The Rising Significance of Telehealth in Local HIV Care under COVID-19 Pandemic
Under the COVID-19 pandemic, various preventive measures have been adopted to control disease transmission, such as the closure of public facilities, quarantine and social distancing. The lockdown provisions help lower the infection rate but also severely disrupt local healthcare services.1 In particular, the access to healthcare services by people living with HIV (PLWH) may be affected by the lockdown provisions, which potentially poses an increased risk of disruption of antiretroviral therapy (ART) and hence HIV-associated morbidity and mortality. While telehealth has gained popularity in recent years, it may be an alternative for PLWH to gain access to healthcare services during pandemics such as COVID-19.2
Limited Healthcare Services for PLWH during COVID-19
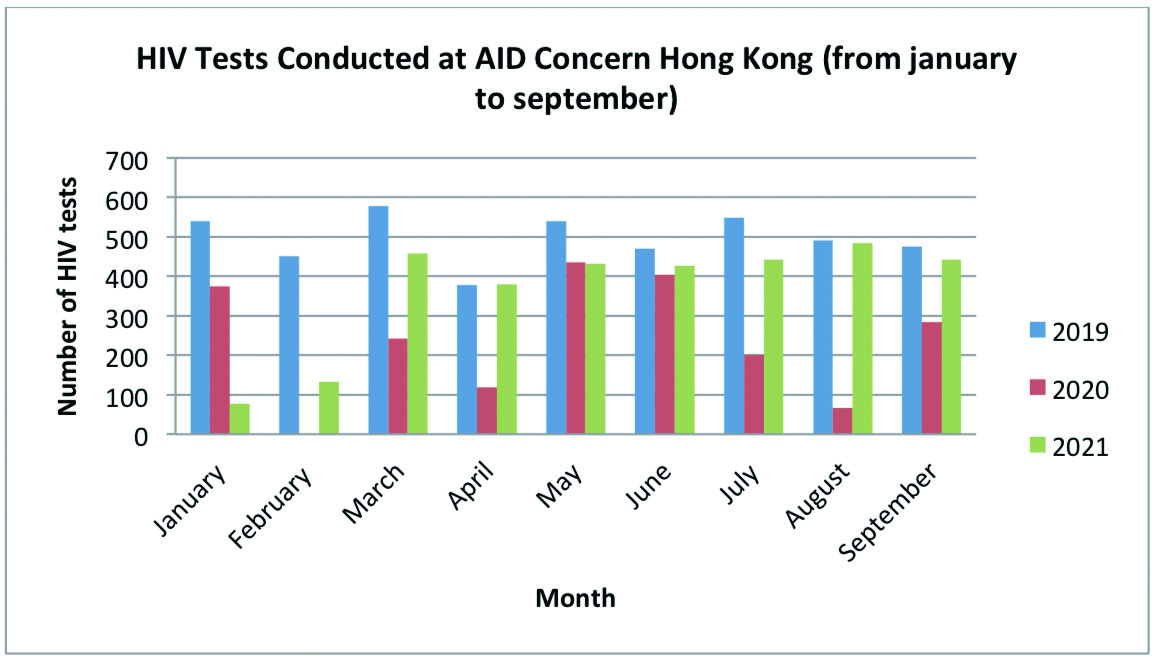
Local healthcare services for PLWH are available mainly at public medical centres with patients’ privacy strictly protected.1 Privacy is of utmost importance for PLWH to access HIV services in consideration of potential stigmatisation.1 Unfortunately, with the rapid and widespread of the coronavirus disease, the services provided at HIV testing centres were suspended until the end of the third wave of the pandemic in August 2020, resulting in the reduction in the number of HIV tests conducted during the period (Figure 1).1
Besides the closure of healthcare facilities, a substantial portion of PLWH refused to access public healthcare services in order to reduce the risk of infection. According to the survey conducted by Hung et al (2020), 30.4% of the public reported that they would avoid medical consultation during the COVID-19 outbreak in Hong Kong.3 The main reason for the avoidance among users of HIV healthcare services was the fear of being infected when accessing the services.4 The disruption of HIV/AIDS-related services not only caused a reduction in routine HIV testing but also disturbed the linkage to HIV care and interference with ART.1 Adherence to treatment is the key to successful ART.5 If the therapy was interrupted, the effectiveness of ART might also be seriously affected.
