

Doctor at the National Health Services (NHS), United Kingdom (UK)

Doctor at Mater Dei, Malta
EEpilepsy is one of the most common neurological conditions, with a prevalence of 0.5% to 1%1. It is considered a chronic brain disorder that affects people of all ages without geographical, social, or racial boundaries. Epileptic seizure is defined as a “transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain2.” This chronic neurological condition substantially burdens the health systems, individuals, and their families. The International League Against Epilepsy (ILAE) has provided a classification system at three different levels: the seizure type (classified into focal onset, generalised onset or unknown onset), epilepsy type (classified as generalised, focal or combined generalised and focal epilepsy or unknown), and epilepsy syndrome2. Notably, antiseizure medications remain the mainstay for the management of epilepsy. Some patients with seizures do not successfully respond to the antiepileptic drug (AED) therapy and are considered to have drug-resistant epilepsy (DRE). To understand more about DRE, we have invited Dr. Daniel Debattista, one of the clinicians at Mater Dei Hospital in Malta, to discuss further on the challenges faced by both patients and clinicians when treating DRE.
So, what is DRE and how does it occur? Dr. Debattista explains that patients are considered to have DRE when monotherapies or combined treatment have been trialled, with no significant benefit reported in patients with epilepsy. He added that some epileptic patients have multiple seizures per day, and with treatment, seizures are reduced to once per day. Contrary to this, some individuals have one seizure per month, reduced to years with appropriate treatment. However, even though antiepileptic drugs (AED) reduce the seizure frequency, they do not fully eliminate the seizure activity in these individuals.
Moreover, the severity of seizures is not usually considered in the definition of DRE. Therefore, these patients are at risk of misdiagnosis and often mismanaged1. Unfortunately, due to the heterogeneity among DRE patients, performing comparative trials or setting up practical guidelines remains challenging; hence, the precise definition of what constitutes DRE remains elusive1.
The prevalence of DRE is around 30%, and incidences vary from 15% in children to 34% in adults3. Recent studies have pointed out that patients with epilepsy related to genetic aetiology and drug resistance are vulnerable to DRE, especially those with severe developmental and epileptic encephalopathies3. Therefore, the personal burden of drug resistance in epilepsy is reflected in its economic impact on healthcare systems and beyond. The financial burden related to DRE is due to the loss of productivity and employment, in addition to the drug resistance which costs the health services approximately 15.5 billion euros per annnum4. Patients with DRE experience decreased quality of life (QoL) with significant medical, social burden and mortality5.
So, what can be done regarding DRE, and how should clinicians approach these kinds of patients? Dr. Debattista explained that the most important thing is to identify patients who are not responding to treatment and show an increased frequency of seizure activities despite being on AEDs. In addition, he also advocated the use of the ILAE criteria for DRE to determine whether a previously used antiseizure medication was tolerated, appropriately chosen, and used6.
The misconceptions regarding the nature of epilepsy and the physical manifestations of seizures are often poorly understood, with negative attributions being common7. In fact, the lack of public understanding regarding the aetiology of epilepsy creates a negative view, which often affects the lives of epileptic sufferers, according to Dr. Debattista. He added that some perceive epilepsy being a mere result of supernatural forces or consider it as a demonic possession, thereby creating fear of affected individuals by others in the society. These perceptions have also been well documented in the literature since such perceptions often shift the blame toward the affected individuals, thereby, potentiating the negative attitude towards the condition7.
Patients with epilepsy may feel rejected from the community and experience public humiliation or even being ridiculed due to a lack of public awareness regarding epilepsy. In extreme circumstances, some may perceive epilepsy as a mental health illness or a result of drug infliction, particularly during an epileptic fit7. Notably, such behaviours are not limited to the general public, instead it has also been reported among some healthcare professionals. Literature based on patient perception and experience has reported some clinicians being less empathic towards the epileptic patients8. But how prevalent is this problem?
In the United States and Europe, the medical or neurological explanation regarding epilepsy is prevalent, therefore, the general public readily accepts the condition. Contrary to this, in areas where the public knowledge of epilepsy remains low, discriminatory behaviour becomes a social norm, thereby promoting the negative impression of the illness9. In addition, “shame” was one of the prominent stigmas described by the epileptic patients since the negative association with epilepsy and the fear of the diagnosis being known to others may create a negative self-perception7.
