
Editor-in-Chief, V·Pulse

Doctor at the National Health Services (NHS), United Kingdom (UK)
Coronary artery disease (CAD) is a significant health challenge, imposing substantial burdens on individuals and healthcare systems worldwide. Notably, in Hong Kong, 1.6% of those aged 15 or above are reported as doctor-diagnosed CAD, with a higher prevalence seen in males (2.1%) compared to females (1.2%). The prevalence increases with age, from 0.1% in those aged 15-24 to 7.7% for those aged 85 or above'. Thanks to the collaborative efforts by researchers, healthcare professionals, and government bodies, advancements in diagnostics, cutting-edge treatment including medications and surgical procedures for CAD are emerging. In addition, a better understanding on the risk factors associated with CAD facilitates more effective lifestyle modifications and cardiac rehabilitation leads to improved patients'outcomes and overall quality of life (QoL).
CAD Remains a Global Health Challenge
Although mortality has decreased in recent decades,CAD remains one of the leading causes of mortality and
morbidity in developed countries. Stark et al. (2024) recently reported that the global age-standardised prevalence of CAD was 3,605 (95% Cl: 2,892-4,454) per 100,000 in 2022, an 18% decrease since the 1990s. Central Europe, and Eastern Europe, as well as Central Asia accounted for the highest agestandardised prevalence of CAD while South Asia having the lowest2.
In Hong Kong, according to the Centre for Health Protection (CHP), CAD accounted for 58.8% of heart disease-related deaths in 2020, whereas the age-standardised death rates due to CAD accounted for 30.5 in male and 11.9 in female per 100,000 standard population. Align with the global trend, a gradual decrease in age-standardised death rate of CAD was observed since 1981 (Figure 1)1. 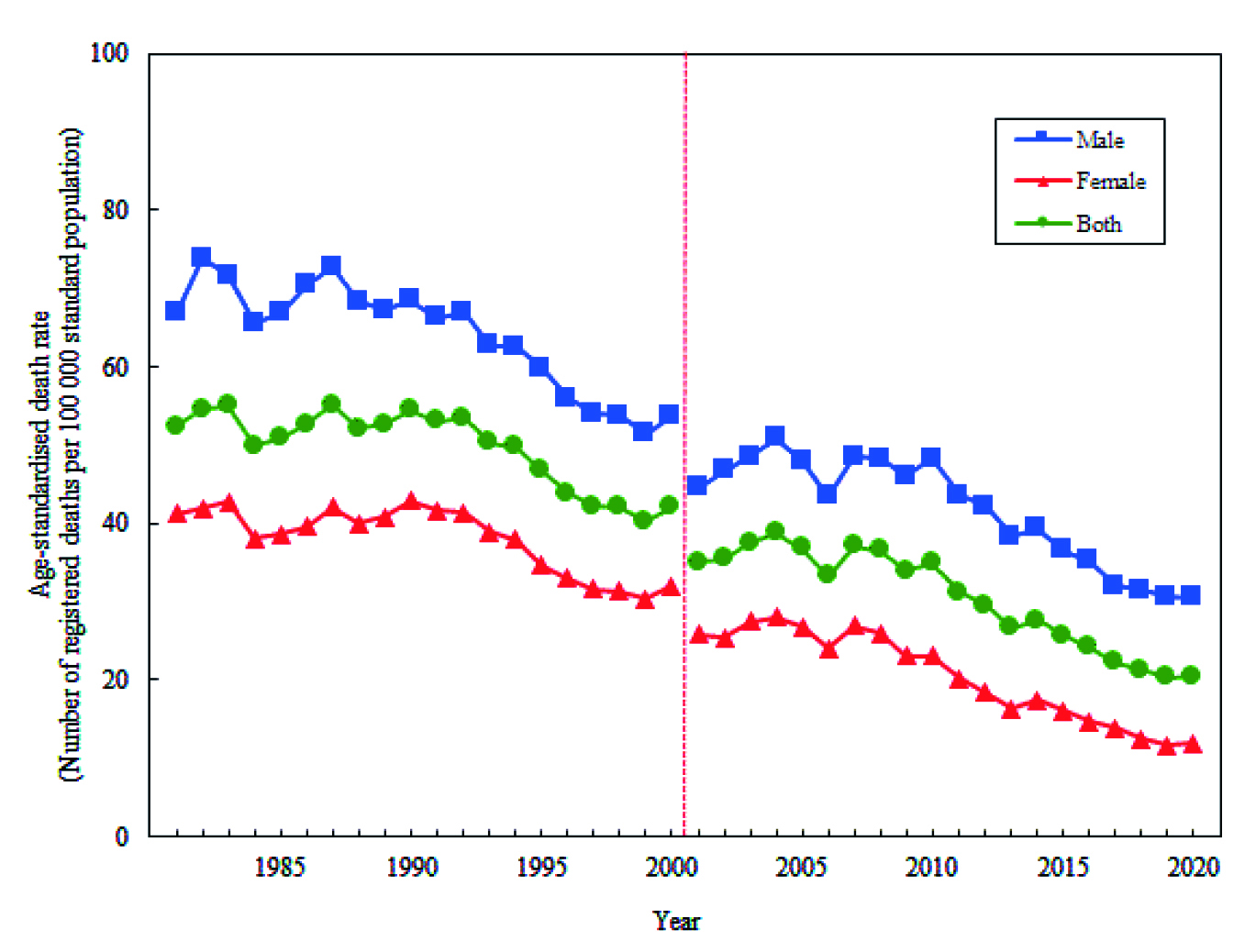
Figure 1. Local age-standardised death rate of CAD by sex, 1981-20201
While CAD potentially leads to adverse cardiovascular (CV) events, such as myocardial infarction (Ml) and stroke, the economic burden of CAD is undoubtedly substantial, which includes direct costs on hospitalisation and medication, as well as the loss of productivity. For instance, a local study involving 89 patients with newly diagnosed stable CAD by Lee et a/. (2013) reported that the mean first-year total direct medical cost of newly diagnosed stable CAD per patient was US$11,477 (HK$89,521). Hospitalisation accounted for 29.2% of the total cost. The results further highlighted that the total cost for patients who underwent invasive coronary procedure was significantly higher than those treated medically alone (HK$115,339 vs HK$47,744, p<0.001)3. Thus, implementing preventive measures of CAD and cost-saving strategies are essential.
