

Department of Medicine & Geriatrics
Tuen Mun Hospital
The advancement in novel therapies for multiple myeloma (MM) has significantly improved the outcomes of patients with newly diagnosed MM (NDMM) or relapsed/refractory MM (RRMM)1. Whereas, inducing an objective response with a prolongation of survival and to improve the quality of life of patients with RRMM is still challenging in clinical practice. To visualise the practical problems faced by both frontline physicians and their MM patients, Dr. Justin Li shared the case of his patient who had a long fight with the disease.
Disease Presentations
The patient was a gentleman aged 62 at the time of diagnosis. He was a retired lorry driver with smoking and drinking habit previously. The patient had been diagnosed with GOLD stage II chronic obstructive pulmonary disease (COPD), mild-to-moderate obstructive sleep apnoea (OSA), knee osteoarthritis, gastroesophageal reflux disease (GERD), and colonic polyps.
The patient was presented to Dr. Li’s clinic for a viral skin rash and mild exacerbation of COPD in July 2013. He was incidentally found to have macrocytic anaemia with leukopenia. Upon admission, the haemoglobin was 11.4 and a total white cell count (WCC) was 2.8 while the platelet count was normal. The peripheral plasma did not show any abnormal cells, except macrocytosis and mild poikilocytosis. The lactic dehydrogenase (LDH) level was elevated to 480. There was no lymphadenopathy or hepatosplenomegaly found.
In view of the persistent unexplained microsite macrocytic anaemia, bone marrow examination was conducted in October 2013, which showed an increase in plasma cells at 18% in the aspirate. The refined biopsy showed features consistent with plasma cell myeloma with prominently increased plasma cells with clusters up to 70% with proper light chain restriction. The free kappa light chain (FLC) level was markedly elevated at 3108 mg/L with a kappa/lambda (K/L) ratio of 388. Skeletal survey revealed wedge collapse of the L1 vertebral body, whereas subsequent MRI showed a marrow infiltration by the myeloma with partial collapse in one lumbar vertebra. The diagnosis of ISS Stage II Kappa light chain myeloma with bone involvement was documented.
Initial Treatment Protocol
The patient was prescribed with bortezomib, thalidomide, and dexamethasone (VTD) in January 2014 and pamidronate was provided for the myeloma bone disease. After 4 cycles of VTD, the FLC level was significantly decreased from 3100 mg/L to about 300 mg/L in March 2014. The patient tolerated VTD treatment well except one episode of COPD exacerbation, resulting in the truncation of one of the treatment cycles. The patient declined autologous stem cell transplantation (ASCT) due to his underlying chronic chest condition. Hence, Dr. Li stepped down the treatment to thalidomide and dexamethasone (TD) for 2 cycles since April 2014. However, a mild progressive rise in FLC was observed again. Thus, VTD was resumed in July 2014 for another 5 cycles till December 2014. During the treatment, very good partial remission (VGPR) was achieved with 93.6% reduction of the FLC down to around 200 mg/L. Nonetheless, the treatment was complicated by another episode of COPD exacerbation in July 2014 but it was uneventful. The patient was then put on thalidomide maintenance since December 2014 (Figure 1).

Figure 1. Reduction in FLC upon VTD therapy
Disease Progression and Treatment Strategy
In March 2015, the patient visited Dr. Li’s clinic and complained on an increasing low back pain for one month. Blood test indicated an increase in FLC to around 500 mg/L. Dr. Li thus prescribed Rd with bortezomib (VRD) as salvage treatment since April 2015. 11 cycles of VRD treatment was provided till January 2016, the patient ran out of funding for lenalidomide treatment thereafter.
In view of the patient’s financial constraint, Dr. Li decided to step down the treatment to 4 cycles of VTD. Luckily, the funding issue was later resolved and VRD therapy was hence resumed. Totally, the patient completed 25 cycles of VRD. The treatment was complicated with COPD exacerbation and one episode of transient ischemic attack (TIA), whereas the best response achieved with this regimen was partial response (PR) (Figure 2).

Figure 2. Change in FLC upon VRD therapy
Tackling the Second Relapse
In late April 2017, the patient’s free kappa level increased up to 200 mg/L. Dr. Li switched the treatment to bortezomib, cyclophosphamide and dexamethasone (VCD) regimen in June 2017. However, the free kappa level continued to increase upon 4 cycles of VCD till September 2017. In October 2017, the patient received a subsidy funding for pomalidomide and thus 9 cycles of Pd therapy was given till June 2018. The best response achieved with Pd regimen was PR (Figure 3).

