Advancement in Diagnostic Imaging for Early Detection of Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is the most common malignant tumour of the liver, whereas patients with HCC are often unaware of its presence until the tumour has progressed to an advanced stage, and no more than 40% are cured surgically1. Thus, HCC is generally associated with unfavourable prognosis that the overall 5-year average survival rate is less than 10%2. This highlights the clinical importance of early detection of HCC. Nowadays, accurate diagnoses for HCC patients can be done with imaging techniques including contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI). However, early detection, especially those involving small lesions, remains challenging. Nonetheless, recent advancement in imaging technology and instrumentation optimises the diagnosis of HCC and hence improves health outcomes for HCC patients.
Performance of Conventional CT and MR Imaging
Dynamic multiphase contrast-enhanced CT and MRI are the current standard tests for imaging diagnosis of HCC. The presence of arterial enhancement of a nodule sized 2 cm or more with subsequent washout on portal or delayed phases are considered to be the definitive imaging features of HCC3. The reported per-lesion sensitivity of contrast-enhanced MRI for nodular HCC of all sizes ranged between 77-100%, while that of CT is 68-91%. However, as the diagnostic performance is highly dependent on tumour size, the sensitivity drops to around 45-80% (MRI) and 40-75% (CT) for HCC of 1-2 cm and lower for lesions smaller than 1 cm4. Hence, the sensitivity of standard CT and MRI is yet to satisfy the clinical requirements for detecting small HCC lesions.
The Era of Dual-tracer PET/CT
Positron emission tomography (PET) is a well-established diagnostic imaging technique playing a major role in the diagnosis and staging of many malignant tumours. 18F-fluorodeoxyglucose (FDG) is one of the most commonly used metabolic probes for PET evaluation. FDG enters living cell membranes through glucose transporters and is phosphorylated to 2-deoxyglucose-6-phosphate, which is then trapped within tumour cells. The increased glucose consumption in dividing cells in tumour lesions leads to enhanced incorporation of FDG. Nonetheless, probably due to the high dephosphorylation rate of 2-deoxyglucose-6-phosphate by glucose-6-phosphatase, which is strongly expressed in liver and in well-differentiated HCC, the retention of FDG within HCC lesions is reduced5. Therefore, the sensitivity of FDG PET in detecting HCC ranges only between 36% and 70%1.
In recent years, dual-tracer PET/CT with FDG and 11C-acetate (ACT) has shown to be useful in evaluating primary and metastatic HCC. Practically, ACT was complementary to FDG in detection of primary HCC. The HCC tumours that were not detected by FDG were visualised with ACT. This phenomenon occurs as a result of the pattern of tracer uptake by HCC that ACT is preferentially accumulated in well-differentiated HCC, whereas FDG tends to be uptake by poorly differentiated lesions6. The difference in FDG and ACT uptake by HCC is illustrated in Figure 1.
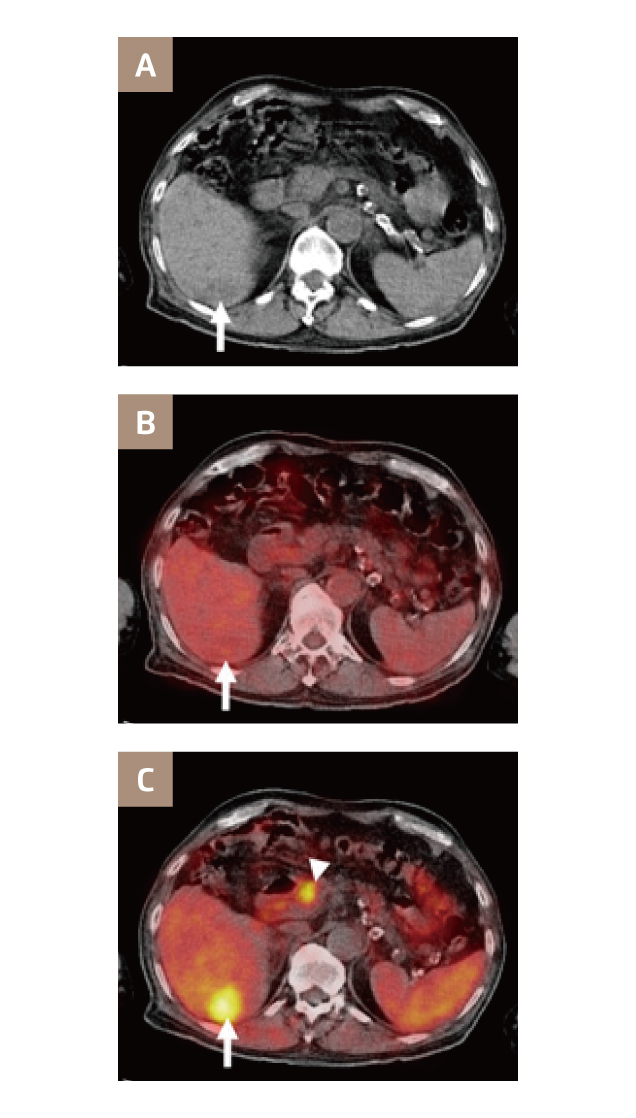
Figure 1. Transaxial PET/CT images of a patient with HCC. (A) Unenhanced CT image shows hypoattenuating lesion in right lobe (arrow), (B) FDG PET/CT, and (C) ACT PET/CT shows focally increased uptake of ACT in tumour (arrow) and physiologic ACT uptake in pancreas (arrowhead)7
A clinical trial comparing the performance of various PET/CT modalities involving 112 patients, 99 of them with HCC, demonstrated that the overall sensitivities of FDG, ACT and dual-tracer PET/CT in the detection of primary HCC lesions were 60.9%, 75.4%, and 82.7%, respectively. In addition, the results further showed that the overall sensitivities of FDG, ACT, and dual-tracer PET/CT for metastatic HCCs were 85.7%, 77.0%, and 85.7%, respectively7. The findings thus suggested that dual-tracer PET/CT with FDG and ACT increases the overall sensitivities for identifying HCC lesions and thus benefits the management of HCC.