Be Aware of the Psychosocial Risk Factors of CAD
It is well-established that non-modifiable intrinsic「isk factors, including age, sex, family history, and ethnicity are associated with the development of CAD. In contrast, lifestyle habits, such as physical activity, amount of good-quality sleep, dietary patterns, and smoking behaviour, are considered as modifiable factors for CAD4. Controlling these risk factors may help lower the risk of developing heart disease and may improve the overall health and wellbeing.
Aside from physiological and lifestyle risk factors, the role of psychosocial factors in relation to the development of CAD is also noteworthy. Albus (2010) evaluated the effects of psychosocial factors such as low socio-economic status, lack of social support, stress at work and family life, depression, anxiety, as well as hostility has on the risk of developing CAD as well as clinical course and prognosis of the disease5. Remarkably, it was reported that the psychosocial risk factors may actually hinder treatment adherence and impede the efforts to control modifiable lifestyle risk factors6.
A meta-analysis of 23 reports included 4,628 CAD and 3,002 stroke events recorded in 16 longitudinal datasets by Valtorta et al. (2015) revealed that loneliness and social isolation
were associated with a 29% increased risk of CAD and a 32% increased risk of stroke, regardless of the gender7. The findings reflected the magnitude add on effects of loneliness and social isolation has on individuals'health, in addition of predisposing them to CAD. Accordingly, interventions targeting psychosocial risk factors for preventing CAD are warranted.
Key Topics under the Management of CAD
The holistic management of CAD should cover various aspects including diagnostic technologies, application of medications, surgical procedures, preventive measures, research on emerging therapies, interdisciplinary collaboration, long-term outcomes with follow-ups, as well as lifestyle mod巾cations and cardiac rehabilitation (Figure 2)8. Among these, innovative diagnostic techniques for early detection and risk assessment, effective medications, and advanced surgical treatments are particularly crucial for improving the overall outcomes of CAD patients.
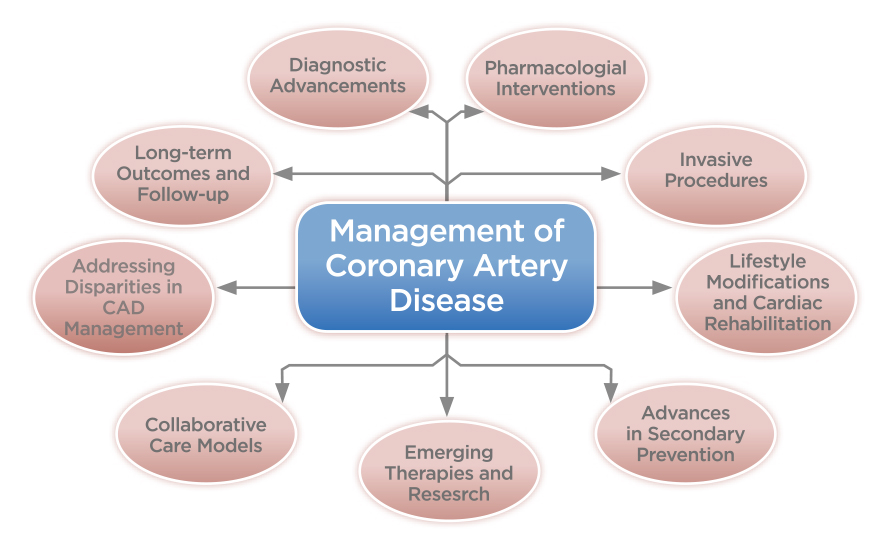
Figure 2. Key issues in the management of CAD8
Cardiac computed tomography angiography (CCTA) is a noninvasive alternative to invasive coronary angiography (ICA) primarily used to evaluate coronary anatomy. CCTA allows rapid determination on the presence of coronary plaque and triage patients'that require further invasive evaluation and treatment, with high positive and negative predictive values9.
