

Specialist in Infectious Disease
MBBS(HK), FRCP (Lond),
FRCP (Edin), FFPH (UK),
FHKCP, FHKAM (Medicine),
MPH (Johns Hopkins) MSc Infect Disease LSTMH (Lond), Dip G-U M (LAS), DTM&H (Lond), PGDipClinDermat (QMUL)
Honorary Consultant, Infectious Disease Centre & Department of Medicine & Geriatrics,
Pandemic in Pandemic – The Impacts of COVID-19 in People Living with HIV
The ongoing COVID-19 pandemic has posed a great challenge on HIV/AIDS prevention and patients’ care. Healthcare professionals, related organisations and people living with HIV (PLWH) have to fight against two pandemics at the same time. Similar to comorbidities such as malignancy, obesity and diabetes, PLWH has been reported to have higher risk of developing severe form of COVID-19 infection when infected by the virus1. Besides, the implementation of quarantine, social distancing and community containment measures have severely disrupted HIV/AIDS-related services in different aspects2. To uncover the impacts of the COVID-19 pandemic on PLWH in local settings, Dr. Wong Tin Yau Andrew, Specialist in Infectious Disease, shared his experiences and opinions on clinical care for PLWH in the current pandemic.
The Risk of COVID-19 Infection among PLWH
PLWH are unique due to their altered immune system from their history of chronic HIV infection and their use of antiretroviral therapy (ART). However, Dr. Wong noted that the risk of infection by SARS-Cov-2, the virus that causes COVID-19, depends on one’s exposure to the virus regardless of HIV status. In reality, there are some PLWH at the 3 local designated HIV Clinics reported to have been infected by COVID-19. Local clinical data on the number of COVID-19 infection among PLWH are currently not available. According to the systematic review by Barbera et al (2021) involving 212 articles, no increased risk for SARS-CoV-2 infection was found among PLWH. Although some reports suggested an increased risk of COVID-19 infection in PLWH compared with those without HIV, the observations can be explained by the occurrence of numerous confounders3. Given the inconsistent protocols in data collection and analyses, the findings in previous investigations evaluating the risk of COVID-19 infection among PLWH were inconclusive3.
When SARS-Cov-2 Meets HIV
The World Health Organization (WHO) confirmed that HIV infection is a significant independent risk factor for both severe COVID-19 presentation at hospital admission and in-hospital mortality4. Most of the existing reports suggest that PLWH may be at increased risk of severe SARS-CoV-2 mediated disease complication due to functional impairment of the immune system and persistent inflammation, which can be ameliorated by antiretroviral therapy5. For instance, a recent meta-analysis by Danwang et al (2022), which included 44 studies accounting for 38,971,065 patients with COVID-19, indicated that HIV-positive individuals were more likely to be admitted to hospital compared to HIV-negative individuals (odds ratio [OR]: 1.49, 95% confidence interval [CI]: 1.01–2.21)1. Moreover, Bhaskaran et al (2020) reported that PLWH had higher risk of COVID-19 death than those without HIV after adjusting for age and sex (hazard ratio [HR]: 2.90, p <0.0001, Figure 1)6. Nonetheless, there have been conflicting findings on the impacts of COVID-19 in PLWH reported. A local case series study by Ng et al (2022) on PLWH hospitalised with SARS-CoV-2 infection demonstrated that HIV patients had a similar respiratory shedding profile compared to HIV-negative controls, but with decrease in IL-10 and NT-proBNP7. Practically, Dr. Wong mentioned that most of the PLWH who are virologically suppressed and infected with SARS-CoV-2 showed mild symptoms.
To illustrate the outcomes of a severe case of co-infection by both HIV and SARS-CoV-2, Dr. Wong shared the case of a male patient. The patient was in his 70s complained of respiratory distress on admission. He had history of pulmonary embolismand was on anticoagulants. Chest X-ray showed infiltrates in both lungs. The SARS-Cov-2 antigen test performed at the Accident & Emergency Department was negative. However, the patient’s condition worsened rapidly and was admitted to the Intensive Care Unit with assisted ventilation provided within couple of hours after admission.
