
Specialist in General Surgery
Cool Down the Heartburn
A Closer Look at GERD Management
Gastroesophageal reflux disease (GERD) is one of the most common gastrointestinal (GI) diseases globally with the reported prevalence in Eastern Asia varies from 5.2 to 8.5%, whereas the incidence of GERD and its complications including Barrett’s oesophagus and adenocarcinoma of the oesophagus has been increasing throughout the world1. Patients with GERD may present with a wide spectrum of symptoms that can extend beyond the common presenting symptoms of heartburn and regurgitation2, leading to a significant decline in the quality of life of patients and is associated with a high economic burden. In the current feature story, Dr. Canon Chan highlighted the key issues in the management of GERD, particularly on refractory symptoms, and shared his opinions on emerging therapies combating the disease.
The Burden of GERD
GERD is a condition in which the reflux of gastric contents into the oesophagus provokes symptoms or complications and impairs quality of life. Heartburn and acid regurgitation are typical symptoms of GERD, whereas the disease can be associated with extra-oesophageal manifestations including asthma, chronic cough and laryngitis3. “In urban regions, the prevalence of GERD, defined by exhibiting GERD symptoms on more than 2 days per week, among working population can be up to 20%,” noted Dr. Chan. Former systematic review of the epidemiology of GERD involving 15 studies originating from North America, Europe, and Asia by Dent et al (2005) identified that the prevalence of GERD, defined by at least weekly heartburn and/or acid regurgitation, ranged from 10-20%, with the highest prevalence in North America (19.8-20%, Figure 1)4. Essentially, there is evidence suggested that the prevalence of GERD has increased significantly since 1995 (rate ratio [RR] 2005-2009 versus pre-1995: 1.50, 95% confidence interval [CI]: 1.26-1.82, p < 0.0001), particularly in North America and East Asia5.
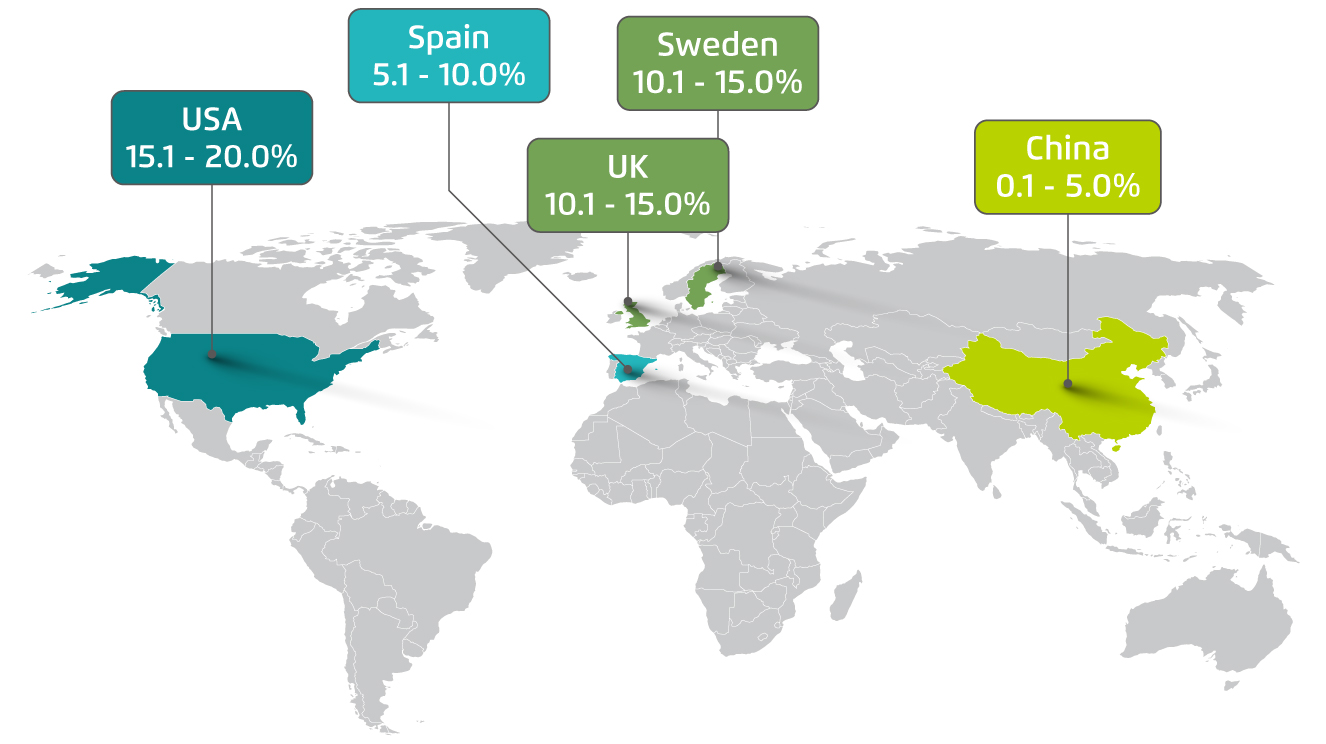
Figure 1. The prevalence of GERD in selected regions4
Dr. Chan outlined that patients with GERD generally report the occurrence of stomach gas and pain, whereas the feeling of heartburn would be developed as disease progresses. Heartburn is more likely to occur under mental stress or at night, whereas nighttime heartburn may cause sleeping difficulties and impair next-day function. “Nocturnal awakenings are prevalent among patients with GERD and is associated with insomnia and sleep dissatisfaction,” commented Dr. Chan. He further added that other GERD-related symptoms include oesophagitis, bad breathe, hoarseness and chronic coughing. Apart from its impact on quality of life, GERD can progress to various complications such as oesophageal cancer if untreated. Moreover, GERD symptoms are reported to constitute a significant burden for many patients in disrupting social and emotional well-being1.