Notably, patients with previous coronary artery bypass grafting (CABG) often require ICA, which is technically more challenging and incurs a higher risk of complications. In the BYPASS-CTCA trial (2023), undergoing CCTA before ICA was demonstrated to significantly reduce the procedure time of ICA and contrast-induced nephropathy, with improved patient satisfaction, compared to ICA alone. Furthermore, there was a significant reduction in incidence of 1-year major adverse cardiac events (MACE) in the CCTA+ICA group compared with the ICA group (Figure 3)10
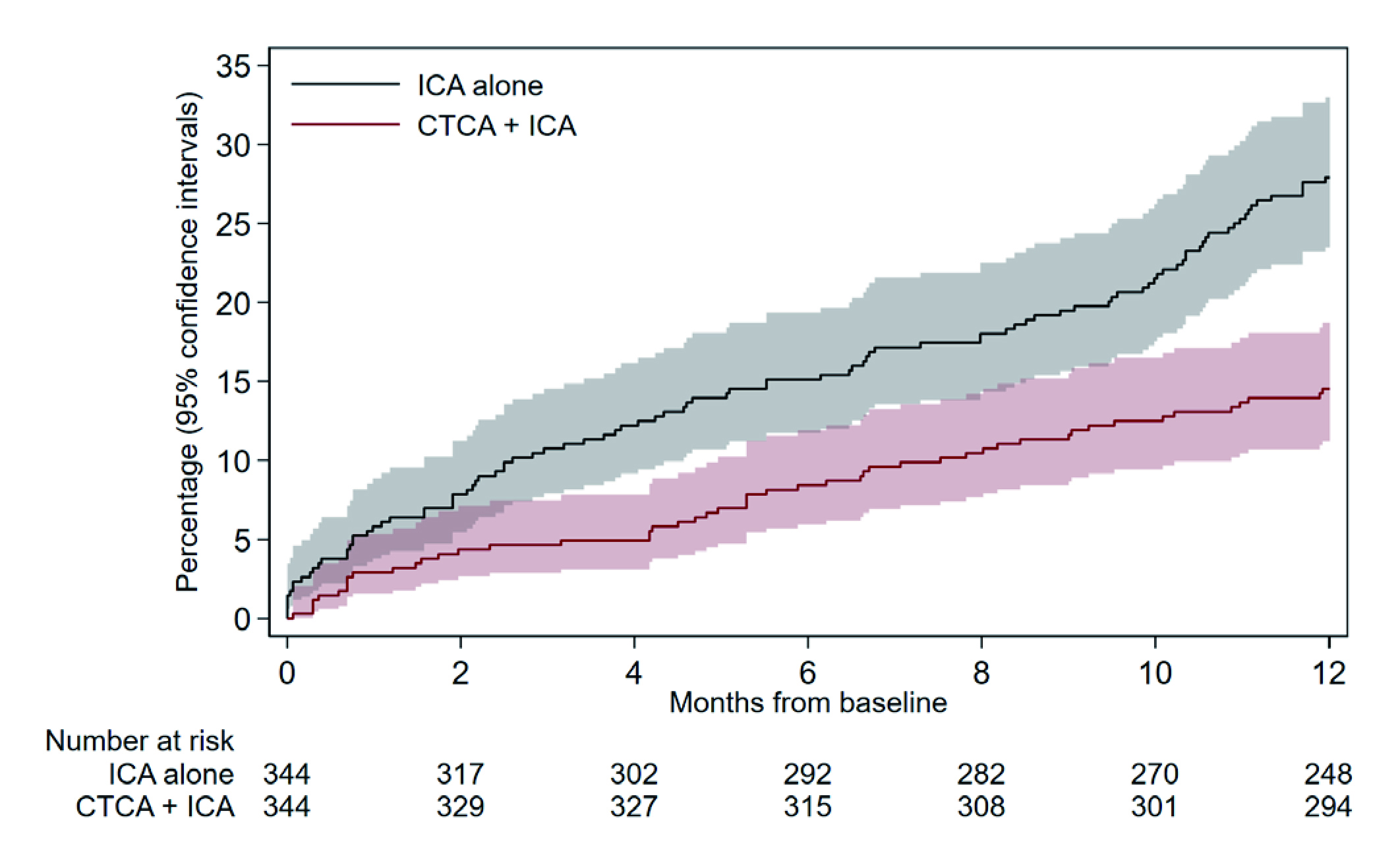 Figure 3. MACE at 12 months in BYPASS-CTCA trial10
Figure 3. MACE at 12 months in BYPASS-CTCA trial10
Besides non-invasive imaging techniques, biomarkers have emerged as promising tools for early CAD diagnosis and
risk assessment. A recent analysis of 3,072 CAD patients by Netto et al. (2022) suggested that plasma levels of troponin T, N-terminal pro B-type natriuretic peptide (NT-proBNP), copeptin, high-sensitivity C-reactive protein (hsCRP), and interleukin-6 (IL-6) showed a significant association with total mortality, whereas the levels of the biomarkers varied at different stages of CAD. Hence, incorporating the biomarker during diagnosis will likely enables fast and precise non- invasive identification of mortality risk in CAD patients,
thus, allowing the tailoring of primary and secondary CAD prevention11.
