

Specialist in Dermatology and Venereology
Good Skin, Good Health
Decoding the Multifaceted Burden ofAtopic Dermatitis
Atopic dermatitis (AD) is one of the most common chronic skin diseases and is characterised by itch and inflammatory eczematous lesions. While the condition most often develops during early infancy and childhood, it is prevalent in adults as well. In addition to skin pain and itch, AD also causes a wide spectrum of physical and psychosocial impairment affecting the patients as well as their families1. With the recent pharmaceutical advancement, effective therapeutics controlling AD are emerging. Nonetheless, due to clinical issues such as poor compliance, management of AD is still challenging. To uncover the burden and clinical management of AD, Dr. Lai Yik Kiu Dominic, Specialist in Dermatology and Venereology, highlighted the current unmet needs and shared his experience in tackling the disease.
The Local Scenario
The prevalence of AD varies in different regions and ethnic populations, whereas the prevalence of adult AD was reported to be 2.6%-6.9% worldwide2. Clinically, AD appears to be most prevalent in children that the prevalence of AD in the first 2 years of life ranges between 7% and 27% in Asian-Pacific countries3. Dr. Lai noted that AD is commonly seen in local clinical practice. “Based on previous report, the local prevalence of AD among pre-school children is around 5.6%, and that in adolescence is about 3.8%4. Of course, there are case of chronic AD or adult-onset AD. However, the proportion would be less than those occur in childhood,” he quoted. He added that a substantial portion of AD patients seeking help from dermatologists suffer from chronic and/or severe disease condition.
The Exacerbating Factors for AD
AD is believed to be triggered by various factors in genetically susceptible individuals. Løset et al (2019) reported the null mutations of the gene encoding filaggrin (chromosome 1q21.3) as the strongest known genetic risk factor for AD, accounting for approximately 75% of heritability. Moreover, former candidate gene studies further identified more than 30 genetic loci linked to AD across different populations. The highlighted genes identified comprise the genes encoding interleukin (IL)-4, the IL-4 receptor, and IL-13, all lying in the Th2 cytokine cluster on chromosome 5q31.15. Dr. Lai stated that the genetic mutations are associated with defects of the epidermal barrier and immunological dysregulation, with the actions of aggravating factors, resulting in the pathogenesis of AD.
There are many exacerbating factors for AD, whereas some of them are unique to AD in either childhood or adulthood. For instance, psychological stress is a common factor associated with adult AD, whereas AD associated with specific foods is predominately associated with paediatric AD6. Dr. Lai highlighted that environmental factors related to seasonal change, such as the increased temperature in summer and the low humidity in winter, would likely trigger AD symptoms. “Moisturised skin and cool weather is preferred. However, sweating, particularly during summer time, would increase the risk of AD,” he noted. In addition, air pollutants, dust mites, and certain irritating chemical agents including soap and cosmetic products may also trigger AD symptoms.
The impact of itch-scratch cycle in AD is noteworthy. Dr. Lai emphasised that scratching is a common but unwanted behaviour among AD patients. The scratch-induced skin damage would result in inflammation worsening of AD. Whereas, ongoing activation of nonhistaminergic sensory nerve fibres by pruritogenic cytokines, chemokines and keratinocyte mediators released on barrier disturbance promotes neurogenic inflammation and sensitisation of nerve fibres. This eventually leads to itch7. While stress is one of the exacerbating factors for AD, Mochizuki et al (2019) speculated that psychological stress increases spontaneous scratching in patients with AD, which may enhance the vicious itch-scratch cycle, resulting in aggravation of AD (Figure 1)8.