In a Japanese study that evaluated the treatment of self-stigma in patients with epilepsy, 20 epileptic patients from a psychiatric outpatient clinics were interviewed10. The study revealed that the patients and their families were often aware of the stigma associated with epilepsy, but many did not know how to address the issues10. On this note, Dr. Debattista reminded us that epilepsy is often debilitating, especially for those with DRE. Furthermore, he highlighted how epilepsy can affect an individual’s daily life, particularly in younger patients who often feel their success in education and employment may be limited by their condition7. Then how do we manage such stigma? Dr. Debattista advocated that ongoing education on epilepsy for both patients and their relatives being the first step since this reduces the fear, and negative beliefs regarding epilepsy. Moreover, epileptic patients should be offered counselling services, which may help them develop a better coping strategy.
Several experimental findings from animal models and brain tissues from patients with DRE has helped researchers to propose different hypotheses regarding the underlying mechanisms of DRE (Figure 1)11. However, no treatment has so far shown to to be completely effectively in controlling the symptoms of DRE. The lack of progress could be explained by the fact that there are significant limitations among the proposed hypothesis that attempted to explain the mechanisms of DRE. For instance, the neural network hypothesis proposes that recurrent epileptic seizures cause neuronal death12. It is known that patients with DRE often have cellular alterations such as neural death and the formation of aberrant and excitatory circuits. The remaining neurons undergo remodelling of the neural network which generates hyperexcitable circuits that are challenging to control using endogenous inhibitory mechanisms and AEDs7. So far, no studies were able to replicate these findings among the DRE models. Therefore, it has not been possible to substantiate whether these observations are attributable to drug resistance in patients with DRE13.
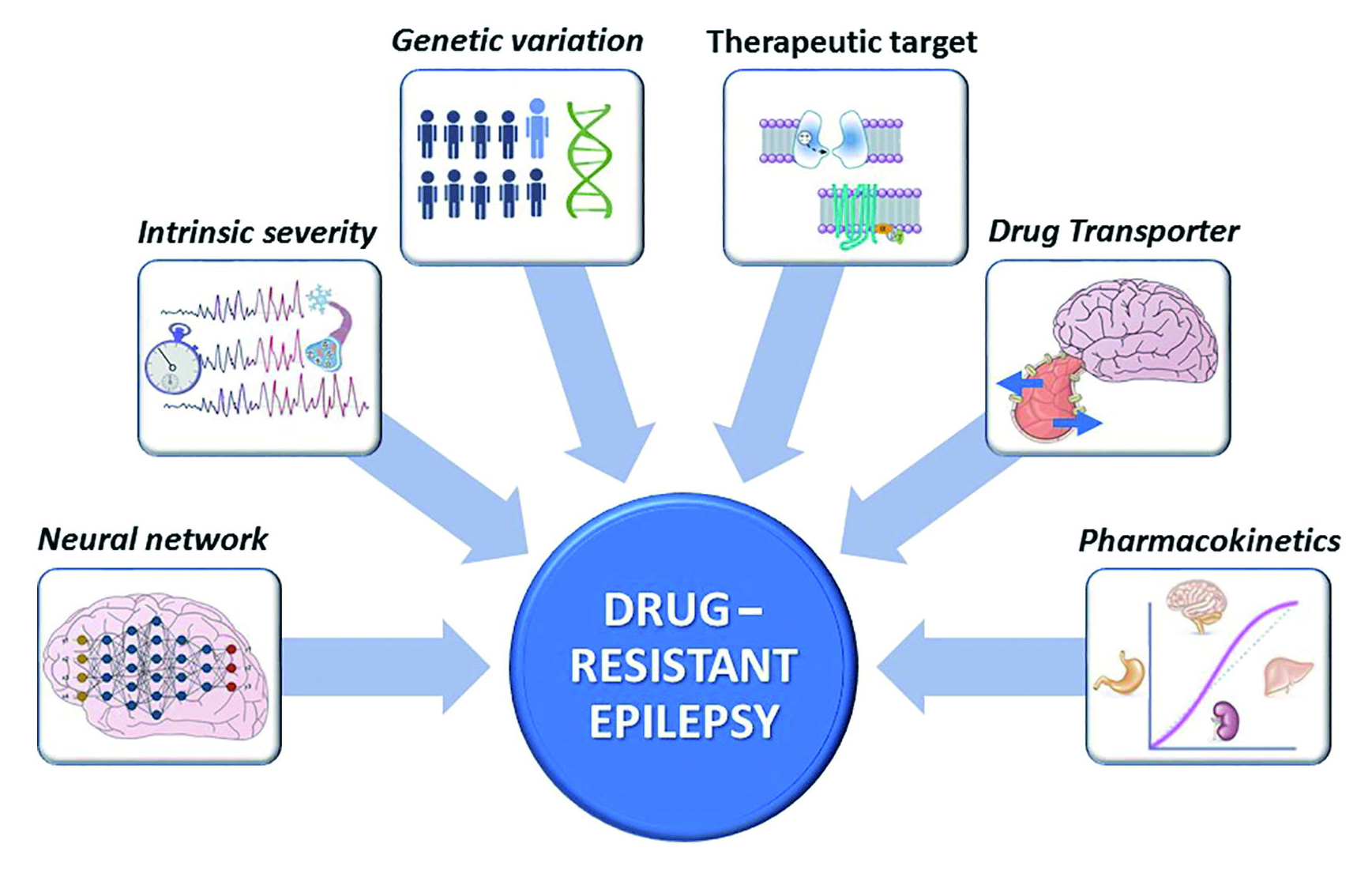
Figure 1. Diagram showing the classical hypotheses of drug resistance in epilepsy11.
Other proposed hypotheses regarding the DRE include the intrinsic severity hypothesis which suggests that drug resistance is an inherent property related to the disease severity14. The predictive factors of DRE include early disease onset, the presence of interictal epileptiform activity, the history of status epilepticus, and comorbidity of neuropsychiatric or neurological disorders. Dr. Debattista explains that this type of model is very difficult to replicate in animal models since animals do not present with spontaneous and recurrent epileptic seizures. He further emphasised that there are high chances of aberrant neuronal circuits with hyperactivity of glutamate, which may induce excitotoxicity, in addition to individuals with DRE overexpressing P-glycoprotein (PGP); together these decrease the efficacy of the antiepileptic treatment13.
