

Specialist in Psychiatry
Cheer Up during Social Unrest
Social movements have become more common around the world in recent years. Large, prosperous cities such as Barcelona, Paris and New Delhi experienced social unrest in 20191. Hong Kong is known for its economic prosperity and the longest life expectancy in the world2. Nonetheless, Hong Kong had been in the spotlight since June 2019 because of the large-scale protests against the bill to establish an official extradition channel to Mainland China and other countries for individuals accused of crime3. The mental health consequences of large-scale population events such as natural disasters, terrorist attacks and epidemics are well documented4, but that triggered by social movements remains largely unclear. To uncover the potential impact of social unrest on mental health, Prof. Char Nie Chen shared his clinical experience and opinions in relieving mental distress.
Social Unrest and Mental Distress
There is a wide spectrum of factors contributing to social unrest. Economic hardship, commodity price shocks, religious beliefs and adverse weather have been associated with civil conflicts, which would be translated into political instability and social unrest5. Prof. Chen suggested that social unrest would be triggered if dissatisfaction towards the society among population is substantial. This is particularly true in a society where people are split by rigid black-or-white ideologies. He added that different people would respond to social unrest in different manners, whether or not they have emotional problems. Besides, he stated that, in macroscopic view, social unrest would adversely impact the economy as demonstrated in a decline in local tourism over recent months. Microscopically, however, social unrest disturbs an individual’s health. “Since the onset of the current social movement, many patients have suffered from insomnia and worries toward future. The stress induced in social unrest would intensify existing health problems,” he noted. Prof. Chen’s opinion agreed with the findings in a recent report which evaluated the association between mental health burden and local social unrest. The study demonstrated that the average proportion of probable depression among the participants during 2009-14 was 1.9%. However, the proportion increased to 6.5% after the Occupy Central Movement in 2017 and further heightened to 11.2% in 2019 before the current unrest. Essentially, the weighted prevalence of depressive symptoms among adults during the current unrest was estimated as 37.4% (Figure 1)1.
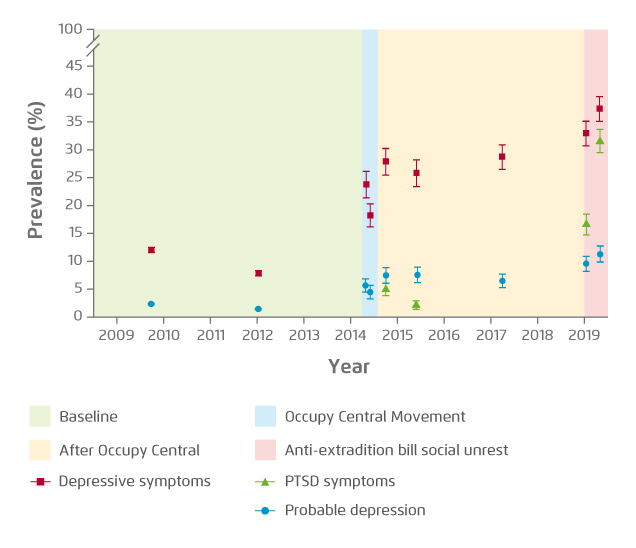
Figure 1. Evolution of mental health before, during and after major unrests1. PTSD: post-traumatic stress disorder
Family stress is defined as any stressor concerning one or more members of the family, or the whole system, at a defined time, which impacts the emotional connection between family members, their mood, well-being, as well as the maintenance of the family relationship6. Prof. Chen highlighted that, in the current incident, family stress would be induced if conflicting political ideologies exist among family members or among friends. However, family stress may also be induced in the absence of conflict. He illustrated with the clinical case of the wife of an active protestor. Her husband was frequently involved in conflicts with the police and her worries triggered mental distress that psychological support and a prescription of sleeping pills, anxiolytics and anti-depressants were needed.
Besides mental distress, Prof. Chen outlined that anger and hostility may increase risk for blood pressure, angina and/or strokes. In reality, violent conflicts can generate physical harm and even death. Thus, the cost of social unrest is significant.
