
Specialist in Haematology & Haematological Oncology
Clinical Assistant Professor (Honorary),
Department of Clinical Oncology,
Faculty of Medicine, CUHK
Scenario
After the Turning Point - Living with Multiple Myeloma
Multiple myeloma (MM) is a malignancy of plasma cells characterised by a monoclonal proliferation of plasma cells resulting in the production of monoclonal antibody and end-organ damage1. Thanks to the development of novel therapies for MM, the outcomes of patients with newly diagnosed MM (NDMM) or relapsed/refractory MM (RRMM) have been significantly improved2. Nonetheless, despite prolonged survival of MM patients for more than 10 years is no longer rare, a substantial proportion of MM will relapse or does not respond to therapy3. Hence, there are clinical opinions advocating that the aim of therapy for MM is to induce an objective response with a prolongation of survival and to improve the patients’ quality of life. In a recent sharing, Dr. Li Wa, Specialist in Haematology & Haematological Oncology, highlighted the essences in clinical management of MM and discussed the holistic care for patients with MM.
The Silent First Attack
Generally, more timely diagnosis could have a positive impact on MM patients both in terms of treatment options and subsequent survival and quality of life. A previous meta-analysis by He et al (2003), which included 131 MM patients with early treatment and 131 MM patients received deferred treatment as control, suggested that treatment at early stage MM would significantly delay myeloma progression4. Nonetheless, myeloma has been classified as one of the hardest cancers to diagnose and diagnostic delays are common. It has been reported that many patients experience a diagnostic interval longer than 3 months until diagnosis is confirmed5.
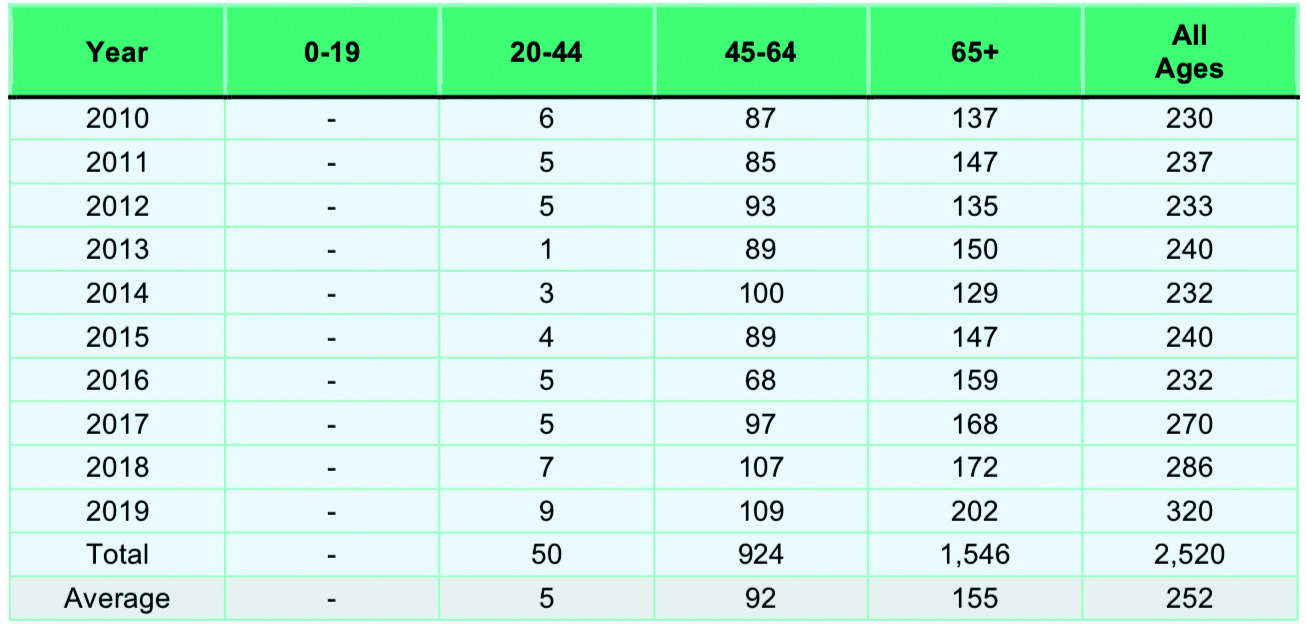 Table 1. Number of new MM cases by year and age group66
Table 1. Number of new MM cases by year and age group66
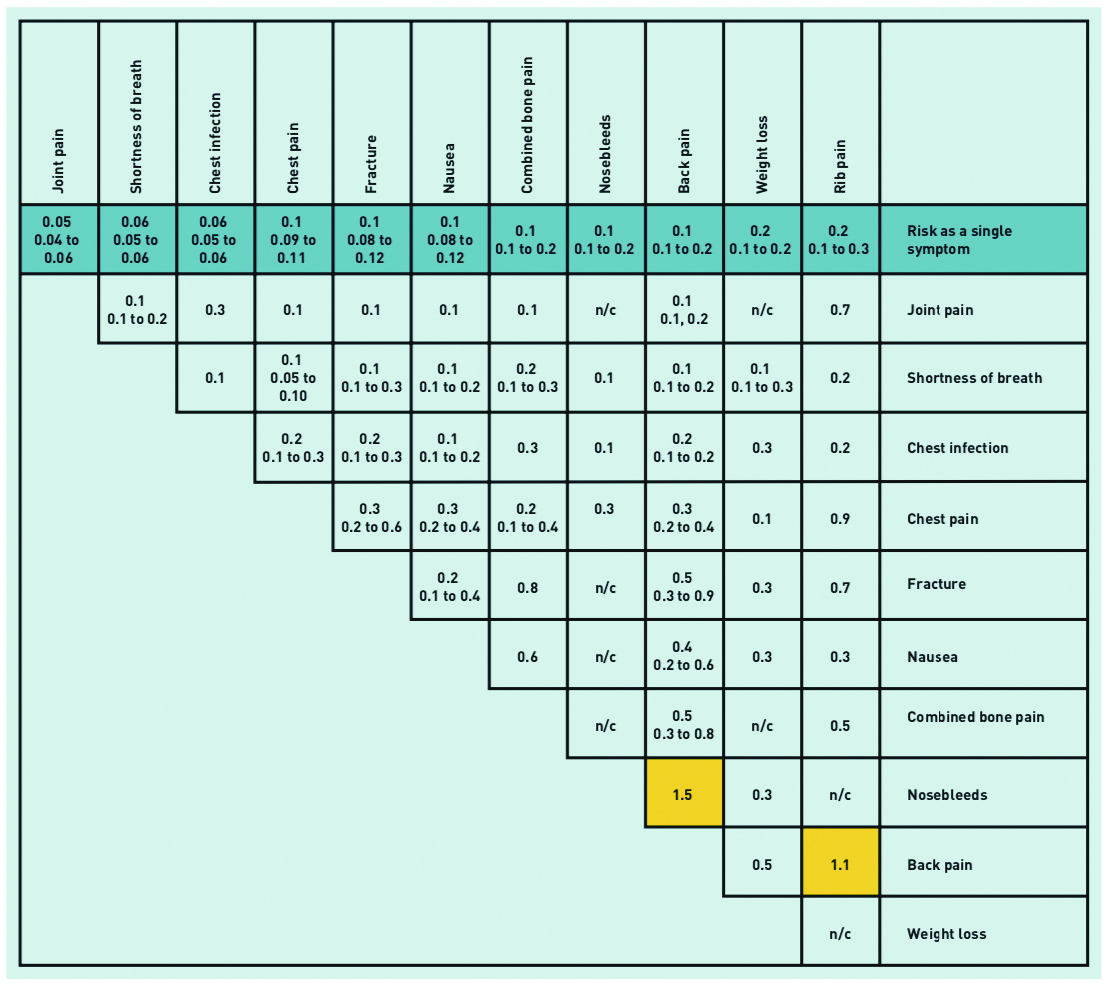
Table 2. Positive predictive values for myeloma symptoms in patients aged ≥60 years, for single and paired features 8
Dr. Li explained that one of the reasons for the delayed diagnosis of MM is the rarity of the disease. According to the Hong Kong Cancer Registry, the average number of new MM cases for all ages was 252, or an age-standardised incidence rate of 1.7 per 100,000 persons, in the period 2010-2019 (Table 1)6. "Unlike lung and colon cancers, myeloma is uncommon and the opportunity for general practitioners to come across this disease is small. Hence, it would not be easy to aware of its occurrence" Dr. Li noted.
