
Chronic kidney disease (CKD) is an increasing public health concern with an estimated global prevalence of 10.6% for stages 3-5 and 13.4% for stages 1-5. In 2016, there were 275.9 million cases of CKD with around 1.2 million deaths and 35 million years of healthy life lost attributed to CKD1. During the peak of coronavirus disease-2019 (COVID-19) pandemic, many renal services were severely disrupted by the lockdown policy which hindered patient access to the kidney diagnostic, and treatments modalities. Together, these disruptions had detrimental effects on patients' kidney health, and their overall wellbeing. Apart from the COVID-19 pandemic, other unexpected events such as natural disasters and political unrest also imposed significant strain on the healthcare system and patients with CKD2. To address the importance of preparing for unexpected events and to highlight the strategies for supporting patients with CKD, the theme of this year's World Kidney Day (WKD) primarily focused on “Preparing for the unexpected, supporting the vulnerable3.”
Che unforeseen threat imposed by infectious diseases on healthcare services was substantial during the COVID-19 pandemic. A systematic review performed by Moynihan et al, (2021) included 3,097 references with 81 studies across 20 countries reporting the impact of COVID-19 pandemic on utilisation of healthcare services. They reported a median reduction of 37% in overall healthcare services utilisation caused by the COVID-19 pandemic, mainly a decrease in patient visits, admissions, diagnosis and therapeutics prescription (Figure 1)4. In Hong Kong, a cross-sectional survey by Hung et al. (2022) assessing the impact of COVID-19 on the health services during COVID-19 locally indicated that 30.4% of respondents avoided the medical consultation due to COVID-195. Not surprisingly, the concern of being infected was the primary reason why individuals avoided healthcare services6, with lockdowns and stay-at-home policies being among the causes for hinderance in utilisation of healthcare services during the pandemic.
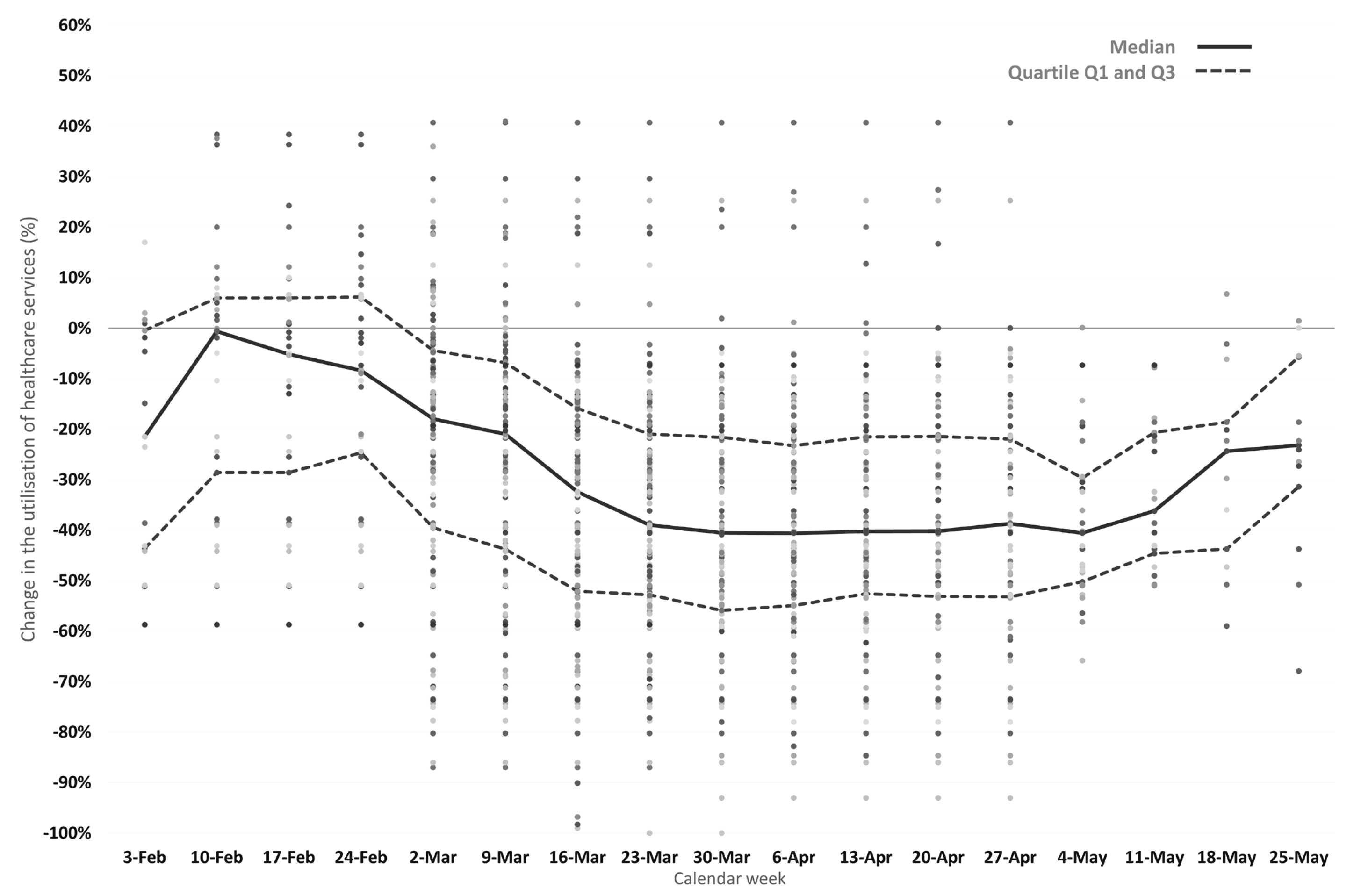
Figure 1. COVID-19-related changes in healthcare utilisation4
Pandemic asides, the access to healthcare services is often related to what the patient can afford, also known as patient affordability. Therefore, healthcare affordability looks at the cost of healthcare services related to patients’ income and capacity to pay. It is dependent on the ratio between the healthcare expenditure and non-healthcare expenditure with a consideration for budget constraints and other