
The Devastating Effects of Acne Scars
Acne is a very common skin condition with a prevalence of around 80% seen in young adults. Moreover, atrophic scars are a common complication, accounting for up to 11% of acne vulgaris cases and often have a devastating effect on the patient’s psychosocial life1. Globally, around 9.4% of the world’s population is affected by acne vulgaris2, and it causes a substantial burden by negatively increasing the anxiety levels of sufferers3. Therefore, an effective atrophic acne scar treatment is desirable and may change the quality of life of sufferers. Currently, a wide range of techniques are utilised to improve acne atrophic scars, such as subcision, punch technique, chemical peeling, dermabrasion, laser, and trichloroacetic acid application1. However, there has been a recent application of skin needling, a collagen induction therapy that utilises microneedles to puncture skin superficially, triggering new collagen synthesis1. Moreover, microneedling is a novel, minimally invasive treatment which requires minimal training and is simple, safe, and effective, according to the literature. To understand the concept behind microneedling and its use in acne atrophic scars, we shall first unravel the pathophysiology behind the cause of acne atrophic scars and its psychosocial impact on individuals suffering from acne vulgaris.
Acne Vulgaris, an Evil Entity Lurking Under Our Skin
Acne vulgaris is a chronic inflammatory disorder that affects the pilosebaceous unit, typically following a prolonged course. It is commonly triggered by Cutibacterium acnes (C.acnes), a bacterial species in adolescence4. The condition commonly manifests with papules, pustules, or nodules primarily on the face, although it can also affect the upper arms, trunk, and back. But what triggers acne, and why is it common in adolescence? Acne develops as a result of hypersensitivity of the sebaceous gland to normal levels of circulating androgens. This process is further exacerbated by C. acnes, which then triggers skin inflammation. Obviously, there are other triggering factors, which include drug-induced acne (lithium, steroids, and anticonvulsants), exposure to excess sunlight, oil-based cosmetics, endocrine disorders (polycystic ovarian syndrome), and psychological stress, which stimulates stress hormones4.
Adolescents are prone to acne, particularly males, but this pattern changes post-adolescent as acne predominantly affects females4. Notably, acne affects adolescents at a time when they are transitioning through both physical and social changes; therefore, it can have a profound negative effect on their mood and psychosocial well-being. Furthermore, the combined effects of acne and the resulting scarring or pigmentation (hyperpigmentation) may lower their self-esteem or cause depression/anxiety5. Then what causes these atrophic scars? The answer to this is inflammation, which is a key component of the pathogenesis of acne atrophic scars. At the adrenarche, there is a spike in the level of adrenal dehydroepiandrosterone output that increases sebum production and keratinocytes in susceptible follicles. Of note, increased sebum excretion is associated with more severe acne and more inflammatory lesions. In fact, the clinical hallmarks of acne are seborrhoea, inflamed lesions known as papules, pustules (≤5 mm in diameter), and nodules (>5 mm in diameter), open comedones known as blackheads, and closed comedones, also known as whiteheads5. The result of acne is often scarring, which can present as atrophic scarring secondary to loss of tissue or raised hypertrophic or keloid scars due to excessive tissue development5. So, how can acne be managed? An accurate assessment of the severity of acne is often challenging since many grading systems have been adopted, with only a few of them being validated. Generally, during the assessment, the site affected, the extent of acne, the number of lesions, the degree of seborrhoea, and inflammation are all taken into consideration. Nonetheless, clinicians are also encouraged to take psychological sequelae into consideration during the assessment by using relevant health-related quality of life (HRQoL) measures5.
Paradigm Shift in Management of Acne Scarring
The early preclinical inflammation related to acne persists throughout the acne lesion’s life cycle, from micro-comedones to closed comedones, followed by inflammatory lesions, which eventually cause erythema, hyperpigmentation, and finally scarring6. The scars are a mere result of altered wound healing response to cutaneous inflammation, with inflammatory cell infiltrates found in 77% of atrophic scars. So, what are these atrophic scars? Are they contagious? Atrophic scars are aberrant production and degradation of collagen in the dermis, leading to atrophic scar formation. In fact, the atrophic scars are classified according to their depth and size of destruction, as illustrated in Figure 16.
