

Doctor at the National Health Services (NHS), United Kingdom (UK)

Doctor at National Hopsital Service (NHS), United Kingdom (UK)
The Challenging Nature of Rosacea
Rosacea is a common chronic inflammatory disease that presents with recurrent flushing, erythema, telangiectasia, papules, or pustules affecting the centrofacial region (cheeks, chin nose, and forehead) and the eyes1. There are four clinical subtypes of rosacea: erythematotelangiectatic, papulopustular, phymatous and ocular. It is important to note that these subtypes are not mutually exclusive and patients may present with features of multiple subtypes2. Interestingly, rosacea usually starts between the ages of 30 to 50 years but may occur at any age groups. Moreover, the global prevalence of rosacea is estimated to be at 5.5% in adult population, affecting both males and females equally1. Approximately 50-75% of patients with rosacea also have ocular symptoms which include dryness, redness, tearing, tingling/burning sensation, foreign-body sensation, light sensitivity, and blurred vision. Apart from the eye symptoms, rosacea may cause anxiety, and depression, which can have detrimental effects on patient’s quality of life (QoL)2. Furthermore, rosacea is also associated with a wide range of systemic diseases such as neurologic diseases, inflammatory bowel disease (IBD), and cardiovascular disease (CVD)2. Notably, rosacea is not an exclusive disease of fair-skinned individuals, instead, it also occurs in individuals with dark-skin, but is often misdiagnosed in these individuals. To understand more on rosacea and the psychosocial impact it has on patients, we have invited Dr. Lynden Christian, one of the clinicians at the NHS, UK to discuss the real clinical challenges faced in diagnosing, particularly in dark-skinned individuals and the holistic treatment approach taken in clinical practice.
Rosacea, a Dark Knight Under the Skin
Rosacea is a chronic inflammatory skin disorder which is prevalent in fair-skinned individuals with a lower predilection for darker skin individuals. Despite this, patients with skin of colour, the characteristic manifestations of rosacea can be masked, thereby making diagnosis significantly challenging3. This may then leave these individuals vulnerable to the disease, thus delay in initiating appropriate treatment and negatively impact their QoL3. The manifestation of rosacea in dark-skinned individuals was explored in a study by Al-Balbeesi et al., (2014) involving 50 patients with different skin complexions (type 4 [light brown], type 5 [brown], type 6 [dark brown or black]) who were diagnosed with rosacea. The mean age of all patients was 42.2 years with mean duration of the disease of 6.1 years4. 18% of participants had a family history of rosacea and the results demonstrated that patients with skin type 4 comprised of 50% of severe erythematotelangiectatic rosacea compared to skin type 6 (42.9%). However, authors concluded that the severity of rosacea was not significantly associated with the specific skin types, instead the condition is equally common in darker-skinned individuals with clinical presentation similar to those seen in fair-skinned individuals4.
Similarly, Dlova et al., (2017) performed an 8-year retrospective chart review of patients with a clinical and histological diagnosis of rosacea or acne rosacea. Among 6,700 patients, 15 (0.2%) had rosacea and all were of African descent with skin types 5 or 65. Surprising, females were predominantly affected by the conditions compared to males (14:1 ratio)5. In regard to these reported findings, Dr. Christian reminded us that rosacea is not limited to fair-skinned individuals and a high index of suspicion should be there which may help diagnose the condition in dark-skinned individuals5. He further elaborated that since rosacea is reported less frequently in dark-skinned individuals, this may be the result of the delayed diagnosis or late presentation due to the difficult in discerning the classical features of erythema or simply due to the lack of awareness of rosacea in dark-skinned individuals6. Thus, additional clues in the medical history and clinical examination may further assist in making the diagnosis. In addition, the recommendation from the National Rosacea Society Expert Committee and global ROSacea COnsensus (ROSCO) panel in 2017 advocated topical and systemic antibiotics as first-line treatment for rosacea7. In relation to the management of rosacea, Dr. Christian suggested that minocycline being most effective with low risk of adverse effects in treating papules and pustules in patients with rosacea.7
Psychosocial And Financial Burden of Rosacea
More than 16 million individuals in the United States (US) are diagnosed with rosacea with around 1.67 million outpatient visits reported between October 2011 and September 20128. Locally, rosacea is common, but data on the actual prevalence remains elusive9. Notably, the goal of current therapies is to manage the clinical signs and the physical symptoms of the disease, but the impact of rosacea on patients’ emotional health and QoL is sometimes overlooked8. In view of this, Dr. Christian advocated to consider physician to explore patient’s self-perception prior to prescribing a treatment regimen. He further added that the clinical severity often does not correlate with the level of psychosocial distress experienced by the patient. These findings have also been documented in literature which suggested that 65.1% of patients with rosacea who had a comorbid psychiatric diagnosis also had a diagnosis of depression8. More interestingly, a survey conducted by the National Rosacea Society (NRS) with more than 400 patients suffering with rosacea reported lower self-esteem at a rate of 75%. In addition, majority of respondents reported their condition made them felt embarrassed (70%), and frustrated (69%). Astonishingly, more than 50% of respondents felt being robbed of pleasure or happiness because of rosacea8.
