney failure, or renal replacement therapy, but to modify the recipe, such as the portion size, according to the advices of healthcare professionals.
Bring the Joy Back into Eating V The World Kidney Recipes The main goal of the of World Kidney Recipes is to galvanise patients and their care partners to work with gastronomic experts and dietetic professionals, including chefs and dietitians, to inspire creativity in culinary medicine and medical nutrition therapy in kidney care. Practically, it is to translate the dietary recommendations into day-to-day practice for patients with kidney diseases. In the process, the role of dietitians is crucial that they help modifying the recipes to be suitable for kidney patients (Figure 4).
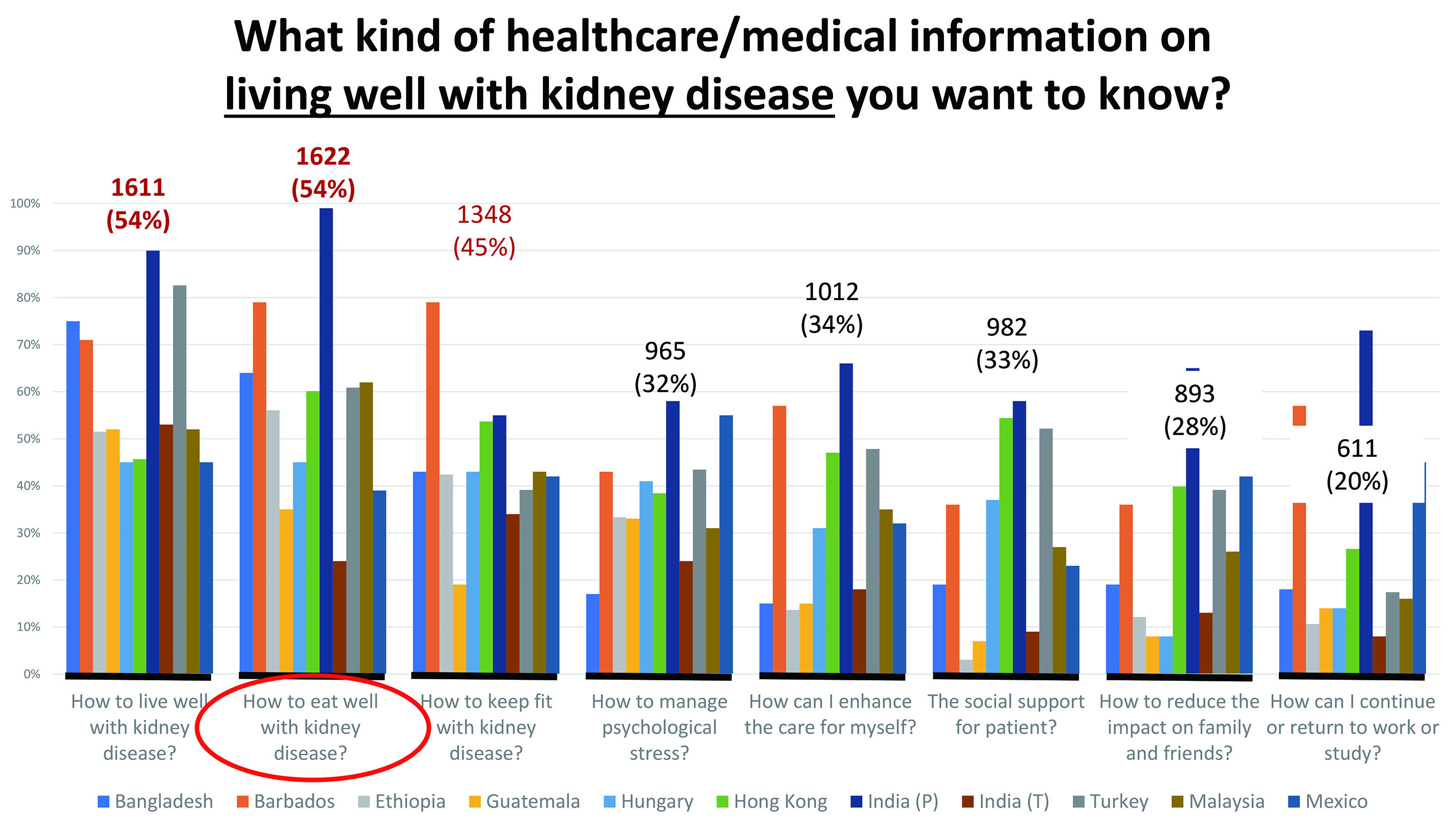
Figure 4. Modified recipe by dietitians for kidney patients (information provided by Dr. Lui)
“We aim to help them to fish, rather than give them the fish,” Dr. Lui addressed. Hence, the involvement of patients in the development of the World Kidney Recipes is crucial. Upon improving health literacy, the patients are expected to have basic knowledge on diet and nutrition and their health conditions. Hence, they can decide the number of portions for each meal in accordance with the recommended number of portions. Remarkably, in cases the patients take some food elements in excess in a meal, they can make adjustment in the next meal. This hence enhances the flexibility for patients in meal planning.
An example of World Kidney Recipes is shown in Figure 5. Apart from ingredients and preparation procedures, patients can find information on the expected exchange portions consumed from this dish. Each recipe is labeled with indicators coupled with the actual amount of food elements, such as low sodium and low phosphorus. Essentially, the recipe also highlights which food elements may be in excess, potassium in this recipe (highlighted in yellow). A remarkable feature of the World Kidney Recipes is the inclusion of tips on cooking skills (in the green box), which helps improving health outcomes and matching with patients’ preferences.