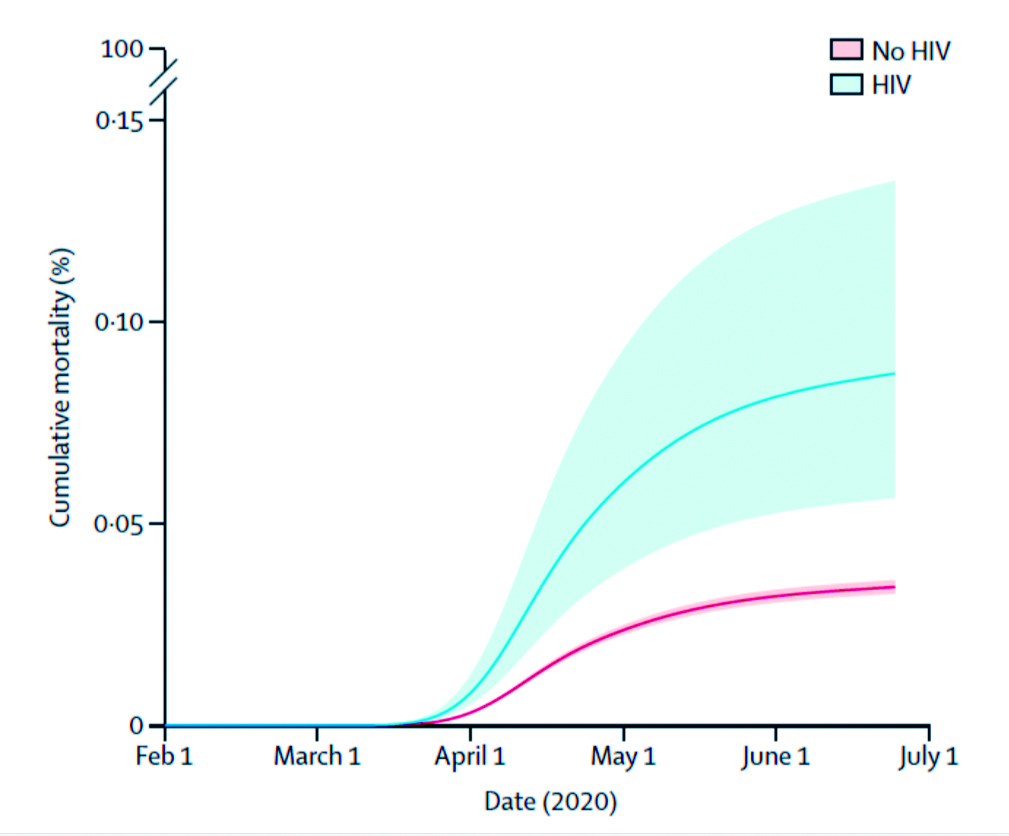
Figure 1. Cumulative COVID-19 mortality by HIV status6
Further diagnostic imaging revealed shadow images in the lungs and computed tomography (CT) indicated blockage of the pulmonary artery. “The blockage of pulmonary artery was unusual as the patient had been on anticoagulants,” Dr. Wong commented. Eventually, SARS-Cov-2 PCR test with bronchoaveolar lavage (BAL) taken at bronchoscopy showed positive result. “It is not surprising to detect SARS-Cov-2 virus in the lungs, but not in nasopharynx for patients who presented late,” Dr. Wong addressed.
In addition to SARS-Cov-2, pneumocystis jirovecii pneumonia (PJP) was subsequently detected in the BAL sample. The patient was tested HIV positive. The HIV infection probably occurred long before to the COVID-19 infection. Hence, Dr. Wong speculated that the severity of COVID-19 infection in the patient was possibly intensified by the HIV co-infection,which was in accordance with previous report6. “The existing HIV infection might have triggered PJP in this patient and the subsequent COVID-19 infection worsened the thromboembolic symptoms, even with anticoagulant treatment. The overall condition was thus very severe and, unfortunately, the patient succumbed after several days,” he noted.
In particular, Dr. Wong emphasised that older age was a main risk factor for severe outcomes of COVID-19 infection. He highlighted that the risk of severe COVID-19 cases is increased exponentially in Hong Kong and worldwide, whereas the occurrence of chronic diseases and/or uncontrolled HIV would further intensify the adverse outcomes. Dr. Wong further highlighted that patients with immunosuppression are generally at increased risk of severe COVID-19 outcomes. Given the patient exhibited no symptoms of HIV infection nor record of the infection in his medical history as well as other notable risk factors, Dr. Wong reminded that frontline clinicians should be open-minded that more risk factors can exist beyond the scope of initial diagnosis. In particular, Dr. Wong emphasised that PLWH on ART for HIV should continue the treatment while receiving treatments for COVID-19. Otherwise, the patient’s immunity would be upset and, even worse is the development of resistance against ART for HIV.