Prof. Chen agreed that the impact of depression is substantial during social unrest. He shared the case of another active protestor who suffered from depression and expressed suicidal ideation. The patient was not satisfied with the current situation in Hong Kong. He was upset towards his own life that he got a job with low salary and therefore, his expectations could not be achieved. He felt no freedom in Hong Kong and hence hoped for a new ideal political system. After realising it was unlikely to accomplish the mission, the patient was in low mood with desperate and suicidal ideation.
Prof. Chen emphasised that physicians have to be neutral and must not rigidly comment on the appropriateness of patients’ thoughts. In case the patient was emotional, counselling should be provided. He outlined the concept of delayed gratification, which is the ability to forgo an immediate reward to gain either better quality or quantity7, and its application in counselling this patient. “If the patient was more flexible and able to accept waiting for a better alternative, his/her distress might be relieved,” he commented.
Risk Factors for Psychiatric Disorders during Social Unrest
Clinically, it would be difficult to identify whether an individual is suffering from psychiatric disorders based on superficial observation. Nonetheless, Prof. Chen highlighted that increased risk for psychiatric symptoms can be congenital and/or environmental, whereas the risk of developing psychiatric symptoms may be associated with unpleasant or traumatic experiences during childhood. He suggested that family stress with the risk of leading to depression or other psychiatric illnesses could also be influenced by unfavourable relationships within the family, between parents, parents and children, or among siblings. Moreover, there are evidences supporting that people who have suffered from child abuse have an increased risk for depression and anxiety8,9. Prof. Chen noted that mental distress can be generated in any stage during one’s life course including studying, career, marriage and interpersonal relationship, depending on how one deals with conflicts and frustrations. A former local prospective study suggested that higher household income, greater psychological resilience, more family harmony, higher family support and better self-rated health appeared to be baseline predictors protected against persistent moderate depression10. This indicates the importance of a flexible and positive approach to any possible negative life stresses.
In evaluating the impact of peers, Prof. Chen commented that peers can have both positive and negative impact on one’s mental condition. “On the negative side, a person might be exposed to friends who use drug/alcohol to forget distressful experiences. He/she may end up in both addictive behaviours and other psychiatric disorders. However, it is also possible that a depressed person interacts with people who could accept and share feelings and offer some lights at the end of the tunnel. They would help relieve the mental stress by providing psychological support and engaging in healthy and meaningful behaviours such as exercises, balanced diets, travelling, or volunteer work,” stated Prof. Chen.
It has been reported that heavy social media use (≥2 hours per day) was associated with both depression and post-traumatic stress during major social unrest1. Of note, there is evidence suggesting that depressed and anxious people tend to be more sensitive to sad faces, adjectives, and emotion-associated words11,12. Further, depressed people typically view ambiguous social interactions as negative13. However, Prof. Chen commented that not only depressed people but also normal people have the preference on “negative” information. Nonetheless, the information would intensify depressive symptoms in depressed people but cause no harm in normal people. He quoted the example of violent movies and traumatic romances in literary work which would not necessarily trigger depression in general public except some psychiatric patients. This is likely because psychiatric patients hold a negative mindset, and the additional stress would reinforce their negative view or amplify their anxiety. “News, literature and other kinds of information only describe the fact of certain incidents, which in fact is neither negative nor positive. The negative impression projected is based on one’s interpretation. It may be worse with anxious or depressed patients as they have already had a negative mindset,” explained Prof. Chen.
Healing the Distressed
Although there are many medications available for treating psychiatric disorders, Prof. Chen addressed that psychotropic medications certainly make patients more comfortable in symptoms unless there are side effects. They also give patients time to reflect on their lives and how to cope with problems. This is why psychological support and treatment are important, especially among those who are very sensitive to drugs or are resistive to taking them. For patients who have difficulties in understanding psychological aspects of their problems, medication treatment can be the only practical way, but treatment outcomes may vary. Hence, Prof. Chen highlighted the importance of both drugs and psychotherapy in helping to change the cognitive mindset and providing a more positive and flexible approach to life problems.