Besides adverse health impacts, the economic burden of GERD is substantial. For instance, Bruley des Varannes et al (2013) reported that the mean total cost of GERD per patient with persistent symptoms in France over the 12-month follow-up period was £á5,237, while 89% of which was due to lost work productivity6. More recently, Gyawali et al (2018) estimated that the GERD-related expenses, mainly on medications and diagnostic testing, in the United States reaches US$9-US$10 billion/year7. Importantly, the disease burden of GERD is intensified by the high and increasing prevalence. Hence, effective prevention and timely management of GERD is crucial in controlling the adverse impacts of GERD. Notably, Dr. Chan reminded that male gender, alcohol consumption, tobacco smoking, obesity, late night supper and sweet food are associated with an increased risk of GERD symptoms.
Diagnosing GERD
The diagnosis and classification of GERD in local clinical practice are based on the global consensus in Montreal Criteria2. Dr. Chan stated that the diagnosis of GERD is typically made by assessment on clinical symptoms, such as heartburn or acid regurgitation occurs on more than 2 days per week or report on serious symptoms such as nocturnal awakening, followed by objective testing with endoscopy in order to detect the occurrence of oesophagitis. “In general, symptom assessment and endoscopy are accurate in diagnosing GERD. Nonetheless, proton pump inhibitor (PPI) trial would be performed after symptom assessment for certain patients in order to enhance the accuracy. When the patient exhibits persistent symptoms but not respond in the PPI trial, endoscopy or oesophageal pH monitoring would be recommended,” Dr. Chan commented.
GERD can be classified as either typical or atypical, based on clinical manifestations. Very often, GERD manifests with typical symptoms including heartburn and acid regurgitation. Nonetheless, GERD may present with other atypical symptoms such as laryngitis, asthma, cough, or non-cardiac chest pain (Figure 2). Of note, patients with atypical manifestations may not have concomitant complaints of heartburn8. On the other hand, Dr. Chan highlighted that GERD can be classified according to its severity. He added that the severity staging of GERD would facilitate physicians in deciding the most appropriate treatment protocol for the patients.