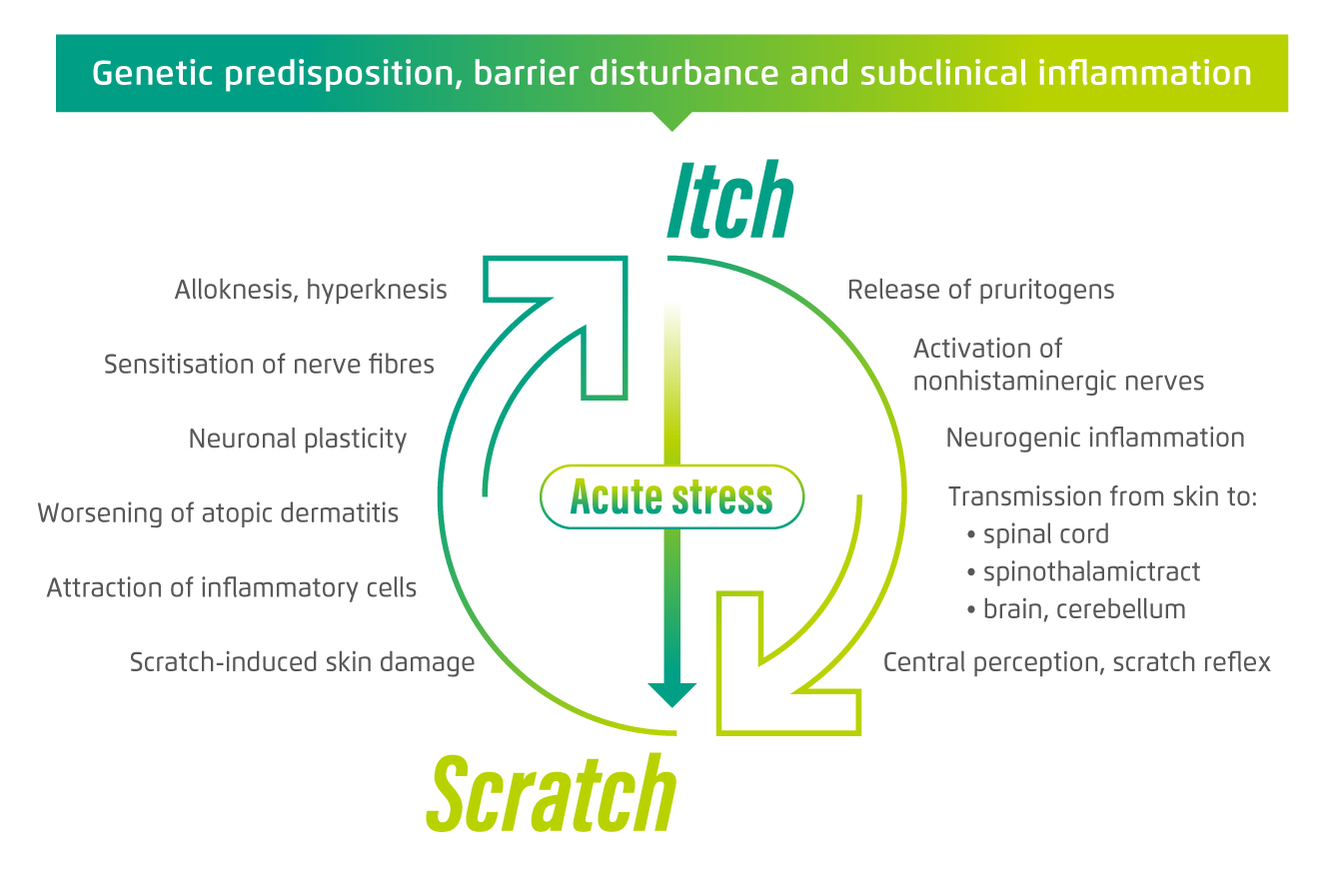
Figure 1. The vicious itch-scratch cycle in AD8
The Substantial Disease Burden
Dr. Lai outlined that pruritus is a predominant symptom of AD. “Dry skins with erythema and itch are commonly observed in AD patients, whereas scratch-related skin erosion occurs in many of the patients as well,” he mentioned.
Dr. Lai further highlighted that the skin lesions observed in AD vary greatly, depending on the severity of inflammation, different stages of healing, chronic scratching and frequent secondary infections. He described that acute lesions are papules and vesicles on a background of erythema, while subacute lesions may develop scales and lichenification. Moreover, chronically involved areas would become thick and fibrotic, and nodules often develop within the plaques. Of importance, patients with a family history of AD, early disseminated infantile disease, female gender and coexisting allergic rhinitis and asthma would be at increased risk of poor prognosis9.
Current evidence suggests that AD is a primary skin barrier defect that facilitates the development of other atopic conditions10. “AD is often an initial step, which may be followed by the sequential development of allergic disease manifestations such as asthma, allergic rhinitis and/or ocular complications,” Dr. Lai stated.