Personalised risk profiling encompasses genetic testing and risk assessment tools, which facilitates precision medicine in CAD management. Uncovering the genetic variants associated with the risk and treatment responses allows for tailored treatment strategies catering individual patient needs主Interestingly, Zhou et al. (2024) recently developed a risk prediction model for recurrent cardiovascular (CV) events among Chinese patients. The model included a list of 125 risk variables, such as clinical laboratory tests and disease and medication history, which were used to help predict the risk of CV disease (CVD), of which 8 classes of CVD-related drugs were considered interactive covariates立The risk prediction model is expected helpful in identifying individuals at high risk of CAD, thereby enabling timely intervention and preventive measures.
The Cutting-edge Pharmaceuticals against CAD
The conventional medication treatment for stable CAD patients consists of beta blockers, calcium channel blockers, nitrates, angiotensin converting enzyme (ACE) inhibitors, and statins8. However, novel therapies for CAD have been emerging in recent years. Importantly, the use of a clopidogrel, a P2Y12 inhibitor, in patients with an acute coronary syndrome (ACS) is also well established.
In the HOST-EXAM Extended study (2023), clopidogrel monotherapy for long-term maintenance after percutaneous coronary intervention (PCI) was demonstrated to yield lower rates of a composite of all-cause death, non-fatal MI, stroke, re-admission attributable to ACS, and Bleeding Academic Research Consortium (BARC) type 3 or greater bleeding than aspirin after a median follow-up of 5.8 years13.
Apart from P2Y12 inhibitors, maintaining a lower low-density lipoprotein cholesterol (LDL-C) is established to reduce the risk of atherosclerotic cardiovascular disease (ASCVD), and long-term maintenance of lower LDL-C is recommended by clinical guidelines for those at greatest risk of future ASCVD-related events14. In this regard, when statins are not tolerated or cannot be prescribed, proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibition was used to reduce the levels of LDL-C. For instance, the findings from the ORION-3 trial revealed that long-term treatment with inclisiran reduced LDL-C levels by 47.5% and the reduction was sustained over 4 years among patients at high CV risk (Figure 4)15.