Drug resistance in epilepsy is a current scientific dilemma that demands attention. Despite the AEDs, patients with epilepsy often still have seizures and epilepsy surgery, particularly the anterior temporal lobectomy in patients with temporal lobe epilepsy, has shown to be efficacious in randomised controlled trials. In fact, it has been reported to be superior compared to the medical therapy with better therapeutic outcomes in some patients15. Dr. Debattista highlighted that epileptic surgery is often underutilised16, as he explains that the epidemiologic data has shown that there are currently around 1 million patients with DRE in the United States alone, with the majority of them suffering from focal onset epilepsy and considered as potential candidates for epilepsy surgery. However, less than 1% are referred appropriately, with only around 2,000 to 3,000 eventually undergoing the surgery17.
To be considered for epilepsy surgery, patients should first meet the criteria for DRE, which specifies that an epileptic patient with failure of two AEDs, either as monotherapy or combination therapy17. However, it should be emphasised that the AEDs must have been tried adequately prior to diagnosing a patient of having DRE17.
On this note, Dr. Debattista clarified that the adequate trial includes choosing an appropriate AED for a type of seizure being treated and titrating up the dose to the maximum tolerated dose. In addition, AEDs that trigger allergic reactions or cause significant adverse events that requires switching to another AED are not considered as treatment failure17. On the other hand, seizure-freedom is a term used when assessing the success or failure of an AED. The precise definition is “sustained freedom for a period 3 times the longest inter-seizure interval or 1 year, whichever is longer18.” Regarding epilepsy surgery, the primary goal is to reduce seizure activity and avoid adverse reactions after surgery, in addition to improving patients’ quality of life. Currently, epilepsy surgery consists of either resection surgery, palliative surgery, or neurostimulation19. To understand the effects of surgical resection in patients with DRE, Hsieh et al. in 2022 performed a retrospective database-driven cohort study which included 251 patients who were followed up for > 9 years at a single high-volume epilepsy centre. Among the 251 patients, 234 (93.2%) achieved a 6 months and 232 (92.4%) experienced a 1 year of seizure freedom. Furthermore, the average period of seizure freedom was up to 10.3 years, and for patients who were not completely seizure-free, the mean seizure frequency reduction at each time point was 76.2%20. Hence, the study concluded that patients who continued to have seizures after the resection often had a considerable reduction in seizure frequency, and many were able to achieve seizure freedom in a delayed manner20. In conclusion, surgical resection offers not only the greatest opportunity for seizure freedom, but also improves the QoL. Nonetheless, like any treatment, the risk of postoperative complications remains. Therefore, treatment options should be carefully discussed with patients and their decision should be supported to optimise the patient-doctor relationship.