To illustrate the disease burden of severe AD, Dr. Lai described a case of his patient, who was a young man in his 30s, suffered from a severe type of AD known as erythroderma, in which intense and widespread erythema affected greater than 90% of the body surface area, with a variable degree of exfoliative skin scaling11. The AD symptoms of the patient onset since his childhood and persisted into adulthood. During periods of seasonal change, the patient suffered from intense pruritus, which significantly impaired his sleep quality. Extensive skin damage and infection occurred upon scratching, whereas lichenification had developed in various joint areas. “Loss of body temperature is easy in patients with erythroderma, and hence they often feel cold. This condition is in fact very dangerous and stabilisation is urgently needed,” Dr. Lai commented.
More Than a Pathophysiological Problem
AD is often complicated by the manifestation of other diseases. Nonetheless, the adverse impacts of AD are not merely pathophysiological, but can be psychosocial and economical. It has been well-reported that AD-associated sleep disturbance would adversely affect work productivity of adult patients and performance in school of young patients. For instance, a recent survey by Murota et al (2020) revealed that mild AD in Japanese adults resulted in approximately 10% decrease in performance during working hours, while that caused by severe AD was as high as 44%. The annual productivity loss associated with mild AD was estimated to cost about 1.2 trillion Yen12. These findings highlight the huge economic cost of AD for the patients as well as the entire society.
“AD patients generally have lower self-esteem. Even during summer, they would dress up to cover the skin lesions. Also, they would avoid swimming,” Dr. Lai noted. Indeed, AD is known to be associated with social embarrassment, and psychological distress. Notably, Nguyen et al (2016) reported that multiple factors including relationships with parents and classmates, sports participation, and the gender of the patient contribute to the development of self-esteem and identity in AD patients. Briefly, AD was found to have significant behavioral effects on children, ultimately resulting in a lack of opportunity to develop proper coping. Also, the disease had a more-prominent role in identity formation and gender roles in girls13.
Dr. Lai pointed out that AD patients are more susceptible for depressive symptoms, particularly among those with severe AD. His comment aligns with the findings of a population-based study by Schonmann et al (2020) exploring the temporal relationship between AD and new depression or anxiety. The study indicated that adults with AD are more likely to develop new depression and anxiety, whereas a dose-response relationship between AD severity and depression risk was observed (Figure 2)14. Moreover, Dr. Lai added that family members or caregivers of AD patients, especially parents of young patients, would experience substantial psychological distress as well.