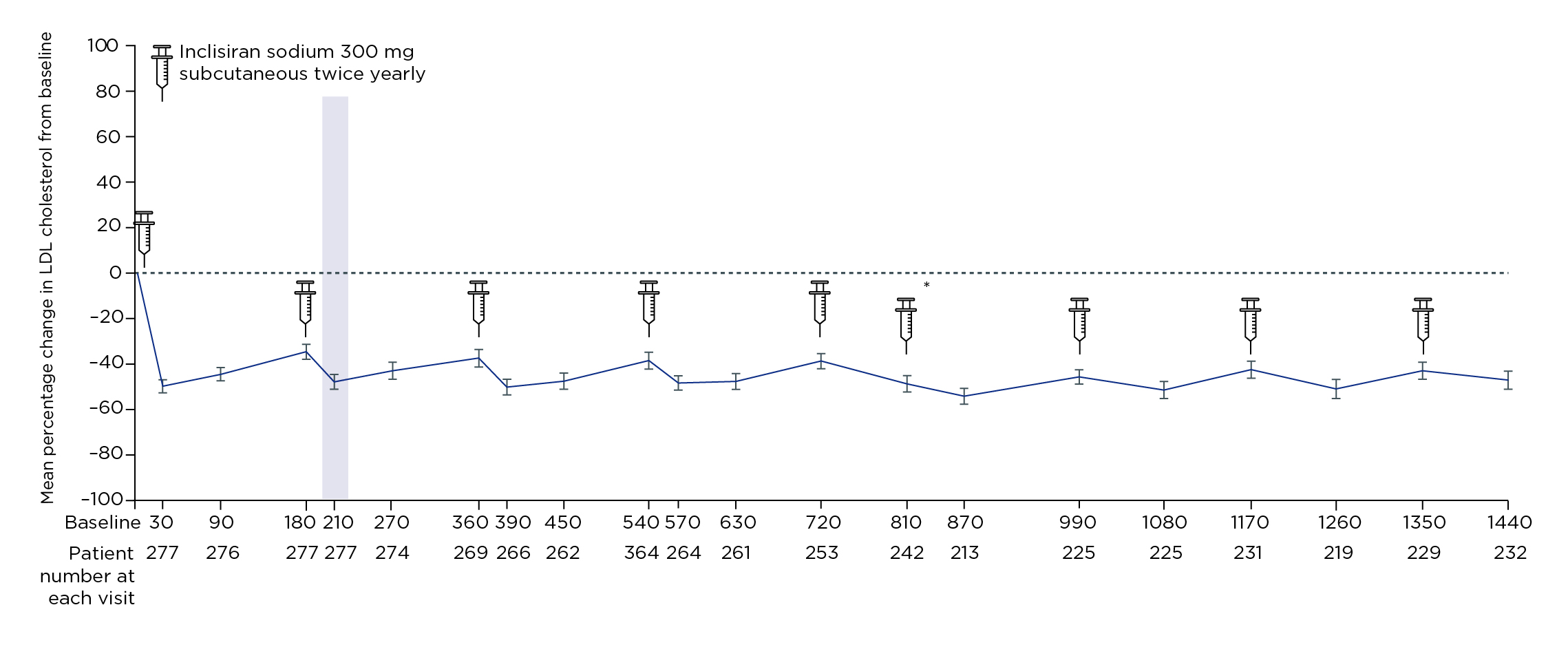
Figure 4. Mean percentage change in LDL-C from baseline to day 1440 (4 years) yielded by inclisiran15
On the other hand, the 5-lipoxygenase (5-LO) pathway is responsible for the production of leukotrienes that have inflammatory and vasoactive actions and are involved in the innate immune response, whereas FLAP (5-lipoxygenase activating protein) is critical for the production of leukotrienes16. Hence, the inhibition of 5-LO or FLAP was hypothesised to reduce mortality, morbidity, and cardiovascular hospitalisation in patients with CAD by slowing the progression of atherosclerosis, to enhance coronary microvascular function, and to improve ventricular contractility following MI17. In the phase 2a FLAVOUR trial, AZD5718, a FLAP inhibitor, was demonstrated to reduce leukotriene biosynthesis in patients with recent MI and was well-tolerated18.
While new medications against CAD are slowly emerging, recently, the focus on primary and secondary prevention of CAD has shifted towards optimising the patient treatment outcomes, for instance, the use of single antiplatelet therapy (SAPT) reducing CAD risk.
Life-saving Innovative Surgical Treatments
From the initial application in improving visualisation with enhanced endoscopic camera control to the recent robotic surgical systems which permit the manipulation of surgical instrument through limited thoracic incisions, robot-assisted technology has revolutionised surgical procedures in cardiology.
A retrospective analysis by Lin et al. (2021) compared the outcomes of conventional coronary-artery bypass grafting (C-CABG) and robot-assisted CABG (R-CABG) using the Da Vinci robotic operation system in patients with multi-vessel CAD (n=516) suggested that in-hospital and long-term mortalities were lower in the R-CABG group. However, the incidences of target lesion revascularisation (TLR), target vessel revascularisation (TVR), MI, and stroke were not significantly different between the two groups. The study thus concluded that R-CABG could be an effective alternative to C-CABG for multi-vessel CAD patients with fewer clinical complexities in real-world practice19.
In addition to enhancing precision, robot-assisted technology also allows tele-operation. The clinical operation of tele-stenting was illustrated in the REMOTE-PCI study (2017). During the operation, a physician operator performed stenting on a patient in a separate physical location using a combination of robotics and telecommunications. Among the 20 participating patients, procedural success, i.e. <30% residual stenosis upon completion of the surgery in the absence of death or repeat revascularisation before discharge, was achieved in 19 (95.0%) patients20.
The robot-assisted surgical procedures not only benefitted patients for improving treatment outcomes and minimising the risk of complications, but it also lowered the burden for frontline physicians by reducing exposure to occupational radiation and orthopaedics hazards17.