Figure 3. Change in FLC upon Pd therapy
The Third Relapse and Complications
The Pd treatment was again complicated with COPD exacerbation and an episode of right leg cellulitis. In June 2018, the patient was admitted to the hospital for pneumonia with chest X-ray showing left lower zone consolidation. Later, mycobacterium avium complex infection was confirmed. Therefore, the Pd therapy was withheld in view of the active infection. A high resolution CT showed emphysematous changes, some non-specific lung nodules and some small calcified granulomatous in the right lung apex and also the left lateral lung base likely due to previous infection. With the advices from respiratory physicians and the microbiology team, azithromycin, ethambutol and rifampicin (MAC) therapy were prescribed. Pd therapy was resumed in August 2018, when the free kappa level had increased to over 1,000 mg/L. Although some responses to Pd therapy were obtained, only stable disease could be retained despite 9 more cycles of Pd were prescribed (Figure 4).
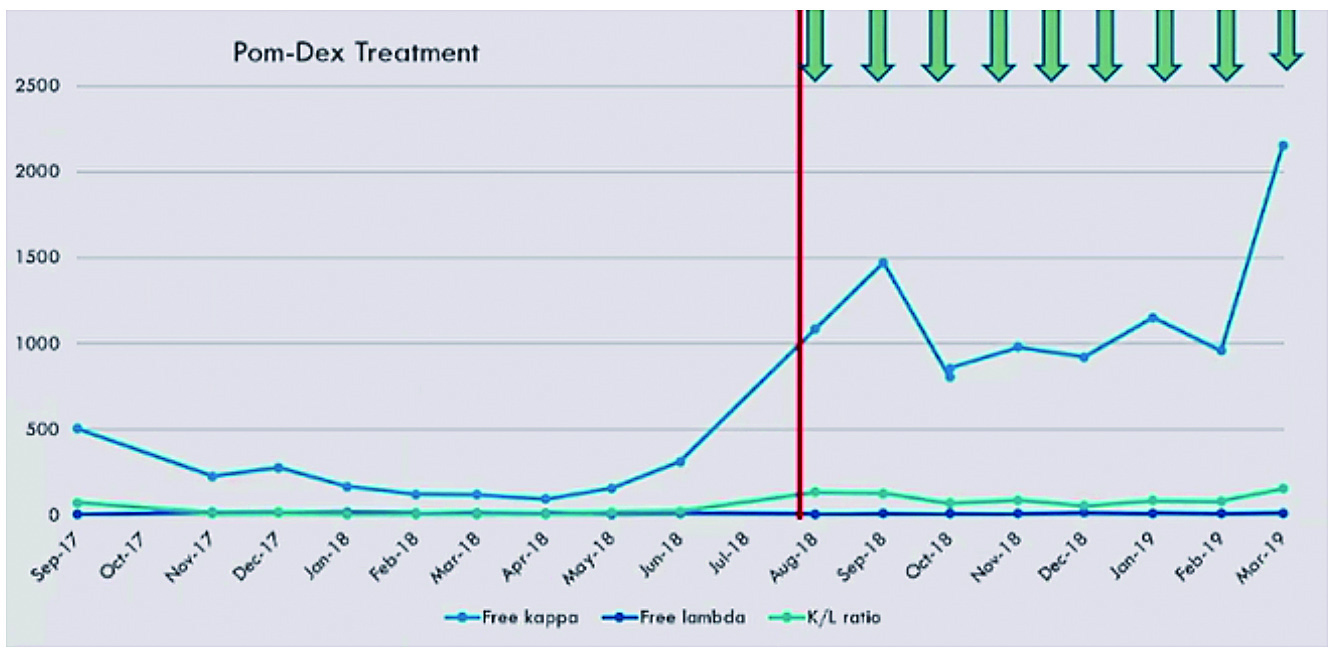
Figure 4. Change in FLC upon resuming Pd therapy
Besides, neutropenia and thrombocytopenia were noted, with the lowest absolute neutrophil count (ANC) of 0.4 and a platelet count of 76. G-CSF injection was required to support his neutrophil counts throughout the treatment process. Repeated bone marrow examination in November 2018 revealed persistent MM. As there was a free drug programme available, the patient opted to try ixazomib-based treatment (ITD) since April 2019.
Countering the Relapsed Disease
Totally, 15 cycles of ITD therapy were prescribed till June 2020 achieving stable disease (Figure 5). While the MAC treatment was completed in July 2019, the patient was complicated with another episode of COPD exacerbation in January 2020 and thus MAC treatment was restarted in February 2020.
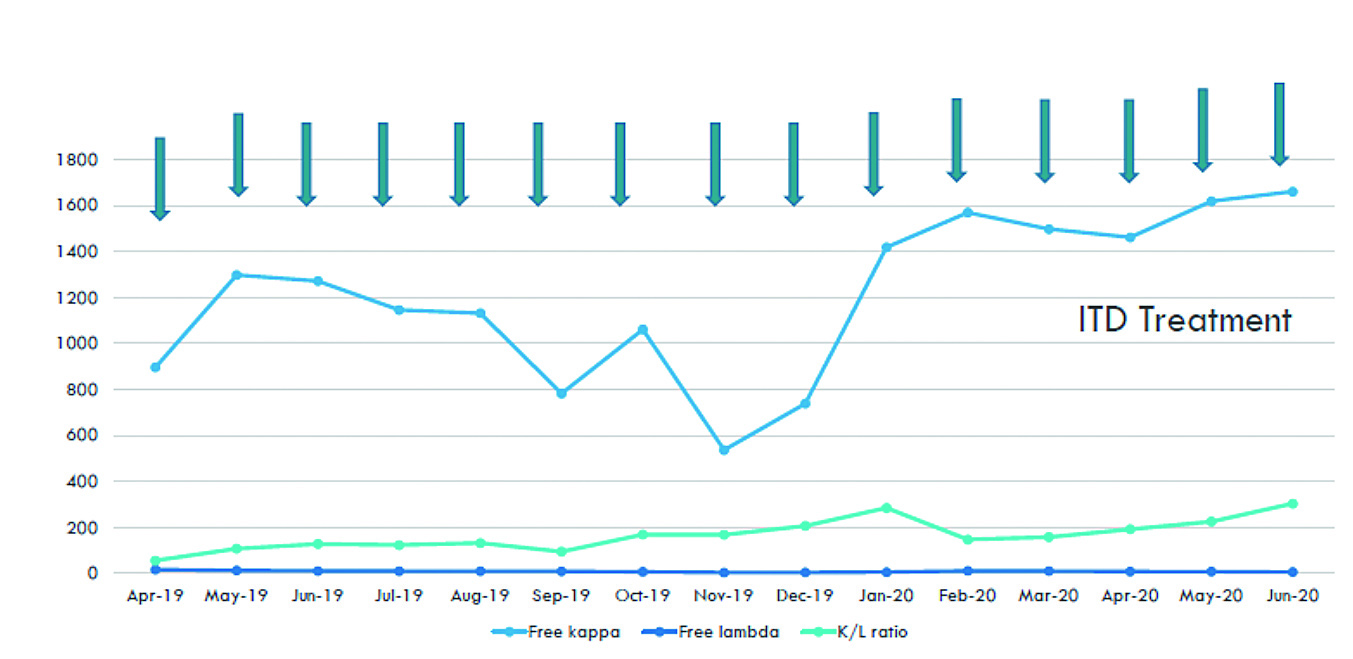
Figure 5. Change in FLC upon ITD therapy
In June 2020, the patient complained for ribs pain. Also, deteriorating haemoglobin and platelet counts were noted and thus repeated blood transfusion was provided. Although the kappa level remained static, the K/L ratio was found increasing. In considering the patient’s funding, carfilzomib plus melphalan and prednisone (KMP) therapy was the only option available. 4 cycles of KMP therapy were given since June 2020 till December 2020 and PR was achieved (Figure 6).