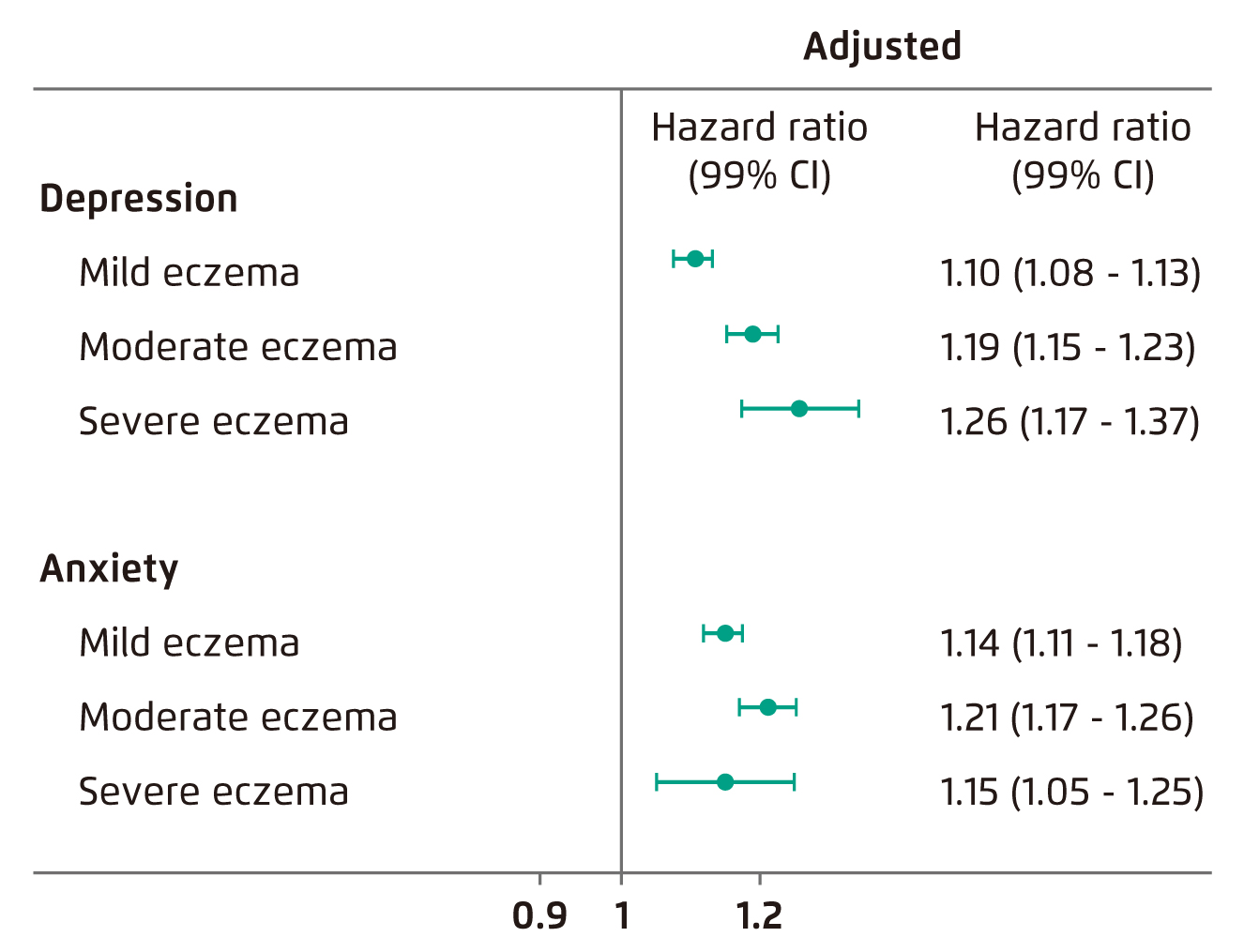
Figure 2. Hazard ratios for the association between AD and depression/anxiety14
In managing AD patients, Dr. Lai reminded that early detection on the impact of AD on patients’ quality of life is crucial. “It would be easy to omit the potential impact on quality of life when one focuses mainly on the skin conditions of patient,” he expressed. To facilitate early detection, he recommended to ask the patients some quick questions during consultation, “it is not necessary to go through a full set of questionnaire, but a few simple questions about their mood and whether they can sleep well can do”. The support from multi-disciplinary team is required in case psychosocial and/or economic problems are detected. He noted that there are local AD patient groups aim to provide supports for the patients and their families.
Clinical Management of AD
There is a wide spectrum of therapeutics available for controlling AD. Dr. Lai outlined that the treatment protocol is decided based on the specific disease severity of the patient. Emollients are recommended to help prevent moisture loss and drying of the skin. For mild-to-moderate cases, topical corticosteroids (TCS) or topical calcineurin inhibitors (TCIs) will be prescribed. In severe diseases or those with skin lesions in face, step up treatment with systemic immunosuppressive agents or phototherapy may be required. Currently, a number of biologic agents targeting the immune pathways involved in AD have been developed and are proven to be effective in controlling AD.
In response to the inquiry on TCS phobia, Dr. Lai commented that the phenomenon is very common in local clinical practice. “AD is a chronic relapsing and remitting disease. Before seeking help from dermatologists, the patients might have consulted some general practitioners or tried various TCS. Side effects or withdrawal symptoms of TCS might have developed already, this contributes to TCS phobia in the patients,” he noted. Former review suggested that TCS phobia is common not only in Hong Kong but across different cultures, with prevalence ranging from 21.0% to 83.7%. The phenomenon is a major contributing factor for nonadherence and hence treatment failure in AD patients15. In tackling TCS phobia, Dr. Lai advised that patient education and selecting the TCS with the appropriate strength for each specific region are essential. Further, sensible decide on the treatment duration for TCS is crucial. In particular, proper communication and explanation on the reasons for the prescribed treatment with the patients are the keys for relieving TCS phobia.