Psychotherapy enables patients to identify the personal factors contributing to their psychiatric problems and to deal with the psychological, behavioural, interpersonal and situational causes. Practically, psychiatrists help the patients identify options for the future and set realistic goals that enable them to enhance their emotional and mental well-being. They also help the patients understand and improve patterns of interacting with other people in order to reduce the risk of mood problems. Further, psychiatrists need to identify negative or distorted thinking patterns contributing to psychiatric problems for the patients as well.
Several meta-analyses demonstrated that psychotherapy is effective in reducing depressive symptom severity14,15. For instance, a recent meta-analysis investigating the neural mechanisms and predictors of response to psychotherapy in depression and anxiety showed that there were significant decreases in anterior cingulate/paracingulate gyrus, inferior frontal gyrus (IFG) and insula activation occurred after therapy (Figure 2), whereas cuneus activation was predictive of subsequent symptom change16. The findings not only illustrated the efficacies of psychotherapy in depression and anxiety, but also addressed the potential neural mechanism of psychotherapeutic response.
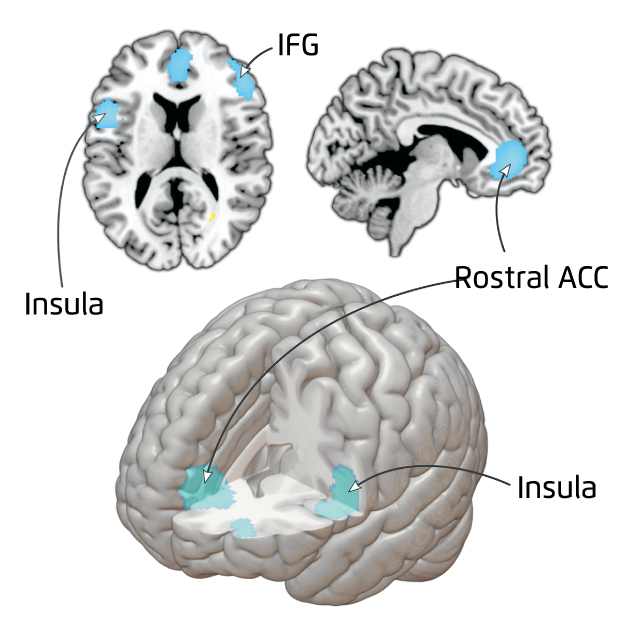
Figure 2. Brain activation change pre-to post-treatment16. ACC: anterior cingulate cortex
Prof. Chen commented that, as much as psychiatrists need to understand the basic concepts of other medical specialities, physicians from other specialties need to do the same in handling patients in their clinics with psychiatric disorders. This is because there is no boundary when patients are suffering from human ailments. For instance, a surgeon needs to have basic knowledge on treating paediatric cases. With the understanding of other specialties, physicians are able to provide advice and referrals to the appropriate specialists. He said that, clinically, many patients in medical clinics may have psychiatric problems since psychiatry is commonly associated with all organ systems and disorders, including acute and especially chronic disorders. Such association may be related to the underlying patho-physiological relationships, but the news of any new disease, more likely than not, often cause certain degree of emotional stress to any healthy person.
Prof. Chen emphasised the importance of communication between physicians and patients. “Physicians need to understand their patients and help them to live healthily and happily in their environments. We may not in a position to dictate the choices of the patients, or stop them from believing that their choices are good for them. However, we could discuss with them whether these choices are healthy or not, or if there are any alternatives. There are many examples of cases, in which we could discuss with patients the healthy lifestyle, habits, the use and abuse of certain medicines or special treatment regimes, the need for certain tests, operation or hospitalisation, sex assignment surgery, sex orientation, etc.,” advised Prof. Chen. Of note, Prof. Chen addressed that the approach for counselling younger patients may be different from that for elderly patients. He further reminded that physicians of all specialties should encourage patients to engage in a healthy lifestyle by gentle persuasion but not to directly ask patients to follow their advice without further explanation. Otherwise, the doctor may be disappointed later to know that the patient did not follow his advice.