Besides the advancement in surgical procedures, innovation in treatment instruments is also remarkable. Drug-coated balloons (DCB), designed to administer anti-proliferative agents to coronary lesions without the use of a metallic stent, have emerged as a potential alternative to drug-eluting stent (DES), combining the advantage of local drug release during balloon angioplasty without the long-term disadvantage of DES, including impaired vessel motility and increased risk of late thrombosis21.
A recent randomised control trial (RCT) involving 600 patients with in-stent re-stenosis undergoing percutaneous coronary intervention (PCI) by Yeh et al. (2024), target lesion failure was significantly lower in the paclitaxel-coated balloon group (17.9%) compared with the uncoated balloon group (28.6%, p=0.003). Also, ischemia-driven TLR and target vessel MI were also lower after treatment with a paclitaxel-coated balloon22. The results thus highlighted that DCB was superior to an uncoated balloon with respect to the composite end point of target lesion failure and was an effective treatment option for patients with coronary in-stent restenosis.
The Advancements in the Era of Artificial Intelligence
The rapid progress of artificial intelligence (Al) has created new opportunities to improve the interventional workflow in managing CAD. While image acquisition is crucial for guiding coronary intervention, Al has been applied to improve imaging quality while reducing artifacts and the radiation dose. For example, convolutional neural networks (CNN) architecture has been applied for restoring images from low-dose computed tomography (CT) images (Figure 5A-5C)23.
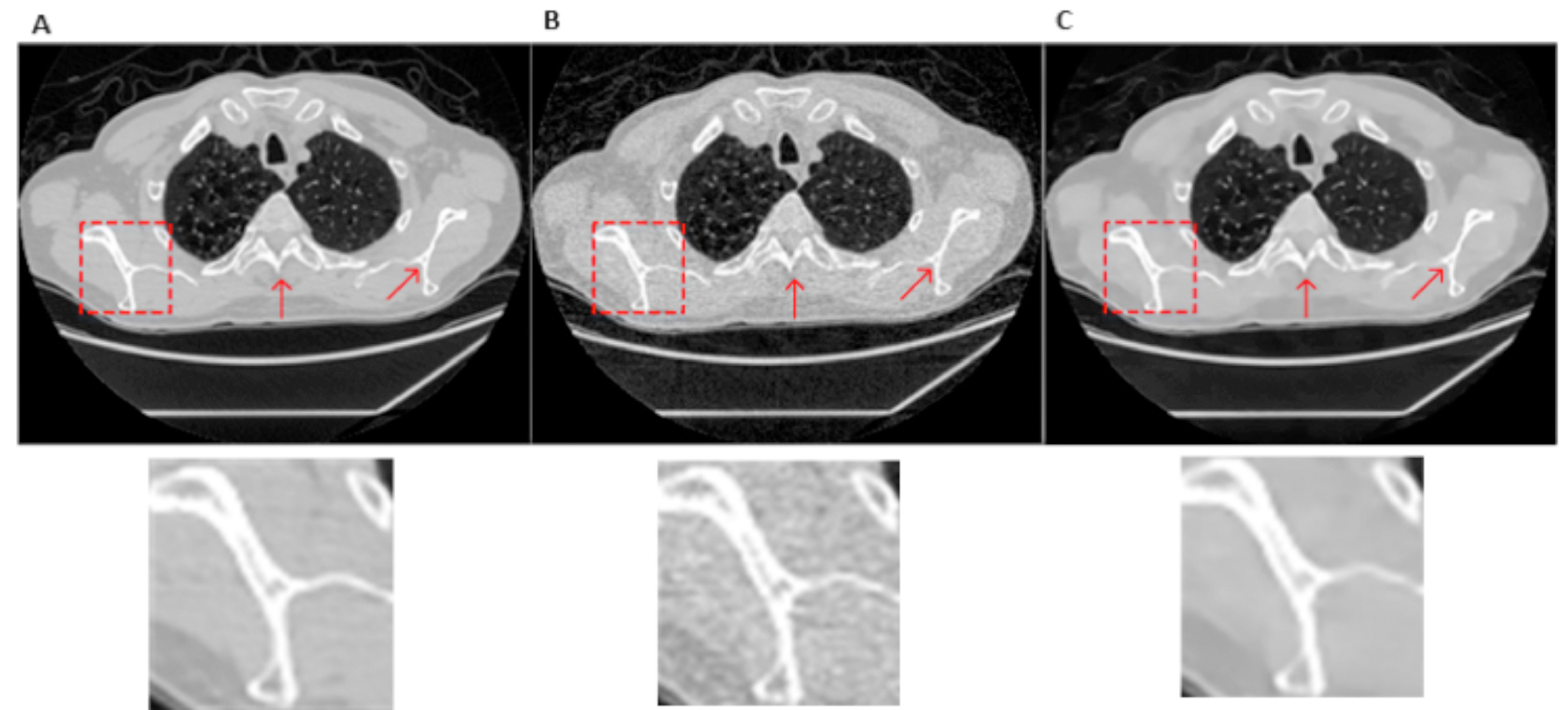
Figure 5. Restoring chest CT image with the specific zoomed regions within the red box23, A) normal dose image, B) low-dose image, C) CNN-processed image
In view of diagnosis and risk stratification, deep learning (DL) models have proven excellent performance in the diagnosis of stenosis using dedicated CNN architectures. Interestingly, Du et al. (2021) trained a DL model based on a dataset of 20,612 angiograms, in which 13,373 angiograms were labelled with coronary artery segments, and 7,239 were labelled with special lesion morphology. The DL model was reported to predict coronary artery segments with an accuracy of 98.4%, and the recognition sensitivity was 85.2%. Importantly, the model took only 2 seconds for the automatic recognition24. With the exceptional diagnostic performance, the DL architecture provides a coronary diagnostic map and is expected to help cardiologists to flag and diagnose lesion severity and morphology during the intervention.