Figure 6. Change in FLC upon KMP therapy
In December 2020, a compassionate programme for daratumumab was available. Hence, daratumumab plus carfilzomib and dexamethasone (DKd) therapy was prescribed. In the first cycle of daratumumab infusion, the patient experienced adverse events but the symptoms were manageable. The patient subsequently tolerated the therapy and 14 cycles of DKd were treated until January 2022. PR was achieved by the DKd therapy (Figure 7). The free kappa level was improved for a few months but increased again since September 2021. The patient declined the suggested CAR-T therapy due to financial reason. Given another funding programme was approved, daratumumab plus pomalidomide and dexamethasone (DPd) therapy was prescribed since January 2022 and the patient was able to remain stable disease.

Figure 7. Change in FLC upon DRd therapy
In March 2022, the patient was admitted to hospital for neutropenic fever with pneumonia. Unfortunately, the patient was infected with COVID-19 during hospital stay and had developed progressive respiratory failure requiring high flow oxygen support as well as COVID-19 treatment. His chest condition was gradually improved, but long term oxygen therapy was required. The patient had developed progressive cytopenia and repeated blood transfusion was needed. Flow cytometry further confirmed the development of plasma cell leukaemia. The patient eventually agreed for palliative care and supportive blood transfusion. At the time of report, the patient was trying on traditional Chinese medication.
Concluding Remark
Dr. Li presented the management of RRMM with multiple lines of therapies across 9 years, which was undoubtedly a long treatment journey. During the course of treatment, the practical challenges encountered by physicians in deciding the optimal therapy at various stages of the disease were visualised. Dr. Li concluded, in addition to the combinations of therapies, more factors such as the patient’s physical condition, the response to prior line of treatments, underlying cytogenetic features as well as the financial aspects have to be taken into account in deciding the salvage regimen.
References
1. RichardsonPG, LaubachJ, GandolfiS, FaconT, WeiselK, O-¦GormanP.Maintenance and continuous therapy for multiple myeloma. Expert Rev. Anticancer Ther.2018; 18: 751-V64.