Symptoms in many cancers are indicative of the diseases, such as rectal bleeding for colorectal cancer, and hence are referred to as 'red flags' indicating the need of urgent investigation and referral to specialist services7. Unfortunately, Dr. Li mentioned that the symptoms of MM are non-specific and not predictive. He quoted that most of the symptoms of MM have a positive predictive value (PPV) of less than 1%. While bone pain, mainly affecting the back, is a symptom approximately 7 months before diagnosis in nearly half of all patients with myeloma, its PPV as a single symptom for MM is only 0.1-0.2 (Table 2)8. The predictive values of MM symptoms partly explain the diagnostic delays.
The uncommon diagnosis of MM and the non-specific symptoms are main reasons for the diagnostic delay of the disease. Considering that the average age of patients at the time of diagnosis is nearly 70 years of age, comorbid conditions are often coexistent with the MM diagnosis. Dr. Li added that the diagnostic process appears to be more difficult in those patients suffered from multiple medical problems. For instance, bone pain is a symptom of MM, whereas osteoporosis is common among elderly and can induce bone pain as well. Hence, it would be difficult to diagnose MM based on the occurrence of bone pain in elderly patients.
Upset Quality of Life in MM
MM is characterised by the uncontrolled expansion of malignant plasma cells in the bone marrow and the production of a monoclonal immunoglobulin. Bone marrow involvement often results in anaemia, lytic bone disease, bone destruction, fractures and hypercalcemia9. Dr. Li outlined that anaemia and bone pain are the most common initial symptoms of MM observed clinically. Of note, he mentioned that some of the pathophysiological damages caused by the disease could be irreversible due to delay diagnosis. In these cases, the impacts on quality of life of the patients would be substantial.
While the paraprotein may result in renal insufficiency, Dr. Li stated that some MM patients referred to the specialist clinics have already been suffered from end-stage renal failure, “Some of these patients have their renal function improved upon treatment, but in some cases the renal function cannot be fully recovered and long-term dialysis treatment is required.”
While bone pain can be induced by pathological fractures associated with MM, the intensity of pain can be varied and acute fractures are generally associated with higher intensity of pain. Dr. Li noted that the pain can be mild as irritation in many cases. However, in certain cases of MM involving the spine, pathological fracture of the vertebral body and neurological deterioration can occur. Whereas, epidural myeloma would cause spinal cord compression leading to progressive paraplegia and sensory disturbance10. “These patients would possibly be bed-bound in the rest of their life, even the myeloma is in good remission,”Dr. Li commented. Thus, the impacts of MM on patients quality of life would be evaluated based on reversibility of the damages created.
To facilitate early diagnosis of MM, Dr. Li advised that a high degree of suspicion is essential for frontline clinicians. Despite the non-specific nature of MM symptoms, performing blood tests for the patient upon the observations on unexplained bone pain, fatigue, and recurrent infections would help early identifying abnormality. The recommended blood test consists of the assessments on blood calcium level, renal function (serum creatinine), and anaemia (haemoglobin). In addition, imaging to identify bone lesions in needed as well11. “The laboratory findings would improve the predictive value of MM symptoms occurred,” Dr. Li commented. In cases of suspected myeloma, more specific tests like serum protein electrophoresis and immunofixation can be performed11.
Curative versus Disease-control
Upon NDMM has been documented, some clinicians advocating the curative approach tend to incorporate all active agents early in the disease course in order to target the disease at its most vulnerable stage before the development of micro-environmental independence and secondary cytogenetic abnormalities. In contrast, clinicians favouring disease-control prefer a risk-adapted approach in which an aggressive strategy is pursued for intermediate-risk and high-risk patients, whereas an alternative sequential therapy approach is offered for standard-risk patients in order to minimise toxic effects and to maximise quality of life12.
"Follow the argument, then disease should be treated early in the course. Yet the treatment of smoldering myeloma is not yet a standard practice for all patients" Dr. Li commented. He outlined that MM develops from a pre-malignant plasma cell dyscrasia, namely monoclonal gammopathy of unknown significance (MGUS). MGUS has the potential to evolve into smouldering MM, which then progresses into MM. However, the progression can be very slow and the vast majority of patients do not progress through the full spectrum of disease. Particularly, he mentioned that MGUS is relatively common among elderly, with the incidence approximately 10% in people aged over 80. Essentially, most patients with MGUS do not progress to myeloma, the risk being approximately 1% per year13. "Although initial mutations and monoclonal band development occur in MGUS, no damage can be observed in the patients and no treatment will be prescribed at this stage" Dr. Li stated.