Given that intravascular imaging post-stenting is indicated to evaluate the result after stent deployment, some DL models have been developed for rapid and automatic quantification of stent expansion and apposition. Yang et al. (2021) developed a DL method to automatically analyse stents with both thin (s0.3mm) and very thick tissue coverage (>0.3mm), and an algorithm to accurately analyse stent area for vessels with multiple stents. Three-fold cross-validation demonstrated that the algorithm achieved a precision of 0.932 and a sensitivity of 0.939 for stents with thin tissue coverage, and a precision of 0.856 and a sensitivity of 0.874 for stents with very thick tissue coverage (Figure 6A-6C)25.
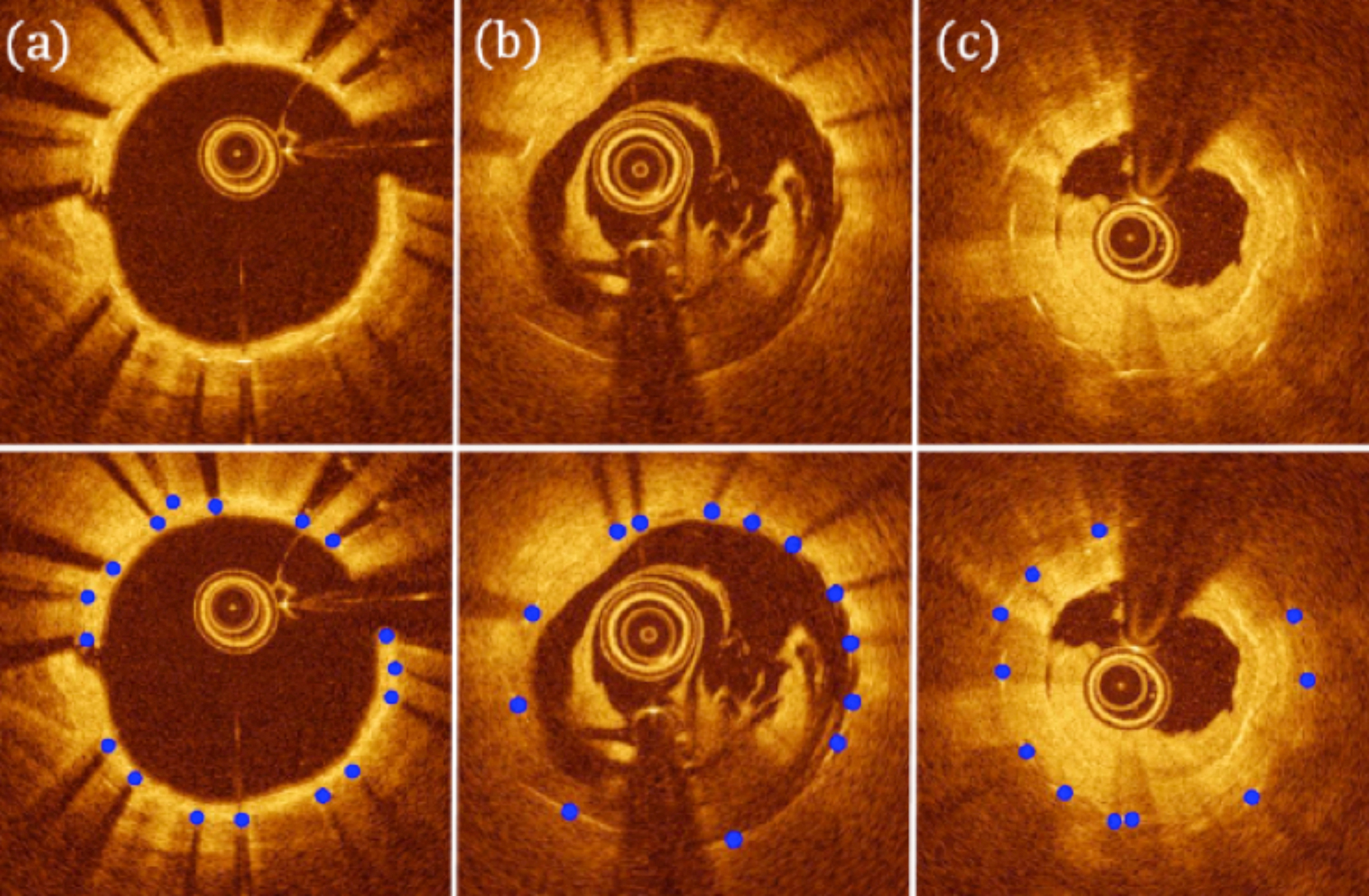
Figure 6. Stent detection results by the proposed algorithm: the top row shows original images and the bottom row illustrates the corresponding detected stent struts25, A) clear lumen with thin-medium tissue coverage, B) significant residual luminal blood, C) thrombus and very thick tissue coverage
Based on the results, the method can facilitate the evaluation of stent implantation and post- stent tissue coverage.