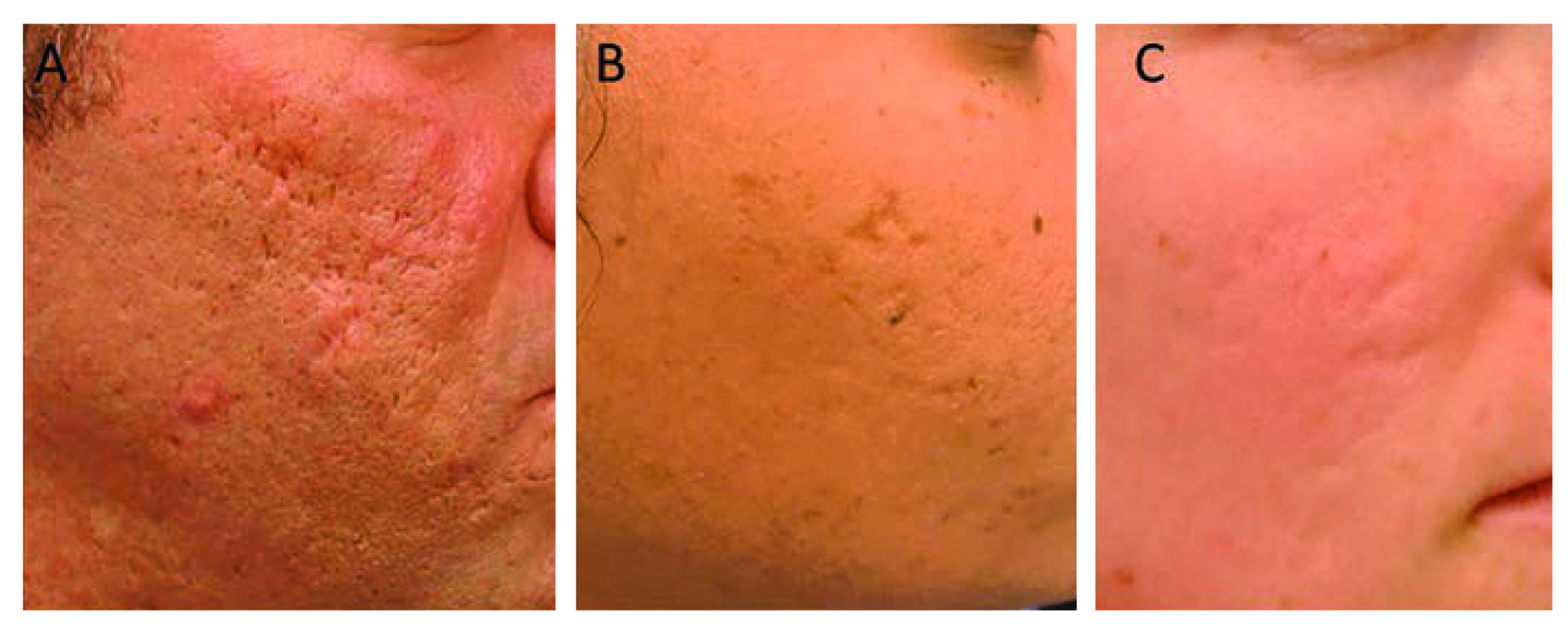
Figure 1. the three types of atrophic acne scars: A. Icepack (comprises 60-70% of atrophic scars and are narrow, V-shaped epithelial tracts deep to the dermis), B. Boxcar(20-30% of atrophic scars that are wide, round-to-oval depressions with sharply demarcated vertical edges), and C. Rolling (15-25% of atrophic scars that are widest with fibrous anchoring of the dermis to the subcutis resulting in superficial shadowing and an undulating appearance of the scar)6.
Traditionally, the treatment of acne scars involves targeting erythema if present. Once this is addressed, the focus is shifted towards addressing the atrophic scarring with an approach dictated by the types of scars present and whether generalised or individual scars are predominant. The scar-associated erythema (SAE) can be successfully treated by pulse dye laser (PDL) or other laser devices6. On the other hand, generalised atrophic scars are treated through a wide range of clinical applications, which include lasers, chemical peels, dermabrasion, and, more recently, with microneedling.