sourced elements of coverage7. Therefore, economic crisis can have significant impact on healthcare assess, for instance, unemployment substantially put financial strain on individuals by limiting their affordability. Contrary to this, the unexpected change in the country’s economy have detrimental effects on the healthcare affordability. For instance, Kyriopoulos et al. (2019) highlighted the case of unprecedented sovereign debt crisis seen in Greece in 2009 in which patients were not able to afford the basic healthcare needs8.
The disruption of healthcare utilisation during the natural disasters or extreme weather has also been extensively documented. Notably, Clarke et al. (2015) reported that extreme weather often has negative effects on individual’s health, particularly the elderly who are unable to leave their homes or drive to seek assistance, particularly in extreme weather. Therefore, they are often socially isolated, which hinders them from accessing healthcare services9. To highlight the effects of unexpected events, Lempert et al. (2013) highlighted how hurricane Sandy in 2012 disrupted the dialysis services, which resulted in worsening of kidney diseases with a higher incidences of acute kidney injury (AKI) reported10.
During the unexpected events, patients with kidney disease are considered among the most vulnerable due to the complexity of their disease which requires regular specialist centre care. During the COVID-19 pandemic, access to the renal dialysis units or immunosuppressive therapies were often limited, thereby, predisposing these individuals to severe complications, including death11. A meta-analysis performed by Deng et al. (2022) included 23 studies highlighted the effects of COVID-19 pandemic on the renal services with a reduction in access to kidney transplantation (risk ratio [RR]: 2.15, p < 0.001), dialysis, and in-person nephrology care compared to pre-COVID-19 era. This further demonstrated the fact that COVID-19 was a significant barrier to accessing care in a highly vulnerable chronic disease group12. Nonetheless, these scenarios only depict part of the problem related to the unexpected events and how they disrupt healthcare services. Therefore, to minimise these disruptions, stakeholders from various health sectors should cooperate and formulate strategic plans to minimised disruption of healthcare services during the unexpected events. In addition, they should also ensure that there are contingency plans put in place to ensure patients such as CKD patients can access the healthcare services without any barriers.