Dr. Li further addressed that roughly 10% of patients with smouldering MM would progress to MM. Based on the disease load, a portion of smouldering MM is classified as high-risk. According to the NCCN Guidelines, treatments can be initiated in some cases of smouldering MM14. Nonetheless, Dr. Li commented that the initiation of treatment for smouldering MM does not aim to cure the disease. He added that, minimal residual disease (MRD) detection is not a routine in daily practice, and the status of cure cannot be easily defined practically. "Aggressive treatments at the initial stage which shows no clinical symptom would not generate any clinical benefit. On the contrary, this will exhaust treatment options for subsequent lines of treatment. Also, the potential toxic effects of treatment should be taken into account" he expressed.
Coping with the Fear of Recurrence
Although the majority of patients respond well to initial therapy and disease levels are greatly reduced, treatment is generally not curative and most patients will relapse at some point. In addition to provide the appropriate treatment according to the specific status of each patient, Dr. Li advised that frontline clinicians need to educate and communicate with the patients about the disease and the treatments. Of note, a stepwise approach in communication would facilitate better understanding and acceptance for the patients.
Dr. Li stated that his treatment protocol for each patient is defined based on the shared decision-making with his patients.
"Informing the patients on the potential adverse events and how they can be handled before prescribing treatment is recommended" Dr. Li highlighted that preparing the patients for potential outcomes is important. In fact, some of the adverse events associated with MM as well as its treatments are inevitable that the patients need to live with them. Hence, Dr. Li would remind his patients on the nature of the disease and the response strategies during the course of treatment. This is particularly important when the indications of recurrence were observed during clinical monitoring. Besides psychological preparation, advices on financial preparation are also very important. On the other hand, MM patients may seek psychological support from certain patient support organisations.
Triumph in the Battle
MM is a rare but real disease that is generally considered incurable. The burden of MM-related symptoms, treatment-related toxicities, and psychosocial effects adversely impact the health- related quality of life of patients. Despite novel agents have shown improved rates of response, progression-free survival and overall survival, Dr. Li emphasised that early treatment is necessary in preserving, salvaging organ functions. While the patient's quality of life mirrors the course of the disease that it is worsen with disease progression but improved with effective therapy, early treatment would not only prolonged survival but expect to increase quality of life. In fact, most of the MM therapies are well-tolerated and patients may carry on their usual lives.
disease progression but improved with effective therapy, early treatment would not only prolonged survival but expect to increase quality of life. In fact, most of the MM therapies are well-tolerated and patients may carry on their usual lives.
While improving quality of life would be of great importance in the management of MM, coping with the stress associated with relapse disease is one of the major issues in this regard. Yet, the traditional approach of using the most effective therapy does not take into considerations psychologic and socioeconomic factors which can result in significant burden to the MM patient. Hence, as advised by Dr. Li, communication with the patients with the appropriate approach at the right timing is essential. In particular, advices on psychological and financial preparation are crucial in addition to medical support. To conclude, in improving both the survival and quality of life for MM patients, a multidisciplinary team approach with a focus on shared decision-making based on the patients goals has to be emphasised.
References
1. Padala et al. Med Sci 2021; 9: 3. 2. Richardson et al. Expert Rev. Anticancer Ther.2018; 18: 751-V64. 3. Dimopoulos et al. Clin Lymphoma, Myeloma Leuk 2018; 18: 163-173.e6. 4. He et al. Cochrane Database Syst Rev 2003; 2003. DOI:10.1002/14651858.CD004023. 5. Koshiaris et al. BMJ Open 2018; 8: 19758. 6. Hong Kong Cancer Registry, Hospital Authority. https://www3.ha.org.hk/cancereg/allagesresult.asp (accessed May13, 2022). 7. Koshiaris. Int J Hematol Oncol 2019; 8: IJH13. 8. Shephard et al. Br J Gen Pract 2015; 65: e106. 9. Seitzler et al. Expert Rev Hematol 2019; 12: 419¡V24. 10. Ha et al. J Korean Neurosurg Soc 2013; 54: 151. 11. Myeloma Diagnosis Pathway-V Myeloma Academy. https://academy.myeloma.org.uk/resources/myeloma-diagnosis-pathway/ (accessed May14, 2022). 12. Rajkumar. Nat Rev Clin Oncol 2011; 8: 479. 13. Bird et al. Palliat Care Soc Pract 2019; 13. DOI:10.1177/1178224219868235. 14. Kumar et al. J Natl Compr Cancer Netw 2020; 18: 1685-V717.