Dr. Christian explained that patients with rosacea are often affected by the social stigmas as some of them are being viewed as alcoholics or as having a poor physical hygiene. He shared findings from one of the surveys conducted by Kelton Research which evaluated patients’ self-perception and the perception of others regarding patients with rosacea. The online perception survey contrasted images of females with and without rosacea. More than 1,000 members of the general population and 502 females with rosacea completed the online survey between the October 29th, 2009, and November 9th, 2009. The survey found that females with rosacea were perceived to be more insecure, not as healthy, not as intelligent, and not as successful when compared to females with clear skin. Furthermore, respondents with and without rosacea had a negative first impression of females with rosacea8. Apart from the psychosocial burden, rosacea also carries a significant economic burden as skin diseases accounted for 96 billion US dollars (USD) in 2004. The financial impact of rosacea was explored further by a study performed by Beikert et al., (2013) involving 475 patients with rosacea to determine their willingness to pay for their treatment. Among the participants, 79.9% were females with a mean age of 56.3 years and when questioned on the percentage of their monthly income they would pay for their condition, more than half (60.3%) of the patients reported that they would invest 0% to 10% of their monthly income towards rosacea, and 28.3% expressed that they were willing to invest 10% to 20% of their monthly income. Surprisingly, only 11.4% of the participants expressed that they were willing to invest more than 20% of their monthly income for rosacea treatment and this group of participants were mainly females ages between 21 to 30 years10. These findings suggests that patient who feel rosacea being a major burden affecting their QoL were willing to spend more on the treatment to achieve complete healing8. Dr. Christian reminded us that in clinical practice, only a small percentage of patients with rosacea will seek professional advice and treatment8. Therefore, physicians should keep that in mind and always consider the psychosocial aspect of the disease by simply listening to their patients.
A Misunderstood but Sinister Medical Condition
Rosacea is a common, serious skin disorder which is underrecognised and undertreated as it affects 1 in every 10 individuals in the US according to the American Academy of Dermatology11. Dr. Christian reminded us that despite this relatively high incidence, the diagnosis of rosacea is often delayed or never made which results in needless suffering for many patients. He further added that the rosacea is associated with a wide range of medical condition, including the inflammatory bowel disease (IBD)12. In fact, Li et al., (2023) reported both Crohn’s disease (CD) and ulcerative colitis (UC) being associated with an increased risk of rosacea13. Thus, clinicians should remain vigilant in diagnosing skin disorders in patients with IBD since early diagnosis and initiation of treatment early can make a significant difference to a patient’s QoL, according to Dr. Christian.
The relationship between IBD and rosacea was also demonstrated in a systematic review and meta-analysis by Jun et al., (2023) in IBD patients to determine the associated between rosacea and IBD12. Eight eligible studies were included in the meta-analysis and analysis suggested that prevalence of rosacea was higher in IBD group compared to the control group (odd ratio [OR] 95% confidence interval [CI]: 1.52-2.26]. Interestingly, both CD and UC groups had a higher prevalence of rosacea with ORs of 1.74 (95% CI: 1.34-2.28) and 2.00 (95% Cl: 1.63-2.45), respectively (Figure 1)12. Surprisingly, those with rosacea also had an elevated risk of developing IBD (both CD and UC) with an incidence rate ratio of 1.60 (95% CI: 1.33-1.92), and 1.26 (95% CI: 1.09-1.45), respectively. The conclusion drawn from the study suggested IBD has a bidirectional relationship with rosacea12. In regard to these findings, Dr. Christian suggested that since both rosacea and IBD share pathogenesis, particularly both having an autoimmune basis, it is not surprising to see this bidirectional relationship between the two. Furthermore, the changes in immune responses (innate and adaptive immune systems) and microbiome dysbiosis are often documented in both rosacea and IBD; therefore, the changes in the gut-skin axis may play a significant role in the development of these conditions12. In conclusion, Dr. Christian advocated clinician to take appropriate medical history, perform a thorough clinical examination, particularly in those where the diagnosis of rosacea can easily be overlooked.