Self-testing kits are encouraged during the pandemic. However, its distribution to users is a big challenge under the rigorous social distancing provisions.1 Furthermore, most of the users may not realise the availability of the self-testing kit without effective broadcasting of the information.1 While identification of PLWH among the high-risk population is one of the obstacles in containing the HIV pandemic. The limited healthcare services would undoubtedly hinder the progress in identifying HIV-infected people and hence increase the risk of HIV transmission.4
The Potential Role of Telehealth during Pandemic
To reduce public exposure and the risk of infection, many HIV services including counselling services, legal services and HIV support group meetings have been switched to virtual mode such as telephone or secure video conferencing in several countries.4 This kind of health delivery mode is known as telehealth. Telehealth has been defined by the World Health Organization as ”delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities”.6
Telehealth offers virtual platforms for specialists and patients, which can alleviate the fears regarding infection as well as the risk of exposure while waiting or during transportation.7 It also enables remote triaging by allowing patients to seek help from healthcare professionals through online platforms for a symptom check video call, and specialists can triage them according to the severity or screen out high-risk patients.2 This helps minimise the risk of contamination in the clinics.6 As a result, staff and patients are both more relieved and comfortable when using HIV services. Telehealth services can help provide ongoing counselling and support services efficiently, and the linkage between specialists and HIV patients increases which also leads to an enhanced workflow.8
Telehealth is more than just tele-conferencing that we can also utilise the technologies to monitor patients’ conditions. Tele-monitoring includes remote monitoring of patients’ clinical data to provide an opportunity for feedback and intervention.9 In the United States, software called CAREW was developed to track ART patients. It acts as a tool for clinicians to manage electronic health records of the patients allowing HIV treatment providers to identify, refer, and track patients in need of dual care.10 Telehealth can also help facilitate persistent engagement in pre-exposure prophylaxis (PrEP) uptake.11 By providing a convenient platform for delivering PrEP, people can get the treatment easily and the risk of treatment discontinuation would be reduced.11 Telehealth can also act as a preventive measure for HIV transmission. Government and organizations can deliver effective behavioural interventions and valuable messages to the general public about safe sex and the possible risk of acquiring HIV.8 Besides, by providing patients with accessible health education and decision-making options, telehealth services can help patients enhance their self-care competency.9
Challenges in Telehealth in Local Clinical Setting
There are several challenges and limitations when switching traditional healthcare services to telehealth services. During the pandemic, 85% of prescribers used telehealth to deliver HIV healthcare. However, most of the individuals were not using these services.12 The main reasons people refuse to use telehealth services may be privacy concerns and distrust of advanced technology.7 People may worry that their personal information is not secured.
Besides privacy concerns, people may not be familiar with digital devices or have financial issues to possess a computer or smartphone.7,13 Basic technology resources and the internet is necessary for telehealth services, otherwise the patients cannot access any system nor communicate with the designated specialist.7 Moreover, digital literacy may also be a barrier for people to explore telehealth services.7 Last but not least, one of the key elements of provider-patient relationships is the intimacy built up during the services. Without the in-person encounter, this strength of the personal connection is weak and it is hard to connect with patients or gain their trust.6,7
Conclusion
With the rapid spread of coronavirus, employing telehealth is an effective and safe alternative to engaging with HIV patients. It can help to diagnose, treat, respond and prevent. This kind of new healthcare module is likely to retain beyond the pandemic. Although there are some limitations, users’ satisfaction with telehealth services has been reported.14 Hence, boosting and expanding the scope of telehealth services are warranted. Meanwhile, it could be a hybrid approach including a mix of telephone, video, and in-person visits to fit patients and their healthcare needs.13 It is not necessary to switch all traditional services to telehealth services immediately, it can be an adjuvant approach initially. Nonetheless, our society needs to be well-prepared for future pandemics.
References
1. Suen et al. J Int Assoc Provid AIDS Care 2021; 20. DOI:10.1177/23259582211059588. 2. Smith et al. J Telemed Telecare 2020; 26: 309–13. 3. Hung et al. Int J Heal Policy Manag 2022; 11: 508–13. 4. Suen et al. Int J Infect Dis 2021; 106: 358–62. 5. Fan et al. BMC Public Health 2020; 20. DOI:10.1186/S12889-020-8171-5. 6. Reiss et al. Medicina (Kaunas) 2020; 56: 1–13. 7. Grove et al. AIDS 2021; 35: 1328–30. 8. Telehealth for HIV Prevention and Care Services | Treat | Effective Interventions | HIV/AIDS | CDC. 9. Legislative Council of the Hong Kong Special Administrative Region - Development of telehealth services. 10. Avery et al. Curr Opin HIV AIDS 2017; 12: 488–93. 11. Koester et al. J Int Assoc Provid AIDS Care 2020; 19. DOI:10.1177/2325958220919269. 12. Hung et al. Int J Antimicrob Agents 2021; 58: 21004180. 13. Smith et al. HIV AIDS (Auckl) 2021; 13: 651. 14. Dandachi et al. AIDS Behav 2020; 24: 2463.