Although there are still limitations of DL and unaddressed challenges ahead, advanced DL algorithms open new opportunities for precise diagnosis and tailored treatment in cardiology with a high degree of automation, reduced radiation, and enhanced risk stratification. Vitally, the technology is expected to benefit patients by optimising treatment outcomes.
Shaping the Future of CAD Management
The recent advancements in diagnostic methods and therapies have significantly reduce the burden of CAD.
Our better understanding on the pathophysiology of the disease facilitates the development of effective medications and personalised treatment, whereas the use of Al not only enhance the efficiency in clinical operation, but also help physicians overcome technical difficulties during surgical treatments. While the innovations undoubtedly have revolutionised the landscape of clinical management of CAD, the role of education on healthy lifestyle remains crucial. Prevention is always the most important yet is most often overlooked. Therefore, clinicians should empower their patients to take control of their health and manage their disease holistically.
References
1. Centre for Health Protection - Heart Diseases. https://www.chp.gov.hk/en/healthtopics/content/25/57.html. 2. Stark et al. J Am Coll Cardiol 2024; 83: 2320. 3. Lee et al. Heart Asia 2013; 5: 1. 4. Coronary Heart Disease - Causes and Risk Factors | NHLBI, NIH. https://www.nhlbi.nih.gov/health/coronary-heart-disease/causes. 5. Albus. Psychological and social factors in coronary heart disease. Ann Med 2010; 42: 487–94. 6. Rozanski et al. J Am Coll Cardiol 2005; 45: 637–51. 7. Valtorta et al. Heart 2016; 102: 1009–16. 8. Bansal and Hiwale. Cureus 2023; 15. DOI:10.7759/CUREUS.50644. 9. Widmer et al. Journal of the Society for Cardiovascular Angiography and Interventions 2024; 3. DOI:10.1016/j.jscai.2024.101301. 10. Jones et al. Circulation 2023; 148: 1371–80. 11. Netto et al. Nutrients 2022; 14. DOI:10.3390/NU14163433/S1. 12. Zhou et al. European Heart Journal - Digital Health 2024; 5: 363–70. 13. Kang et al. Circulation 2023; 147: 108–17. 14. Virani et al. Circulation 2023; 148: E9–119. 15. Ray et al. Lancet Diabetes Endocrinol 2023; 11: 109–19. 16. Pettersen et al. J Med Chem 2019; 62: 4312–24. 17. de Oliveira Laterza Ribeiro et al. Life 2023, Vol 13, Page 951 2023; 13: 951. 18. Prescott et al. Int J Cardiol 2022; 365: 34–40. 19. Lin et al. Medicine 2021; 100: E23830. 20. Madder et al. EuroIntervention 2017; 12: 1569–76. 21. Sciahbasi et al. Journal of Clinical Medicine 2024, Vol 13, Page 1320 2024; 13: 1320. 22. Yeh et al. JAMA 2024; 331: 1015–24. 23. Li et al. Biomedical Optics Express, Vol 8, Issue 2, pp 679-694 2017; 8: 679–94. 24. Du et al. EuroIntervention 2021; 17: 32–40. 25. Yang et al. Biomed Opt Express 2021; 12: 7500.
Answers for CME quiz of Feature Story of Issue 24: 1.B, 2.B, 3.D, 4.C, 5.D