Unexpected events are unpredictable, with disruption to kidney care becoming much more prevalent and likely to increase in near future. In fact, studies have shown COVID-19 pandemic have accelerated kidney pathology and worsened the outcomes of nephrology patients with more patients requiring emergency dialysis13. Therefore, a considerable level of preparation should be put in place to account for these unexpected events to ensure that people, regardless of their CKD status, should receive appropriate, immediate, and continuous healthcare during and after an unexpected incidence. In this regard, the theme for the World Kidney Day 2023 was coined as “Preparing for the unexpected, Supporting the vulnerable!”3
In accordance with the theme, local and international kidney organisations advocated for policymakers to adopt integrated health strategies that prioritise prevention, early detection, and management of non-communicable diseases (NCDs), including kidney disease, and urged the governments to include emergency preparedness plans for the management and detection of NCDs. They also encouraged the healthcare services to provide equitable and adequate access for patients with NCDs during global crisis. Moreover, patients are recommended to plan for emergencies by preparing emergency kits that consists of food, water, medical supplies, and medical records11.
When considering the roles of policymakers and governments, the priority is to implement an appropriate policy framework that tailors the needs of patients with kidney disease before, during, and after an emergency. Furthermore, investment into a resilient primary and public healthcare systems may help us withstand from unfavourable conditons14.
Moreover, healthcare service providers are key players responsible for the delivery of healthcare services, even during adverse events. Therefore, they should be well-prepared to scale up health service in order to meet the unexpected rising demand by providing adequate staff training and educating patients and caregivers on ways to deal with emergency situations. Apart from strengthening operation, utilising innovative technologies, such as telemedicine has also shown to be effective. Therefore, healthcare service providers should also promote public awareness and ways to prepare for emergency in vulnerable communities14.
On the other hand, the participation of patients with kidney disease is crucial for preparing in case of emergency. Apart from preparing the emergency kit, the patients should also formulate a list of important contacts, such as contacts of back-up dialysis units, and the list of their medical needs. Of importance, they should be familiar with emergency evacuation procedures and equipped with relevant knowledge; for instance, they should be able to safely disconnect themselves from a dialysis machine during an emergency14.
While unexpected emergencies are unpredictable and remains uncontrollable, implementing a well-designed preparatory framework helps to reduce the risk to local economic, socio-political, and environmental aspects, thereby, would enhance the capacity of vulnerable population to cope with the unexpected events. Above all, when a significant event has occurred, it is most important to adopt the 4 “Cs” approach for disaster response – Command, Control, Coordinate and Communicate.
References
1. Department of Health. Non-Communicable Diseases Watch February 2020 - Be Aware of Chronic Kidney Disease. 2020. 2. Karam et al. Kidney Int Rep 2023; 8: 383–7. 3. Hsiao et al. Kidney Int 2023; 103: 436–43. 4. Moynihan et al. BMJ Open 2021; 11: e045343. 5. Hung et al. Int J Health Policy Manag 2022; 11: 508–13. 6. Lazzerini et al. Lancet Child Adolesc Health 2020; 4: e10. 7. Zavras. Int J Environ Res Public Health 2020; 17: 1–21. 8. Kyriopoulos et al. Soc Sci Med 2019; 222: 274–84. 9. Clarke et al. Am J Public Health 2015; 105: 1489. 10. Lempert et al. Am J Kidney Dis 2013; 61: 865. 11. Daga et al. Pediatr Nephrol 2023; 1: 1. 12. Deng et al. Nephrology (Carlton) 2022; 27: 410–20. 13. Mureșan et al. J Clin Med 2022; 11. DOI:10.3390/JCM11092452. 14. World Kidney Day Campaign. WKD 2023 Position Paper – Resilience in kidney care for all. A call to action. 2023.