References:
1. Dalic L, Cook MJ. Managing drug-resistant epilepsy: challenges and solutions. Neuropsychiatr Dis Treat 2016; 12: 2605-16. 2. Asadi-Pooya AA, Brigo F, Lattanzi S, Blumcke I. Adult epilepsy. The Lancet 2023; 402(10399): 412-24. 3. Guery D, Rheims S. Clinical Management of Drug Resistant Epilepsy: A Review on Current Strategies. Neuropsychiatr Dis Treat 2021; 17: 2229-42. 4. Löscher W, Potschka H, Sisodiya SM, Vezzani A. Drug Resistance in Epilepsy: Clinical Impact, Potential Mechanisms, and New Innovative Treatment Options. Pharmacol Rev 2020; 72(3): 606-38. 5. Denton A, Thorpe L, Carter A, Angarita-Fonseca A, Waterhouse K, Hernandez Ronquillo L. Definitions and Risk Factors for Drug-Resistant Epilepsy in an Adult Cohort. Front Neurol 2021; 12: 777888. 6. Perucca E, Perucca P, White HS, Wirrell EC. Drug resistance in epilepsy. The Lancet Neurology 2023; 22(8): 723-34. 7. Mayor R, Gunn S, Reuber M, Simpson J. Experiences of stigma in people with epilepsy: A meta-synthesis of qualitative evidence. Seizure 2022; 94: 142-60. 8. Sarudiansky M, Korman GP, Scévola L, Oddo S, Kochen S, D'Alessio L. A life with seizures: Argentine patients' perspectives about the impact of drug-resistant epilepsy on their lives. Seizure 2018; 63: 52-61. 9. Al-Dossari KK, Al-Ghamdi S, Al-Zahrani J, et al. Public knowledge awareness and attitudes toward epilepsy in Al-Kharj Governorate Saudi Arabia. J Family Med Prim Care 2018; 7(1): 184-90. 10. Kuramochi I, Horikawa N, Shimotsu S, et al. The self-stigma of patients with epilepsy in Japan: A qualitative approach. Epilepsy Behav 2020; 109: 106994. 11. Pérez-Pérez D, Frías-Soria CL, Rocha L. Drug-resistant epilepsy: From multiple hypotheses to an integral explanation using preclinical resources. Epilepsy Behav 2021; 121(Pt B): 106430. 12. Kapur J. Role of Neuronal Loss in the Pathogenesis of Recurrent Spontaneous Seizures. Epilepsy Curr 2003; 3(5): 166-7. 13. Pérez-Pérez D, Frías-Soria CL, Rocha L. Drug-resistant epilepsy: From multiple hypotheses to an integral explanation using preclinical resources. Epilepsy & Behavior 2021; 121: 106430. 14. Santana-Gomez CE, Engel J, Jr., Staba R. Drug-resistant epilepsy and the hypothesis of intrinsic severity: What about the high-frequency oscillations? Epilepsia Open 2022; 7 Suppl 1(Suppl 1): S59-s67. 15. Wiebe S, Blume WT, Girvin JP, Eliasziw M. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 2001; 345(5): 311-8. 16. Medina-Pizarro M, Spencer DD, Damisah EC. Recent advances in epilepsy surgery. Current Opinion in Neurology 2023; 36(2). 17. Anyanwu C, Motamedi GK. Diagnosis and Surgical Treatment of Drug-Resistant Epilepsy. Brain Sci 2018; 8(4). 18. Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010; 51(6): 1069-77. 19. Sheng J, Liu S, Qin H, Li B, Zhang X. Drug-Resistant Epilepsy and Surgery. Curr Neuropharmacol 2018; 16(1): 17-28. 20. Hsieh JK, Pucci FG, Sundar SJ, et al. Beyond seizure freedom: Dissecting long-term seizure control after surgical resection for drug-resistant epilepsy. Epilepsia 2023; 64(1): 103-13.