Combating Difficult-to-Treat AD
Former population surveys suggested that the proportion of moderate and severe AD among the total diagnosed cases were approximately 20% and 2%, respectively16. In local clinical setting, there are also AD cases apparently unresponsive to initial treatments with moisturisers and mild potency TCS. In evaluating the potential reasons for treatment failure for difficult-to-treat AD, Arkwright et al (2013) suggested certain medical conditions, including metabolic diseases, as well as skin infection, malignancy, and drug reactions, would potentially be confused with AD16 and hence increase the difficulty for physicians to make correct diagnosis. Besides, despite having a wide spectrum of effective therapeutics for AD of different severity, Dr. Lai addressed that diagnostic tests guiding tailor-made treatment for each specific patient is yet to be available.
Dr. Lai highlighted that patients not complying with treatments or leaving the disease untreated are more susceptible to difficult-to-treat AD. “Thickened and hardened skin is commonly seen in these patients. Their disease condition relapses frequently, and may persist into adulthood”. He added that patients’ compliance to treatment for AD is suboptimal in general. As reported in the International Study of Life with Atopic Eczema (ISOLATE), while majority of AD patients received prescription TCS to treat flares, only 24% of patients and caregivers felt confident they can manage AD flares adequately. 49% of respondents were concerned about using the prescribed treatment17. This highlights the significant impact of TCS phobia in difficult-to-treat AD.
To tackle with difficult-to-treat AD, Dr. Lai emphasised that patient education is essential. “It is common that patients consult another physicians and/or try other therapeutics if significant improvement is not observed upon 2-3 doses of initial treatment. This results in numerous treatments with short durations and hence suboptimal treatment outcome,” he mentioned. Thus, Dr. Lai addressed that another reason for treatment failure in difficult-to-treat AD is the unrealistic expectation on treatment outcome. He added that the mismatch in expectations between patients and physicians would lead to frustration. Therefore, a core component of patient education is to allow patients to understand the disease course of AD and to address the appropriate treatment expectation.
Formulating the Optimal Treatment through Communication and Education
Thanks to the advancement in pharmaceutical science and the better understanding on the pathophysiology of AD, effective therapeutics for controlling AD symptoms are emerging. Nonetheless, management of AD is still a challenging clinical issue. As mentioned, poor compliance and unrealistic expectation on treatment outcome are major reasons for treatment failure. Thus, effective physician-patient communication and patient education are essential in optimising treatment outcome. The support from a multi-disciplinary team would be needed in some cases.
To conclude, Dr. Lai advised that sensible choosing the appropriate therapeutics according to the specific needs and concerns, including financial status, of each patient is essential in improving patient’s compliance. For instance, emollients or lotions with the suitable texture would more easily be accepted by patients. “We, physicians, need to consider from the view of the patients in order to formulate the optimal treatment for them,” he advised.
References
1. Rajagopalan et al. Clin Cosmet Investig Dermatol 2021; 14: 1755. 2. Li et al. Clin Transl Allergy 2021; 11. DOI:10.1002/CLT2.12079. 3. Lopez et al. Dermatol Ther (Heidelb) 2019; 9: 685. 4. Leung et al. Hong Kong J Paediatr 2021; 26: 42-57. 5. Løset et al. Dermatology 2019; 235: 355-64. 6. Murota et al. Allergol Int 2022; 71: 25-30. 7. Ständer et al. Br J Dermatol 2019; 180: 689-90. 8. Mochizuki et al. Br J Dermatol 2019; 180: 821-7. 9. Correale et al. Am Fam Physician 1999; 60: 1191. 10. Kapur et al. Allergy Asthma Clin Immunol 2018; 14: 52. 11. Harper-Kirksey. Life-Threatening Rashes 2018; : 265. 12. Murota et al. J Dermatol 2020; 47: 689-98. 13. Nguyen et al. Pediatr Dermatol 2016; 33: 129-35. 14. Schonmann et al. J Allergy Clin Immunol Pract 2020; 8: 248. 15. Li et al. JAMA Dermatology 2017; 153: 1036-42. 16. Arkwright et al. J Allergy Clin Immunol Pract 2013; 1: 142-51. 17. Zuberbier et al. J Allergy Clin Immunol 2006; 118: 226-32.