The Psychosocial Impacts of COVID-19
Besides pathophysiological impacts, the psychosocial impacts of COVID-19 pandemic are noteworthy. The socioeconomic disruptions of COVID-19 would disproportionally affect marginalised populations including PLWH. Former investigation on COVID-related stress on mental and clinical health of PLWH in the United States revealed that the impact on disruptions in healthcare access (47%), financial difficulty (41%), and feelings of anxiety and depression (48%) were significant among the respondents, regardless of HIV status. However, the results reflected that PLWH were more likely to experience job loss and income disruption compared to HIV-negative respondents (70% for HIV-negative vs 48% for PLWH, p = 0.03)8. In view of the fear of being infected by SARS-Cov-2, Dr. Wong highlighted that a certain portion of PLWH avoided access healthcare facilitates including follow-up visits at HIV Clinics, especially during the 5th wave of COVID-19 pandemic.
Holistic Support by the Local Healthcare System
As reported in former study, disruption in healthcare access was one of the major concerns for PLWH in certain countries. Whereas, the healthcare system in Hong Kong is remarkable Dr. Wong commented that the healthcare services for PLWH are mostly maintained during the COVID-19 pandemic, except certain treatments with considerable risk of COVID-19 transmission. “Most of the routine clinical processes performed in each consultation for PLWH including screening tests and various vaccinations were continued during the pandemic,” Dr. Wong addressed. Notably, the HIV Clinics would make sure the PLWH have had collected sufficient medications. Nonetheless, the local healthcare system, including the HIV Clinics, had faced significant challenge during the COVID-19 pandemic. For instance, the manpower of frontline clinicians was tightened during the 5th wave since some healthcare professionals were shifted to handle severe cases of COVID-19, thus leaving less staff in the HIV Clinics. Of note, most of the physicians handling COVID-19 cases were core members of HIV Clinics. Moreover, some nurses in the HIV Clinics were shifted to Accident & Emergency Department. Fortunately, the problem of tightened manpower was relieved by the appropriate contingent allocation of resources and adjustment on the clinical procedures. For example, for PLWH with stable condition, more amount of medications were provided after each visit in order to avoid discontinuation of ART due to sudden suspension of social services and/or lockdown measures. “Discontinuation of treatment is highly not desirable in PLWH, as the disease will rebound definitely,” Dr. Wong mentioned. Hence, the colleagues in HIV Clinics will make sure the PLWH to continue treatment during COVID-19 pandemic. Dr. Wong highlighted that there are nursing staff in the HIV Clinics specialised in contacting their HIV patients in order to update their conditions and to ensure they are on treatment properly in case the patients are lost to follow-up. Fortunately, the proportion of HIV patients lost to follow-up was small in general.
COVID-19 Vaccination for PLWH
In a survey on COVID-19 vaccination among PLWH in China, 2,570 out of 2,740 participants had never received COVID-19 vaccination though 57.2% of participants reported willingness to receive COVID-19 vaccination. Essentially, receiving advice supportive of COVID-19 vaccination from doctors (adjusted OR: 1.99, p <0.001), friends and/or family members (adjusted OR: 3.22, p <0.001), and PLWH peers (adjusted OR: 2.38, p <0.001) was associated with higher willingness to receive COVID-19 vaccination4. Dr. Wong agreed that PLWH would have many concerns on COVID-19 including vaccination. Their vaccination hesitancy is more pronounced as compared to general public due to the fear on adverse effects of vaccination on their disease. Counselling for PLWH on the safety profile of vaccination and the protection provided are thus essential during consultation. Of importance, there is no evidence suggesting that COVID-19 vaccination would affect the efficacy of ART for HIV, pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP). Dr. Wong stressed that COVID-19 vaccination is safe for PLWH. “All COVID-19 vaccines currently available in Hong Kong are either inactivated vaccine (Sinovac) or mRNA vaccine (Comirnaty), thus they are safe for HIV patients including those with advanced disease,” he mentioned. In view of the suboptimal immunity in HIV patients with advanced disease, their overall immunity against COVID-19 upon vaccination would be lower as compared to normal people. Therefore, an additional injection, totally 4 injections, of COVID-19 vaccine is recommended for HIV patients and immunosuppressed individuals9.
