

Specialist in Endocrinology
Diabetes & Metabolism
Preventing Cardiovascular Complications
by Lowering LDL-C in Type 2 Diabetes Mellitus
Diabetes mellitus (DM) is one of the leading causes of death in Hong Kong accounting for 0.9% of all registered deaths in 2017, whereas the crude death rates for male and female were 5.5 and 5.4 per 100,000 population of respective sex1. In particular, type 2 diabetes mellitus (T2DM) is the most frequent type of DM affecting about 700,000 people in Hong Kong2 and is a leading cause of morbidity and mortality due to diabetic complications3. Of note, T2DM patients are at high risks for both micro- and macrovascular complications whereas optimal control of cardiovascular (CV) risk factors can significantly decrease the risk of DM-related complications. As hyperlipidaemia is one of the most important modifiable risk factors for CV disease among DM patients, Dr. Francis CC Chow shared his insights and clinical experience in preventing CV complications by controlling low-density lipoprotein cholesterol (LDL-C) level in patients with T2DM.
The Complexities of DM and its Health Burden
Diabetes mellitus (DM) is associated with the increased risk of cardiovasular (CV) complications whereas each 1% reduction in mean glycated haemoglobin (A1c) would result in reduction of microvascular complications, myocardial infarction and DM-related mortality by 37%, 14% and 21% respectively4. “The risks of micro- and macrovascular complications are higher by 2-10 times in DM patients as compared to non-DM, especially in cases involving multiple risk factors,” Dr. Chow commented. He further highlighted that, among various types of DM, patients with type 2 DM (T2DM) complicated with central obesity, fatty liver and dyslipidaemia are very common clinically. These patients are generally younger, usually aged 30 to 50, while male patients are more common. Essentially, they have high risks for hypertension and dyslipidaemia.
Dr. Chow addressed that DM is associated with a wide spectrum of pathologic conditions including cerebrovascular accident (CVA), renal failure, obesity, depression, etc. (Figure 1). Hence, he emphasised that controlling lipid level is only one part of the total risk management for CV complications in patients with T2DM.
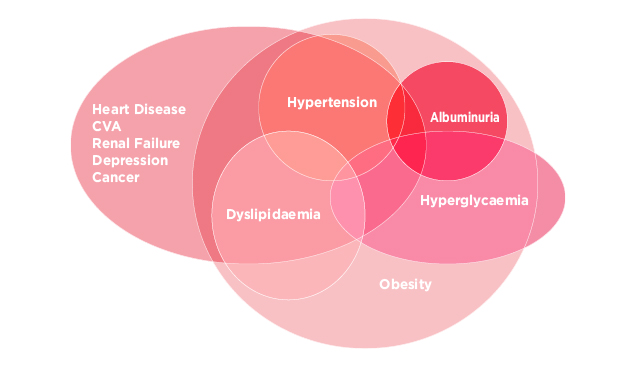
Figure 1. The complexities of diabetes (illustrated by Dr. Chow)
Diabetic Dyslipidemia
Dr. Chow noted that 70-80% of bad cholesterol, low-density lipoprotein cholesterol (LDL-C), is made in the body, but not from diet. Insulin resistance and obesity increase the release of free fatty acids (FFA) from adipose tissue. The FFA are resynthesised into triglycerides (TG) in the liver and then secreted into plasma as very low density lipoproteins (VLDL). The increased amount of VLDL competes with TG-rich chylomicrons and their lipolytic remnants for the limited lipolytic capacity provided mainly by lipoprotein lipase leading to hypertriglyceridaemia5.
Besides, partly due to the action of cholesteryl ester transfer protein (CETP), TG-enrichment of both LDL and high density lipoprotein (HDL) particles occurs. The sizes of the LDL particles are subsequently reduced by hepatic lipase. The small, dense LDL delays their normal clearance from plasma whereas the small HDL particles are more readily catabolised by the kidneys and thus impairing the antiatherogenic functions of HDL (Figure 2)6. Dr. Chow added that genetic factor plays a significant role in the production of extra cholesterol.
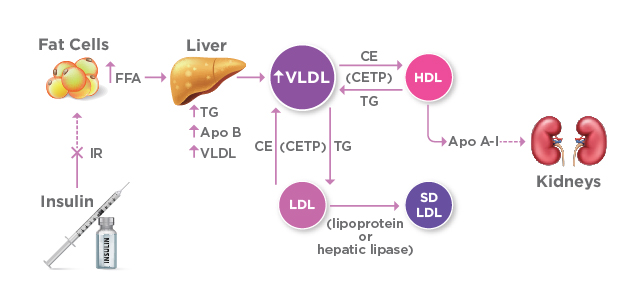
Figure 2. Mechanism of DM dyslipidemia (CE: cholesteryl ester; IR: insulin resistance)
Never Too Low for LDL-C
In preventing CV complications in DM, Dr. Chow commented that LDL-C has to be the foremost to be controlled. Yet, it is specific for each individual on whether his/her LDL-C level is ideal or not. “The ideal level of LDL-C is variable based on one’s background. Nonetheless, there is no lower limit of unsafe,” he emphasised.