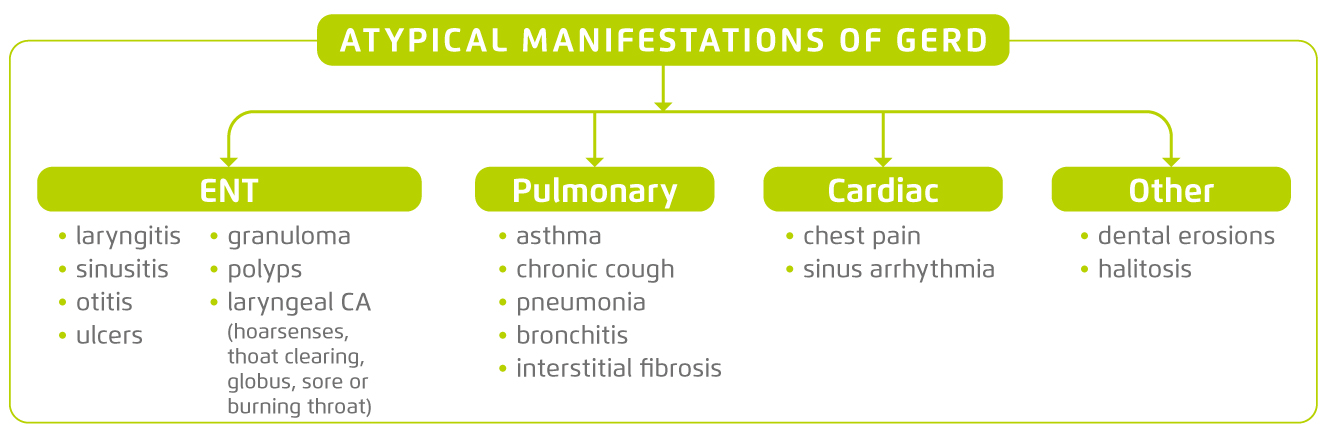
Figure 2. Atypical manifestations of GERD8, ENT = ear, nose, throat; CA = cancer
The Management of Refractory GERD
While there is no consensus on the definition of refractory GERD in Asia or in Western countries, the Asian Pacific Association of Gastroenterology (APAGE) addressed in 2016 that persistent and troublesome GERD symptoms unresponsive partially or completely to at least 8 weeks of a standard dose of PPI may be termed refractory GERD symptoms. In the context, the standard dose of PPI is defined as the approved dose in each country or region, whereas troublesome GERD symptoms are those impair quality of life9.
Previous systematic review by El-Serag and Jones (2010), which involved 19 studies in individuals with GERD taking PPI, suggested that the prevalence of persistent troublesome heartburn and regurgitation was 17% and 28%, respectively. In observational primary care and community-based studies, 45% of participants reported persistent GERD symptoms10. Dr. Chan commented based on previous studies investigating efficacy of PPIs that about 30-40% of GERD patients are unresponsive to PPI treatment.
There are many potential causes of refractory GERD that vary in incidence, severity and frequency. Previous opinions advocate that poor compliance and adherence to PPI treatment would be one of the reasons11,12. Nonetheless, the most common mechanisms for refractory GERD include functional bowel disorders, weakly acidic reflux, and residual acid. Factors related to metabolism and bioavailability play a limited role in PPI failure12. In particular, Dr. Chan commented that most of the patients with refractory GERD are concurrently suffered from comorbidities such as diabetes mellitus (DM), chronic kidney disease and liver impairment. The metabolism of PPI in these patients would be affected and hence limiting the bioavailability of PPI. In addition, hiatal hernia, which refers to herniation of intra-abdominal contents through the oesophageal hiatus of the diaphragm (Figure 3), is commonly linked to GERD and its complications13. Dr. Chan explained that, in hiatal hernia, the negative pressure in thoracic cavity would trigger the reflux of gastric acid.