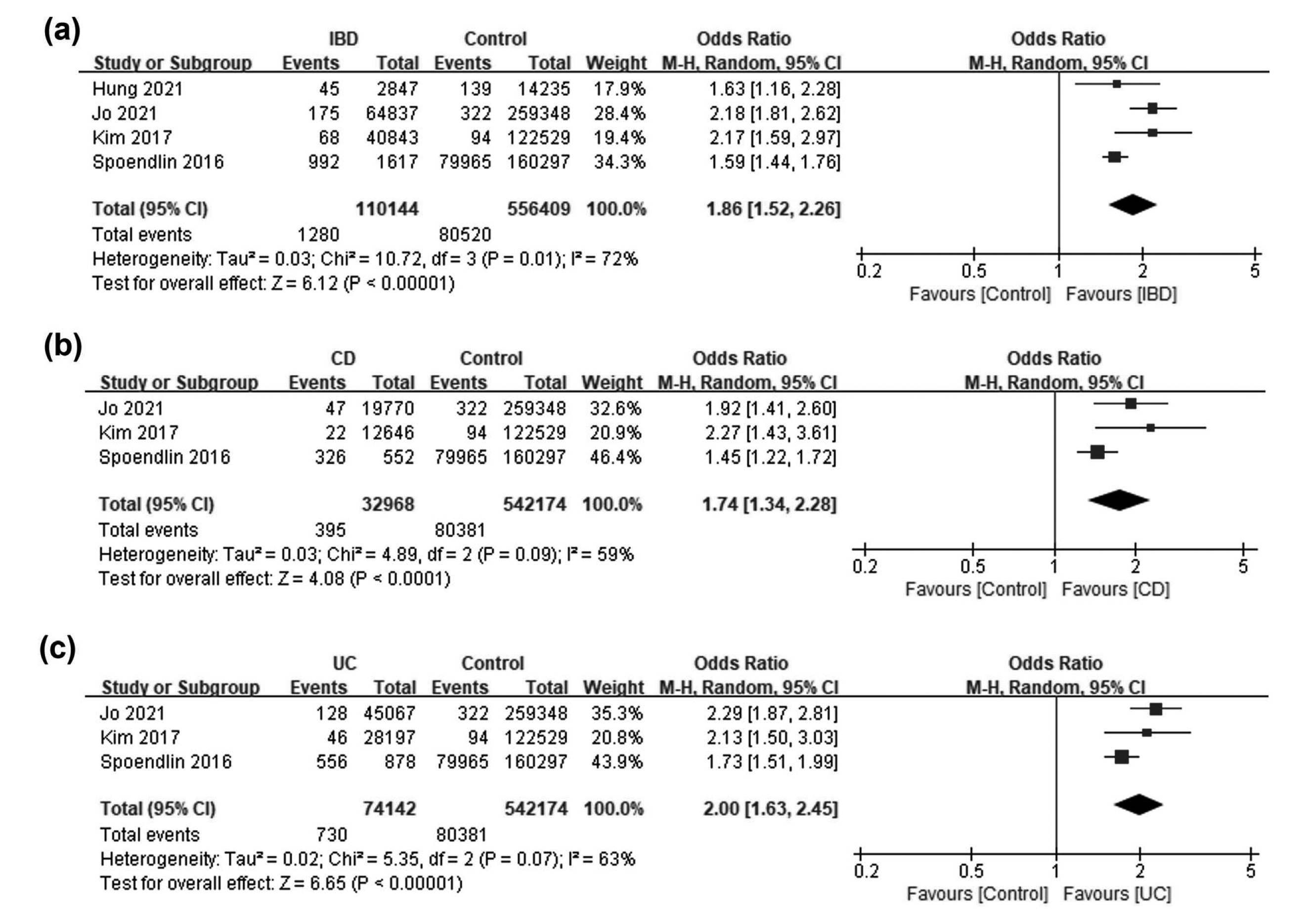
Figure 1. Patients with (a) inflammatory bowel disease (IBD), (b) Crohn’s disease (CD), and (c) ulcerative colitis (UC) had a higher prevalence of concomitant rosacea compared to the control. M-H= Mantel-Haenszel; CI= confidence interval; df= degrees of freedom12.
References
1. van Zuuren EJ et al. Am J Clin Dermatol 2021; 22(4): 457-65. 2. Farshchian M et al. Rosacea. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. 3. Maliyar K et al. Drugs Context 2022; 11. 4. Al Balbeesi AO et al. Ochsner J 2014; 14(3): 321-7. 5. Dlova NC et al. Clinical and Experimental Dermatology 2017; 42(6): 670-3. 6. Maruthappu T et al. Clinical and Experimental Dermatology 2022; 47(2): 259-63. 7. Xiao W et al. Front Pharmacol 2023; 14: 1169916. 8. Huynh TT. Am Health Drug Benefits 2013; 6(6): 348-54. 9. Yeung Wai-Man LC et al. The Journal of the Hong Kong College of Family Physicians 2019; 41(3): 77-84. 10. Beikert FC et al. J Eur Acad Dermatol Venereol 2013; 27(6): 734-8. 11. Helwick C. Rosacea: A Misunderstood, Serious Medical Condition. 2021. 12. Jun YK et al. Dermatol Ther (Heidelb) 2023; 13(7): 1465-75. 13. Li M et al. Sci Rep 2023; 13(1): 14910.