Dr. Chow’s comments comply with the statements in latest guidelines. According to the EAS/ESC Guidelines 2019, LDL-C levels should be lowered as much as possible to prevent CV diseases, especially in high and very high risk patients. Of note, patients with DM are already classified as high-risk for CV complications7. The Guidelines reported that lowering LDL-C beyond the goals set in former EAS/ESC Guidelines is associated with fewer atherosclerotic CV diseases (ASCVD). Essentially, there is no level of LDL-C below which benefit ceases or harm occurs has been defined. “Patients with multiple risk factors such as obesity and longer disease duration are at very high-risk while more stringent treatment goal of LDL-C <1.4 mmol/L is adopted,” Dr. Chow highlighted.
Prevention before Disease Development
Currently, there are several classes of LDL-C lowering medications with established CV benefits, including statins, ezetimibe and PCSK9 inhibitors, whereas statin treatment is recommended for primary prevention according to the risk level. For high-risk patients, potent statins such as rosuvastatin and atorvastatin are recommended in order to achieve the stringent treatment goal. However, Dr. Chow said it was still controversial whether higher dose of potent statin is needed, especially for Chinese patients. He suggested that, based on clinical observations, Asians are more sensitive to statins and thus some of his patients on rosuvastatin 5 mg yielded LDL-C reduction by 60-70%. He further shared that, for follow-up treatment, either up-titrating statin or statin with lipid absorption inhibitor can be considered, whereas the latter treatment is his preferred choice. For patients not responding or intolerant to the treatment, PCSK9 inhibitor would be prescribed. Importantly, Dr. Chow suggested informing the patients on potential side effects routinely and sharing the treatment protocol with them.
As there are multiple risk factors for T2DM, a wide scope of actions are needed in preventing CV complications. Hence, Dr. Chow featured the ABCDES3 of routine DM visits addressed by the Guidelines of Diabetes Canada, which provides recommendations on diagnosis, medications used, lifestyle factors and screening tests (Figure 3)8.
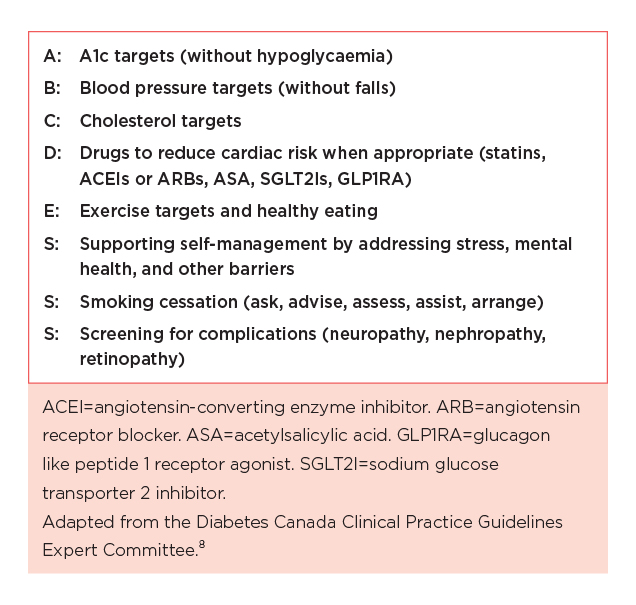
Figure 3. The ABCDES3 of routine diabetes visits8
Dr. Chow emphasised that patients with T2DM need aggressive treatment to control CV risk. “There are about 50-80% of DM patients with suboptimal control on LDL-C level whereas only 20-30% of them are on statins,” he stated. Man et al (2016) reported that the prevalence of therapeutic inertia in lipid management among T2DM patients was common in the primary care setting in Hong Kong3. Thus, adequate family medicine training among physicians is crucial for overcoming therapeutic inertia and hence improving treatment outcomes in chronic disease management.
Based on the proven benefits of LDL-C reduction among T2DM patients and the established clinical efficacies of LDL-C lowering therapies, latest guidelines advocate aggressive treatments for controlling LDL-C level in DM patients in order to prevent CV complications. The clinical experience shared by Dr. Chow demonstrated that treatment with potent statins effectively reduces LDL-C and in turn improving overall health outcomes for T2DM patients. Further enhancement on the awareness of LDL-C control among frontline physicians will certainly help preventing CV complications for T2DM patients before disease onset.
Reference
1. Department of Health. HealthyHK - Public Health Information and Statistics of Hong Kong - Leading Cause of all Deaths. 2. Task Force on Conceptual Model and Preventive Protocols. Hong Kong Reference Framework for Diabetes Care for Adults in Primary Care Settings.; 2018. 3. Man et al. Hong Kong Med J. 2016;22(4):356-364. 4. Stratton et al. BMJ. 2000;321(7258):405-412. 5. Föger. Wien Med Wochenschr. 2011;161(11-12):289-296. 6. Föger et al. J Biol Chem. 1999;274(52):36912-36920. 7. Mach et al. Eur Heart J. August 2019. 8. The Canadian Diabetes Association. Diabetes Canada | Clinical Practice Guidelines - 2018.