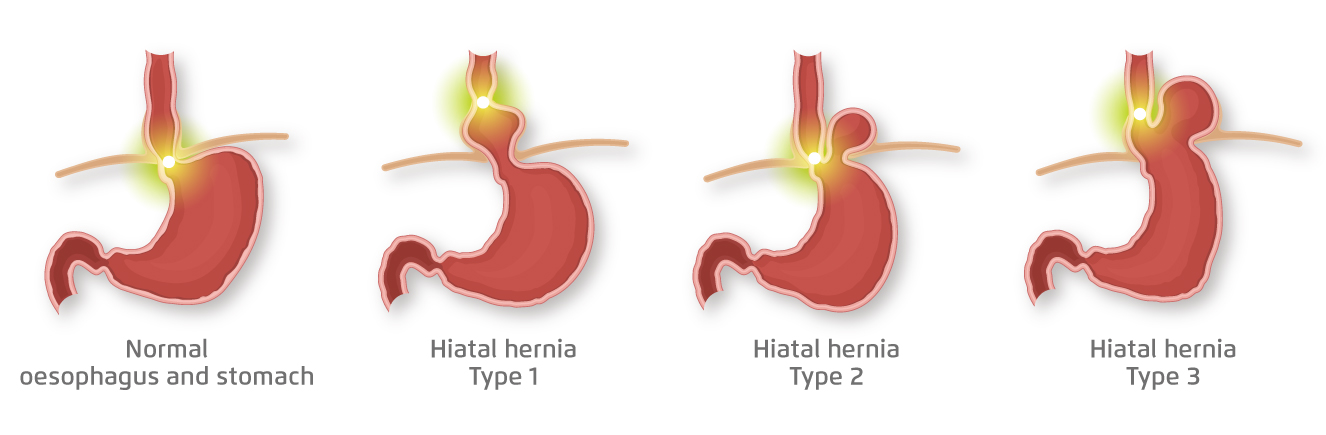
Figure 3. Types of hiatal hernia13
Lifestyle interventions such as avoid eating beyond fullness and eating spicy foods, controlling meal times and quit smoking are expected to alleviate the symptoms14 and hence are recommended for all GERD patients. However, Dr. Chan mentioned that the effectiveness of lifestyle interventions is limited in reality. To manage refractory GERD, he emphasised that the first distinction is whether the patient has GERD that is truly refractory to PPI or non-GERD pathology. “It is crucial to exclude the possibilities of hiatal hernia and other comorbidities as well as tumours. Hence, further diagnostic testing including upper GI endoscopy has to be performed. In cases of persistent troublesome symptoms, ambulatory reflux monitoring and oesophageal manometry are recommended,” he advised.
Upon detection of clinical phenotypes including esophagitis, Barrett’s oesophagus and/or high frequency of reflux, which respond poorly to pharmacological treatments, anti-reflux surgery would be required. Dr. Chan highlighted that, instead of long-term PPI treatment, surgical treatment would be beneficial and preferred for younger patients with refractory GERD. In reviewing the safety profile of anti-reflux surgery, he estimated that the risk of adverse events of anti-reflux surgery would be about 1-3%.
Concerns on Long-term PPI Treatment
PPIs have been the mainstay for GERD treatment due to their effective acid suppression. However, Dr. Chan mentioned that the potential side effects of prolonged PPI treatment have been a concern among his patients. “In recent years, there are clinical data suggesting that prolonged PPI treatment of more than 12 months with background of Helicobacter pylori (H.Pylori) infection would increase the risk of gastric cancer, but this is an association rather than causal relationship,” he stated. Hence, patients with a proven indication for a PPI should continue to receive it in the lowest effective dose15. In order to enhance the efficacy of PPI treatment, Dr. Chan suggested that most PPIs should be taken before meals. He further emphasised that adherence to treatment is essential for achieving better outcomes, whereas PPI treatment normally takes 1 week to generate the therapeutic effects.
Dr. Chan commented that current treatments for GERD, both medications and surgeries, are safe and effective in general. He stated that the allergic reactions with PPI treatment are practically uncommon. “Mild adverse events such as diarrhoea and alteration of gustation have been reported by some patients upon long-term PPI treatment. Nonetheless, the benefit in relieving heartburn yielded by PPI treatment is significant,” he noted. Notably, he reminded that, in elderly patients with comorbidities such as osteoporosis and DM, PPI treatment would possibly interact with the patients’ existing treatments and might reduce the absorption of nutrients such as calcium and iron.