Enhanced Diagnostic Value of Gadoxetic Acid-enhanced MRI (EOB-MRI)
Gadoxetic acid is a liver-specific contrast medium modified with a lipophilic ethyl-oxy-benzyl (EOB) group, which is actively uptake by hepatocytes. Essentially, HCC lesions do not accumulate gadoxetic acid due to the absence of an organic anion transporting peptide. This leads to hypo-intensity in the hepatobiliary phase (HBP) comparing to the enhanced normal liver parenchyma and hence improves detection rates of lesions8.
The major advantage of EOB-MRI is the improved detection of small lesions, ≤2 cm, compared with contrast-enhanced MRI or CT9,10. In a comparison between EOB-MRI and multiphasic CT (MDCT) in differentiating small HCC from arterial-enhancing pseudolesion (AEP) in cirrhotic liver, EOB-MRI yielded sensitivity higher than 90.9%, which was significantly higher than that yielded by MDCT (54.5%, p=0.001, Figure 2). Essentially, among the 44 HCC lesions examined, only 2 showed iso- or high signal intensity during HBP of EOB-MRI11. This indicates the high specificity of EOB-MRI in identifying small HCCs.
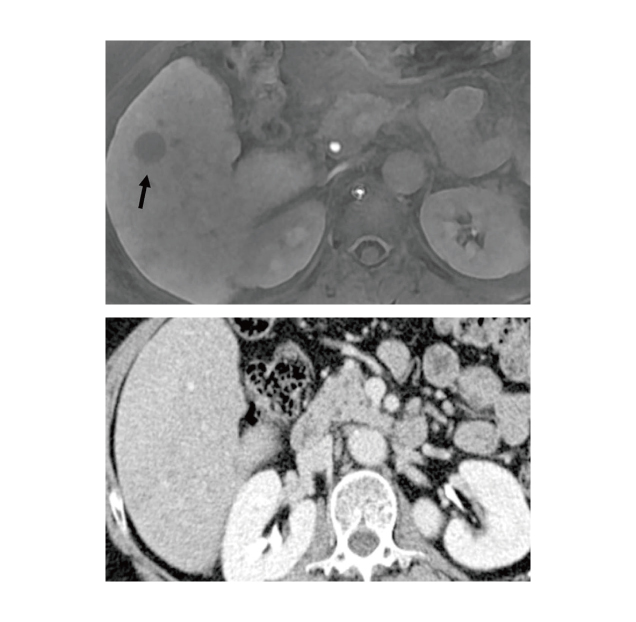
Figure 2. Images of hepatitis B liver cirrhosis, (A) EOB-MRI during HBP showing a 1.3 cm HCC (arrow) and (B) MDCT scan during delayed phase shows the lesion with iso-intensity to liver parenchyma11
Moreover, EOB-MRI would facilitate physicians in making appropriate diagnosis and clinical decisions. For instance, Jin et al (2016) analysed the incidence of change in liver cancer staging determined by liver dynamic CT after EOB-MRI. The results revealed that 22 of 166 patients (13.3%) had their tumour stage changed after EOB-MRI; change from BCLC stage 0 to A in 18 cases and from stage A to B in 4 cases12. Therefore, EOB-MRI would facilitate accurate cancer staging especially for early stage diseases.
Of importantly, in addition to the enhanced detection sensitivity, a remarkable advantage associated with EOB-MRI is that the imaging technique does not involve radiation. Both PET and CT components of PET/CT comes with significant radiation doses. Hence, PET/CT is not suitable for routine HCC screening purpose, whereas MRI would be an excellent option for patients.
Step Ahead - Combined Dual-tracer PET/CT and EOB-MRI
While the clinical applications of FDG PET/CT in cancer diagnosis have been well-established, dual-tracer PET/CT with FDG and ACT improves the sensitivity of tumour detection. Besides, Oh et al (2016) demonstrated that add-on EOB-MRI significantly improved the detection of liver metastasis with nodules smaller than 2 cm as compared to FDG PET/CT alone (sensitivity: 95.1% vs. 59.8%, p=0.0001)13. Hence, with the reported advantages of EOB-MRI in identifying small HCC lesions, combined scanning with dual-tracer PET/CT and EOB-MRI is expected to provide comprehensive imaging information allowing early and accurate diagnosis for HCC, which in turn optimises overall HCC management.
References
1. Lu et al. World J Gastroenterol. 2019;25(32):4682-4695. 2. Wang et al. J Hematol Oncol. 2019;12(1). 3. Hennedige and Venkatesh. Cancer Imaging. 2012;12(3):530-547. 4. Kim et al. AJR Am J Roentgenol. 2006;186(1):149-157. 5. Filippi et al. Expert Rev Med Devices. 2019;16(5):341-350. 6. Ho et al. J Nucl Med. 2007;48(6):902-909. 7. Park et al. J Nucl Med. 2008;49(12):1912-1921. 8. Fahlenkamp et al. PLoS One. 2019;14(3):e0213408. 9. Guo et al. Abdom Radiol. 2016;41(10):1960-1972. 10. Kierans et al. Radiology. 2016;278(1):82-94.11. Sun et al. Invest Radiol. 2010;45(2):96-103. 12. Jin et al. J Surg Oncol. 2016;114(1):106-111. 13. Oh et al. Biomed Res Int. 2016;2016.