Microneedling, An Effective Alternative Scar Rejuvenating Partner
Acne scars are often distressing with negative effects on the quality of life. Even though a variety of approaches are applied during the treatment phase, a less invasive and effective way is often preferred by patients with acne scars7. Even though literature has supported laser treatment as being the most effective treatment for acne scarring, the adverse events experienced by patients can be debilitating. Patients post-laser procedure may experience pain, infection, erythema, post-inflammatory hyperpigmentation (PIH), hypopigmentation and further scarring8. Then what about microneedling? How different is it from the other available treatments for atrophic acne scars? Is it effective in all types of acne scarring, and how safe is it? To answer all these questions, we first need to understand what microneedling entails. Microneedling is a simple technique which helps the body build new collagen layers and thus is considered an alternative to all erosive techniques, such as those used in laser or chemical skin peeling9. The skin responds to fine punctures by releasing the growth factor. Studies have shown that the procedure is safe, and cost-effective, with minimal complications compared to other available treatments9.
As we are aware, acne has long been deemed a self-limiting disease, common in adolescents. Furthermore, the atrophic scars not only bring changes to the skin but also limit daily life and self-esteem, which may predispose individuals to anxiety and depression9. Recent studies has shown that needles break collagen bundles in the superficial layer of the dermis that are responsible for scars with subsequent induction of more collagen immediately forming under the epidermis10. Even though a wide range of studies have looked at the clinical results of microneedling, most are often dependent on the subjective estimate by the physicians according to a prospective clinical study performed by El-Domyati et al., (2015), who evaluated the clinical effect and objectively quantified the histological changes of acne scarring in response to skin microneedling in patients with acne scars. Ten patients with different types of atrophic acne scars were subjected to three months of skin microneedling treatment (six sessions at two-weeks intervals), followed by histometry and biopsies for epidermal thickness and quantitative evaluation of total elastin, newly