Emerging Technologies Countering GERD
While endoscopy is recommended in diagnosing GERD, pH monitoring can be applied to quantify reflux and assess the relationship between reflux episodes and the patient’s symptoms. Recent development in wireless capsule (Figure 4) allows prolonged 96-hour monitoring with improved patient tolerance and provides a higher chance of finding a positive symptom association than traditional 24-hour transnasal catheter recording16. Dr. Chan outlined that pH monitoring can be performed to evaluate effectiveness of PPI treatment by switching off the treatment in selected period during the 96-hour monitoring. In addition to enhancing accuracy of diagnosis, pH monitoring would provide information for physicians in deciding further treatments.
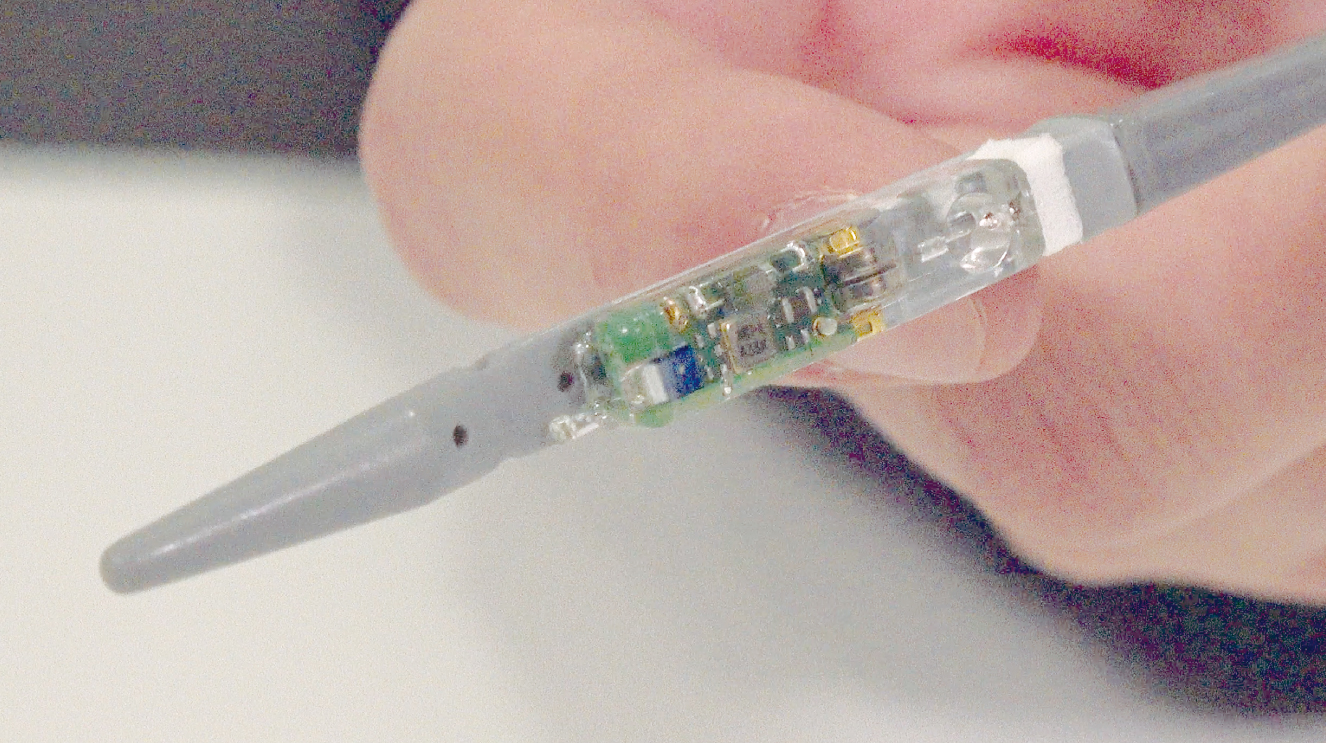
Figure 4. Wireless capsule for pH monitoring
In addition to diagnostic tools, technological advancement has driven the emergence of treatment options for controlling GERD symptoms. In the current interview, Dr. Chan shared his opinions on 3 therapies, namely bile acid sequestrants, magnetic sphincter augmentation (MSA) and electrical stimulation.