Be Well-equipped for Future Pandemic Challenges with Telemedicine
During the COVID-19 pandemic, certain healthcare and social services have been disrupted by the lockdown and social distancing measures. It is encouraging that the number of newly infected cases has been declining recently. However, this is not the end but we need to prepare for future pandemic challenges. Given the limited physical access to healthcare facilities during lockdown, telemedicine provides a sound alternative for delivering clinical services. El-Nahal et al (2022) compared the rates of visit completion among PLWH with the transition from in-person to mostly telemedicine visits during COVID-19 pandemic in the United States with pre-pandemic period. The results demonstrated that visit completion increased significantly from 88% pre-pandemic (n = 2,010) to 91% during pandemic (n = 1,929, p = 0.008)10. The findings hence suggested that delivering care via telemedicine would improve engagement of patients.
In addition to improving access to care, it is advocated that virtual platforms can help mitigate some of the perceived intimidation associated with face-to-face treatment11. These advantages would likely encourage PLWH to adhere with care and treatment. In Hong Kong, however, Dr. Wong commented that the clinical application of telemedicine in HIV care is still at the initial stage. The current scope of telemedicine application at the 3 designated HIV Clinics is only limited. However, he agreed that the COVID-19 pandemic has catalysed the progress of its implementation in clinical practice.
The long interval between consultations would be a reason for the limited application of telemedicine. Clinically, PLWH with stable disease can visit HIV clinic for consultation and collecting medication once per 6 months. While the burden on clinic visit is not significant, the PLWH are willing to spend in-person visits. Dr. Wong highlighted the practical difficulty in applying telemedicine. “It would be easier for subsequent consultations to be conducted through telemedicine approach, but not in the first instance which the doctor-patient relationship is yet to be established, especially when physical examinations are involved,” he commented.
Technical literacy can be another reason hindering the clinical use of telemedicine. Dr. Wong shared that some patients did have difficulty in setting up the required hardware and operating the computer programs. “After the patient had fixed all technical problems, the consultation was over already,” he said. This case highlights the importance of developing user-friendly telemedicine instruments since there are many patients not familiar with computer operation and information technology.
Although technical limitations still exist, there are emerging evidences reporting the successful experiences on improving clinical operations as well as patients’ outcomes with telemedicine. With further technical advancement, telemedicine is expected to play a crucial role in future clinical practice.
Concluding Remarks
Dr. Wong addressed that stigmatisation and discrimination towards patients infected with COVID-19 were observed. “The situation is similar to the early days of HIV pandemic. This is largely due to the misunderstanding towards to disease. Therefore, medical and social supports, including emotional support, for HIV Patients co-infected by COVID-19 are essential, particularly among the patients currently receiving no support,” he highlighted. He reminded that frontline clinicians should care about the feelings of these patients.
To conclude, Dr. Wong emphasised that the ART and follow-up for HIV/AIDS should not be interrupted by treatments for COVID-19. Practically, there are delayed follow-up cases due to patient’s fear of COVID-19 infection. Hence, it is advisable for frontline clinicians to remind the patients to comply with the prescribed treatments and follow-up, including blood testing. Last but not least, COVID-19 vaccination will not cause harm to HIV patients, and should be encouraged for protecting people against the disease.
References
1. Danwang et al. AIDS Res Ther 2022; 19: 1–12. 2. Suen et al. J Int Assoc Provid AIDS Care 2021; 20. DOI:10.1177/23259582211059588. 3. Barbera et al. HIV Res Clin Pract 2021; 22: 1. 4. Huang et al. JMIR Public Heal Surveill 2021; 7. DOI:10.2196/31125. 5. Yang et al. Curr HIV/AIDS Rep 2022; 19: 5. 6. Bhaskaran et al. Lancet HIV 2021; 8: e24. 7. Ng et al. J Clin Virol plus 2022; 2: 100062. 8. RaccamarichClaudia Uribe et al. Open Forum Infect Dis 2020; 7: S308–S308. 9. The Centre for Health Protection. Consensus Interim Recommendations on the Use of COVID-19 Vaccines in Hong Kong. 2022. 10. El-Nahal et al. AIDS 2022; 36: 355–62. 11. Grove et al. AIDS 2021; 35: 1328–30.