synthesised tropoelastin, collagen types I, III, VII10. The results obtained were remarkable, as noticeable clinical improvement in atrophic post-acne scars was reported post-microneedling (Figure 2) with a statistically significant increase (p<0.05) in the mean of collagen types I, III and VII and newly synthesised collage (Figure 3), whilst a significant reduction in total elastin (p<0.05) at the end of the treatment.

Figure 2. Photographs of patients with post-acne scars in response to skin microneedling therapy showing clinically noticeable improvement after one month of treatment, which continued to improve after three months of treatment when compared to baseline10.
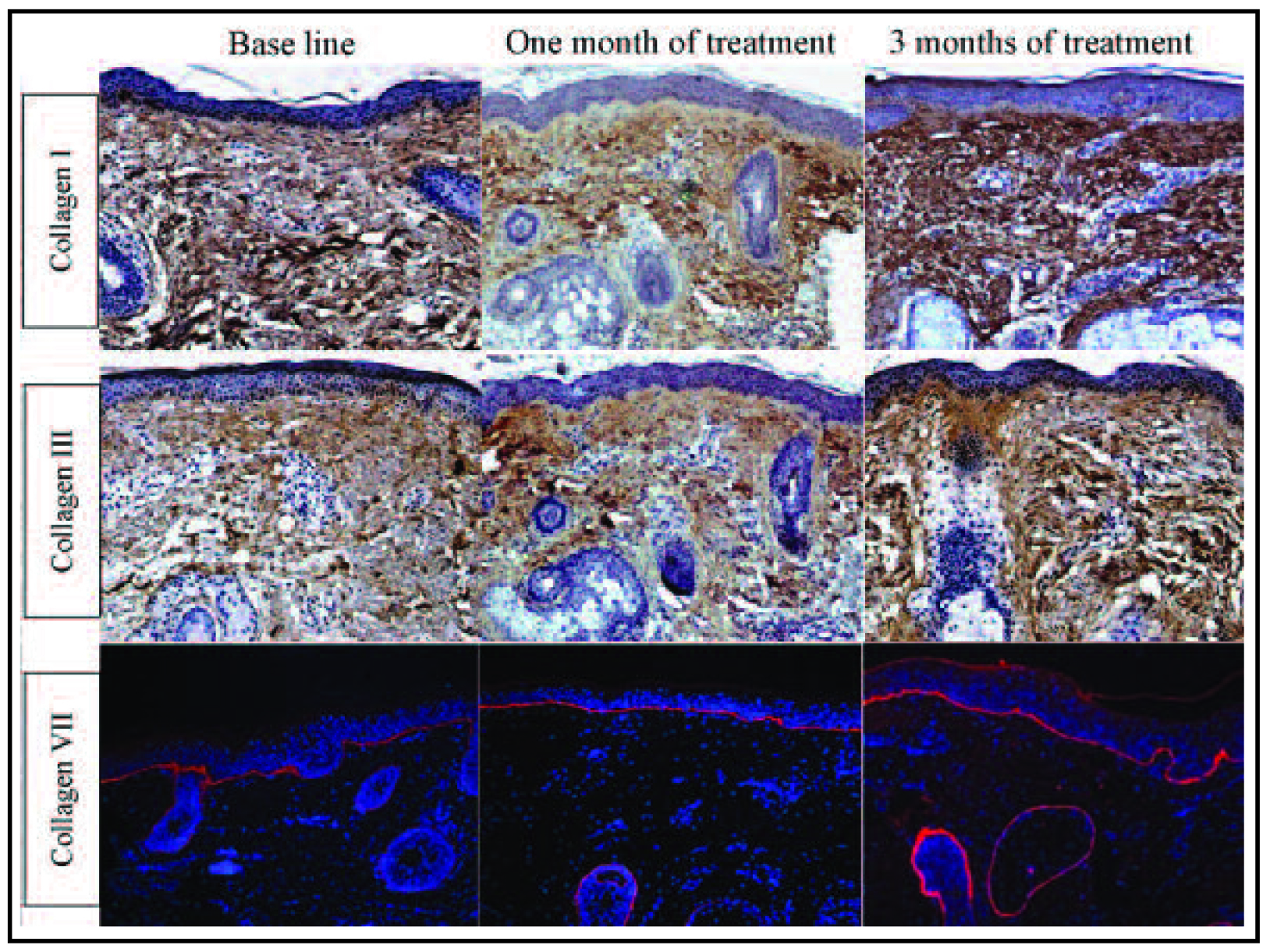
Figure 3. Increase in the level of collagen in response to skin microneedling therapy for post-acne atrophic scars. Immunohistochemical staining of skin tissues at baseline, one month after treatment and three months after starting microneedling treatment for collagen type I, type III and type VII, compared to the baseline)10.
The conclusion drawn from the study suggested that multiple minimally invasive sessions of skin microneedling were effective for post-acne atrophic scars as they stimulated the repair process and were relatively risk-free with minimal patient recovery time10. The findings coincided with those reported in a prospective single-centred study by Pham et al., (2019), who evaluated the effectiveness and safety of microneedling therapy in atrophic acne patients in Vietnam. Similarly, the study found that skin microneedling was effective and a safe treatment for atrophic acne scars1. In conclusion, microneedling offers a safe yet effective treatment option for patients with atrophic acne scars without causing significant damage to their wallet.
References
1. Minh PPT et al. Open Access Maced J Med Sci 2019; 7(2): 293-7. 2. Alanazi MS et al. Electron Physician 2018; 10(8):7224-9. 3. Wang Y et al. Front Med (Lausanne) 2022; 9:939584. 4. Sutaria AH et al. StatPearls. Treasure Island (FL): StatPearls Publishing 2023. 5. Layton AM et al. The Lancet Child & Adolescent Health 2023; 7(2): 136-44. 6. Connolly D et al. J Clin Aesthet Dermatol 2017; 10(9): 12-23. 7. Rajput CD et al. J Cutan Aesthet Surg 2021; 14(2): 177-83. 8. Havelin A et al. Clin Exp Dermatol 2023; 48(5): 443-7. 9. Tirmizi SS et al. Cureus 2021; 13(1): e12578. 10. El-Domyati M et al. J Clin Aesthet Dermatol 2015; 8(7): 36-42.