Eat Smart, Eat Well
Dr. Lui emphasised that it is not a one-step process to get to “eat smart, eat well” for kidney patients. “Continuous enhancement of the World Kidney Recipes is needed to make it more user-friendly, to provide more tips, to include new smarter ways of cooking,” he noted. However, there are still challenges for the World Kidney Recipes. Firstly, Dr. Lui highlighted that there is currently no consensus in the standard of “high” and “low” globally, whereas the working group of World Kidney Recipes adopted the Australian standard. On the other hand, the current recipes focus on home cooking, but the case of dining out is not included. The amount of food elements consumed when dining out may be difficult to be estimated and control, but it is crucial for the patients to aware on the food contents they intake.
In summary, Dr. Lui commented that a balance between nutrition requirements and protecting kidney functions has to be established. The key issue is to empower the patients to choose the appropriate food and to prepare and serve them correctly, based on the recommendations of healthcare professionals. As addressed by Dr. Wang, to slow down kidney failure, dietary pattern definitely has a vital role. She stressed that maintaining the appropriate balance between plant-based protein and meat-based protein is essential. In reality, the restrictive diet adversely impact the quality of life for kidney patients, thus a change from restrictive diet to modified diets is needed to improve compliance and health outcomes. Finally, Dr. Wang concluded with the name of a nutritional education program for CKD patients that kidney patients should “eat like a rainbow”.
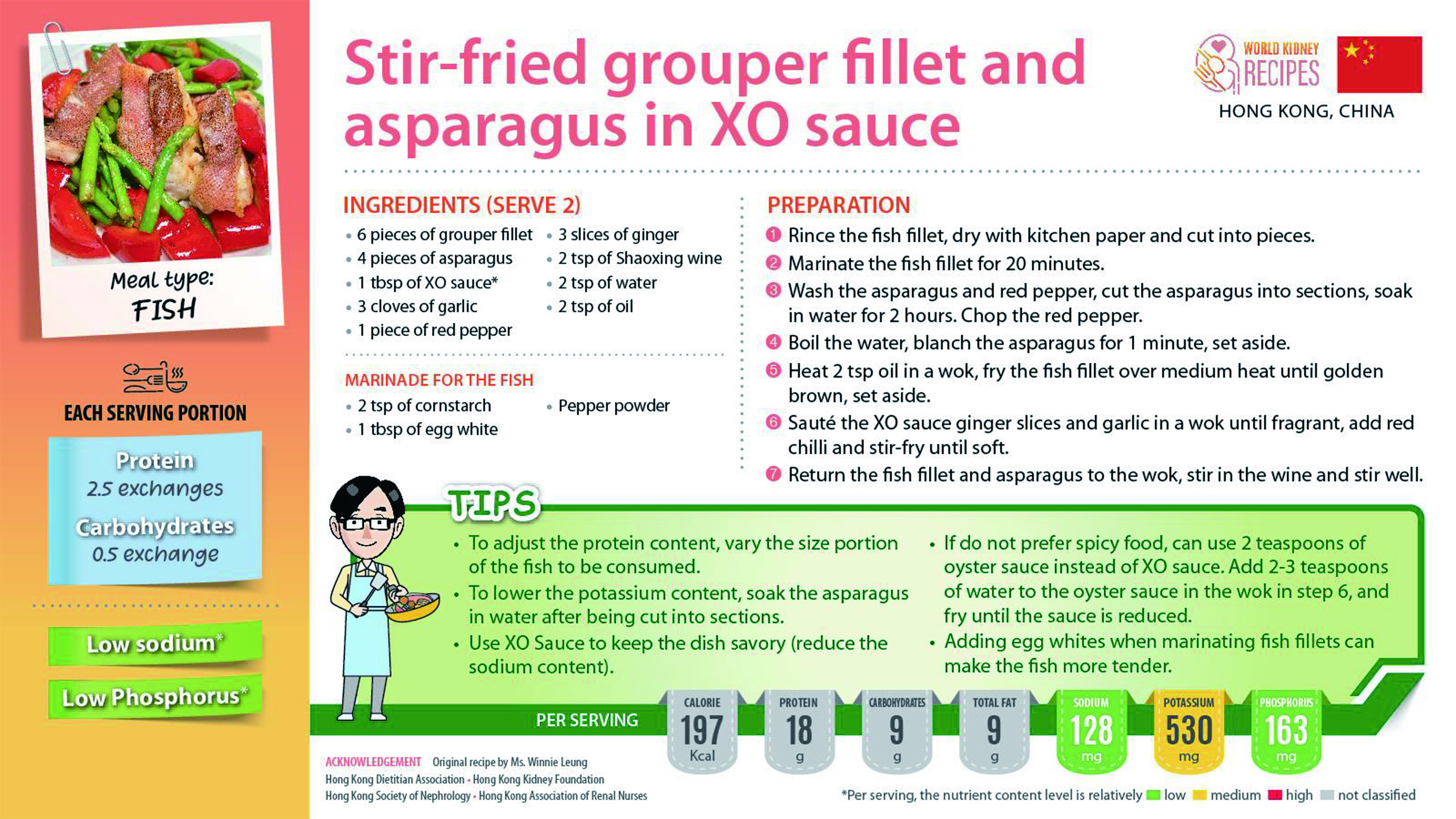
Figure 5. The World Kidney Recipes (information provided by Dr. Lui)
References
1. Sever et al. Clin Kidney J 2021; 14: 23-V35. 2. Ko et al. Am J Kidney Dis 2020; 76: S1-V107. 4. Klahr et al. N Engl J Med 1994; 330: 877-V84. 5. Cases et al. Nutrients 2019; 11. DOI:10.3390/NU11061263. 6. Staruschenko et al. Hypertension 2018; 71: 1015-V22. 7. Boonstra et al. Nephrol Dial Transplant 2021; 36: 1207-V21. 8. Brega et al. Heal Lit Res Pract 2019; 3: e127.