Prof. Chen noted that patients may refuse prescribed treatments if they do not trust their doctors. Some may not even take regular medication, but they will not tell their doctors. He said that occasionally there are cases in which he prescribed the same medication for the referred patients as the original physician, but his treatment appeared to yield an expected positive outcome. Prof. Chen’s clue for an effective treatment is the mutual trust established with his patients. Thus, empathy and mutual trust in doctor-patient communication are the key for successful management of psychiatric problems.
Cheer Up the Society and Promoting Mental Health
The current sociopolitical conflict in Hong Kong is complicated and there is no easy solution for the situation. Essentially, the adverse impact of the unrest in terms of psychiatric complications has been reported1. To optimise the health outcomes of psychiatric problem management, effective therapeutics and psychotherapy are required. In addition, collaboration between psychiatrists and physicians of other specialties is crucial.
Besides frontline physicians, the participation of general public is essential in promoting mental health. Although the improvement in understanding mental health care among the local population is significant over past decades, the stigma towards patients with psychiatric symptoms is still substantial. There is also the misguided belief that all psychiatric medications are addictive, or that they should relieve the patients’ psychiatric symptoms as quickly as cold medicines do. But the stigma towards psychiatry as a specialty is also significant, which would directly delay the development of psychiatry as a clinical discipline and indirectly adversely impact the overall health outcomes of all psychiatric patients. Prof. Chen stated that the social support and public donation towards the local department of psychiatry in medical school was less as compared to other clinical departments.
Medicine and psychiatry are clinical disciplines that deal with human organ systems, especially the brain. The former is largely visible and well supported by technologically improved procedures; but the latter is, though invisible, shown in behaviour and in social relationships. Psychiatric disorders can be beyond one’s control just like many medical disorders. But a stable individual often fails to understand the loss of emotional control in a psychiatric patient, or wrongly believes that the patient with a weak character is unwilling to control him/herself and should be told to do so without treatment. Acceptance and support for patients with psychiatric disorders from general public would enable patients see the need to seek help early and hence optimise overall health outcomes. Prof. Chen summarised that all of us should work together to make Hong Kong a better place to live both physically and mentally. The supportive and positive atmosphere in a society not only would facilitate the care and rehabilitation of patients with psychiatric disorders, but also promote a happier society with less social unrest or family violence.
References
1. Ni et al. Lancet. 2020;395(10220):273-284. 2. The World Bank. Life expectancy at birth, total (years) 3. Hou et al. The Lancet Psychiatry. 2019;6(12):982. 4. Goldmann et al. Annu Rev Public Health. 2014;35(1):169-183. 5. Ponticelli et al. J Comp Econ. 2020;48(1):1-19. 6. Clemson et al. Family Stress. In: Encyclopedia of Behavioral Medicine. New York, NY: Springer New York; 2013:771-773. 7. Koepke et al. J Comp Psychol. 2015;129(4):339-346. 8. Ozen et al. Psychiatr Danub. 2018;30(3):340-347. 9. Gallo et al. Child Abus Negl. 2018;79:107-114. 10. Ni et al. Am J Public Health. 2017;107(4):593-600. 11. Lees et al. Cogn Emot. 2005;19(3):453-462. 12. Gotlib et al. J Abnorm Psychol. 2004;113(1):127-135. 13. Kupferberg et al. Neurosci Biobehav Rev. 2016;69:313-332. 14. Fulton et al. J Palliat Med. 2018;21(7):1024-1037. 15. Okuyama et al. Cancer Treat Rev. 2017;56:16-27. 16. Marwood et al. Neurosci Biobehav Rev. 2018;95:61-72.