Duodendogastrooesophageal reflux of bile acids has been hypothesised to play an important role in the development of oesophageal symptoms, oesophagitis, Barrett’s metaplasia and oesophageal adenocarcinoma. Moreover, bile reflux into the airway has been proposed to contribute extra-oesophageal GERD manifestations. Hence, therapies targeting bile acids may have a role in managing GERD, especially in patients not responding completely to acid inhibition17. In a recent randomised control trial by Vaezi et al (2020), add-on bile acid sequestrants with ongoing label-dose PPI for 8 weeks significantly reduced weekly heartburn severity and regurgitation symptoms frequency as compared to placebo18. However, Dr. Chan commented that only small number of bile acid sequestrants has been registered in Hong Kong. It is also noteworthy that bile acid sequestrants are not primarily indicated for treating symptoms of gastric acid reflux but reflux of bile acids. He stated that bile acid sequestrants are generally safe. However, there is no supporting evidence on long-term treatment to date.
MSA works by closing around the gastrooesophageal junction and thus increasing pressure to prevent pathologic reflux while allowing for food and liquid bolus to pass through16. Saino et al (2015) demonstrated in a 5-year prospective study that MSA implantation could significantly improve reported quality of life in patients with GERD symptoms controlled poorly with PPIs as compared to baseline. In particular, complete discontinuation of PPIs was achieved by 87.8% of patients19. Although the implantation of MSA can be done by laparoscopy with less trauma as compared to traditional anti-reflux surgery, there are many technical requirements for the implantation. For instance, patients with severe hiatal hernia are not eligible for MSA implantation. Dr. Chan added that it has to be no previous surgeries done in the patient’s stomach. Importantly, the MSA treatment is indicated for patients with mild-to-moderate GERD symptoms but not for severe diseases. Moreover, the price for MSA treatment is much higher than traditional anti-reflux surgery.
Electrical stimulation controls reflux by stimulating the lower oesophageal sphincter (LES) to increase the resting sphincter tone. The device can be implanted laparoscopically, whereas the battery is estimated to last for 10 years. Kappelle et al (2015) showed that electrical stimulation yielded improved scores of quality of life and acid exposure in 44 partial PPI responders upon 6 months of treatment20.
While the disease burden of GERD is significant, current treatments managing the disease is generally effective and safe. Thanks to the advancement in biomedical technologies, accurate diagnostic tools and treatment modalities for GERD, including refractory disease, are emerging. As a final remark, Dr. Chan recommended that patients with newly diagnosed GERD and not respond to prescribed treatment for 2 weeks should seek for further medical advices and diagnostic testing in order to better understanding the pathological condition and facilitate timely treatment.
References
1. .Kumar et al. Cureus. 2020;12(9). 2. .Vakil et al. Am J Gastroenterol. 2006;101(8). 3. .DeGiorgi et al. Acta Otorhinolaryngol Ital. 2006;26(5):241-246. 4. .Dent et al. Gut. 2005;54(5):710-717. 5. .El-Serag et al. Gut. 2014;63(6):871-880. 6. .Bruley des Varannes et al. BMC Gastroenterol. 2013;13(1):39.7. .Prakash Gyawali et al. Gut. 2018;67(7):1351-1362. 8. .Vaezi. MedGenMed. 2005;7(4):25. 9. .Fock et al. Gut. 2016;65(9):1402-1415. 10. .El-Serag et al. Aliment Pharmacol Ther. 2010;32(6):720-737.11. .Dickman et al. J Neurogastroenterol Motil. 2015;21(3):309-319. 12. .Mermelstein et al. Clin Exp Gastroenterol. 2018;Volume 11:119-134. 13. .Dunn et al. Ann Laparosc Endosc Surg. 2020;5(0):2914. .Yuan et al. Therap Adv Gastroenterol. 2019;12. 15. .Vaezi et al. Gastroenterology. 2017;153(1):35-48. 16. .Jiang et al. Curr Treat Options Gastroenterol. 2020;18(1):69-81. 17. .McQuaid et al. Aliment Pharmacol Ther. 2011;34(2):146-165. 18. .Vaezi et al. Gastroenterology. 2020;158(8):2093-2103. 19. .Saino et al. J Laparoendosc Adv Surg Tech. 2015;25(10):787-792. 20. .Kappelle et al. Aliment Pharmacol Ther. 2015;42(5):614-625.





