The mineral balance in the body is governed by various organs including kidney, bone, small intestine and parathyroid glands. Particularly, the kidneys receive input through humoral mediators and neural networks, integrate the input, and alter the excretion and absorption of calcium and phosphate in the renal tubules to maintain a mineral balance in the whole body. Thus, once kidney function declines, disruption of the mineral network would gradually develop.
Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) is a systemic disorder characterised by abnormal serum biochemistries, including hyperphosphatemia and hypercalcemia, bone disorders, and vascular calcification (VC). CKD–MBD is highly prevalent in patients with Chronic Kidney Disease (CKD) and increases the risk of morbidity and mortality in these patients, especially those receiving dialysis therapy.
Given the complex pathophysiology of CKD-MBD, the treatment for CKD–MBD involves phosphate unloading, maintenance of calcium balance, control of secondary hyperparathyroidism, maintenance and enhancement of bone strength, and prevention of VC, cardiovascular diseases, and death. Currently, phosphate binders, vitamin D receptor activators (VDRAs), calcimimetics, and medications for osteoporosis are the cornerstones for pharmacological treatment of CKD–MBD.
On 8-Dec 2022, a hybrid lecture titled “Advancing the Care for Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD)” organised by the Hong Kong Society of Nephrology was successfully held. In the lecture, Dr. Shunsuke Yamada of Kyushu University Hospital and Dr. Desmond Yap of the University of Hong Kong shared their insights on the risk of vascular calcification of CKD-MBD and its prevention, and the management of CKD-MBD, respectively. In outlining the treatment options for uremic VC, Dr. Yamada presented the efficacy of calcimimetics in lower serum parathyroid hormone (PTH) levels. He also outlined the vicious cycle formed by anaemia, CKD, and congestive heart failure (CHF) in the cardio-renal-anaemia (CRA) syndrome. Hence, the clinical benefits of darbepoetin in achieving target blood haemoglobin levels, avoiding of red blood cell transfusion, and increasing in vitality were presented. In Dr. Yap’s lecture, the control of phosphate, the use of vitamin D receptor activators (VDRAs), and the use of calcimimetics were discussed. Essentially, Dr. Yap also shared his clinical experience in managing patients with CKD-MBD in local settings.
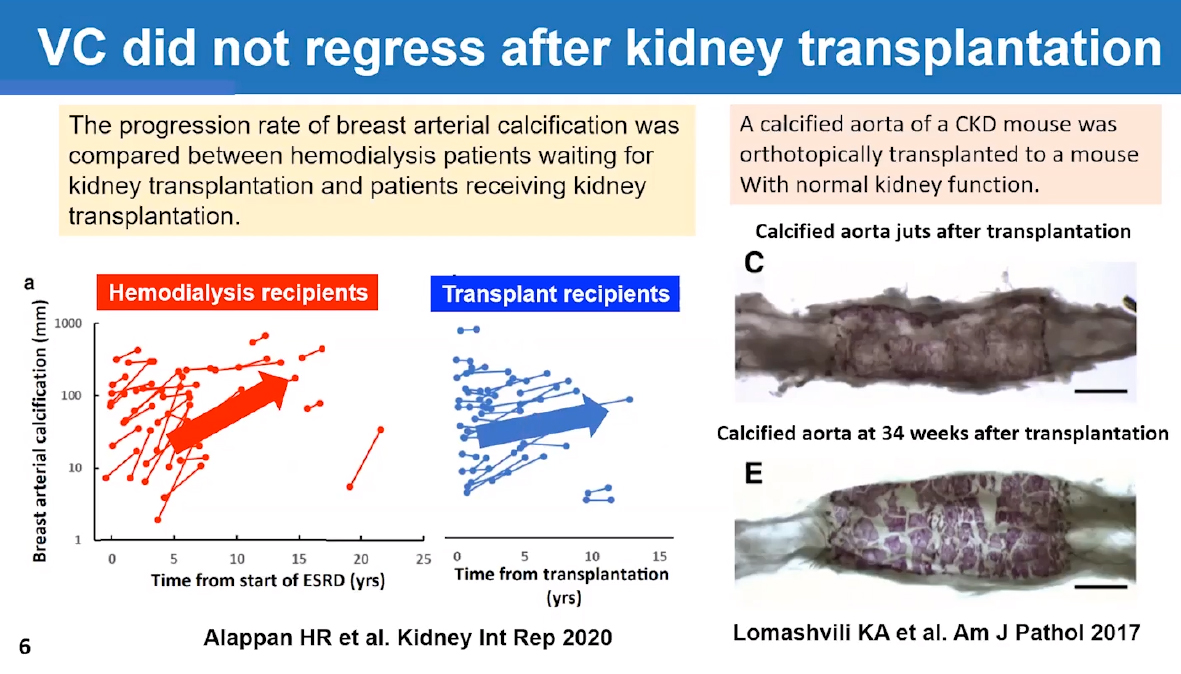
Dr. Yamada outlined the pathophysiology of vascular calcification

The clinical performance of cinacalcet plus low-dose vitamin D was reviewed
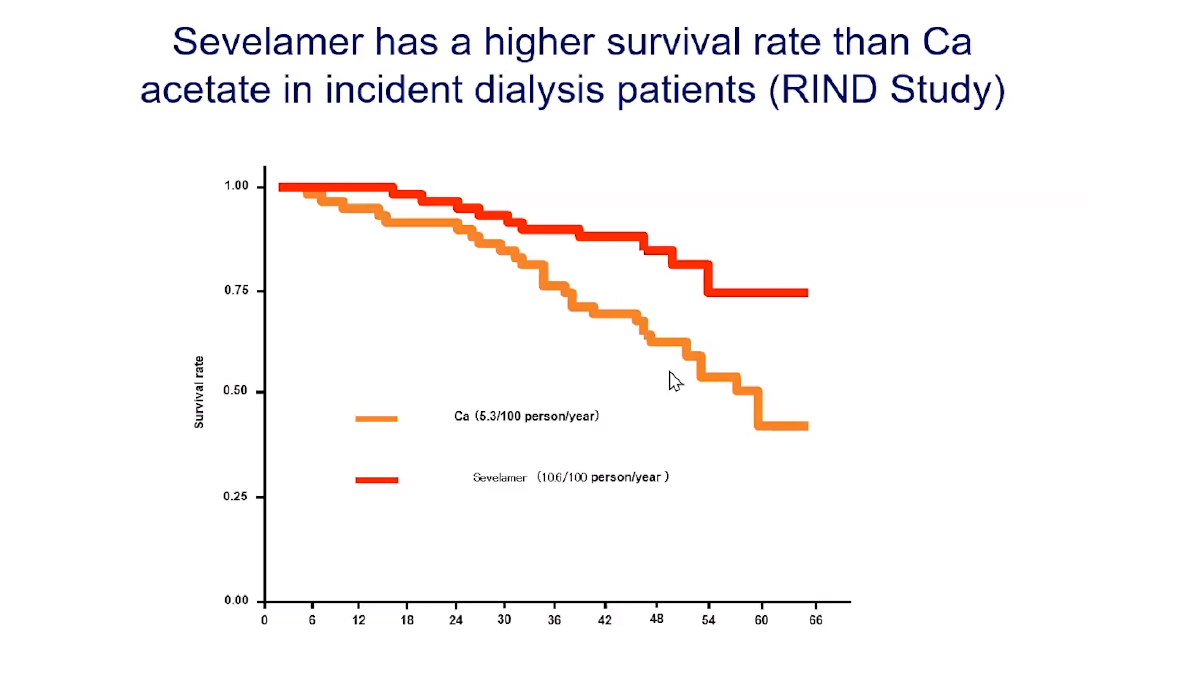
Dr. Yap presented the survival benefit of sevelamer achieved in the RIND Study
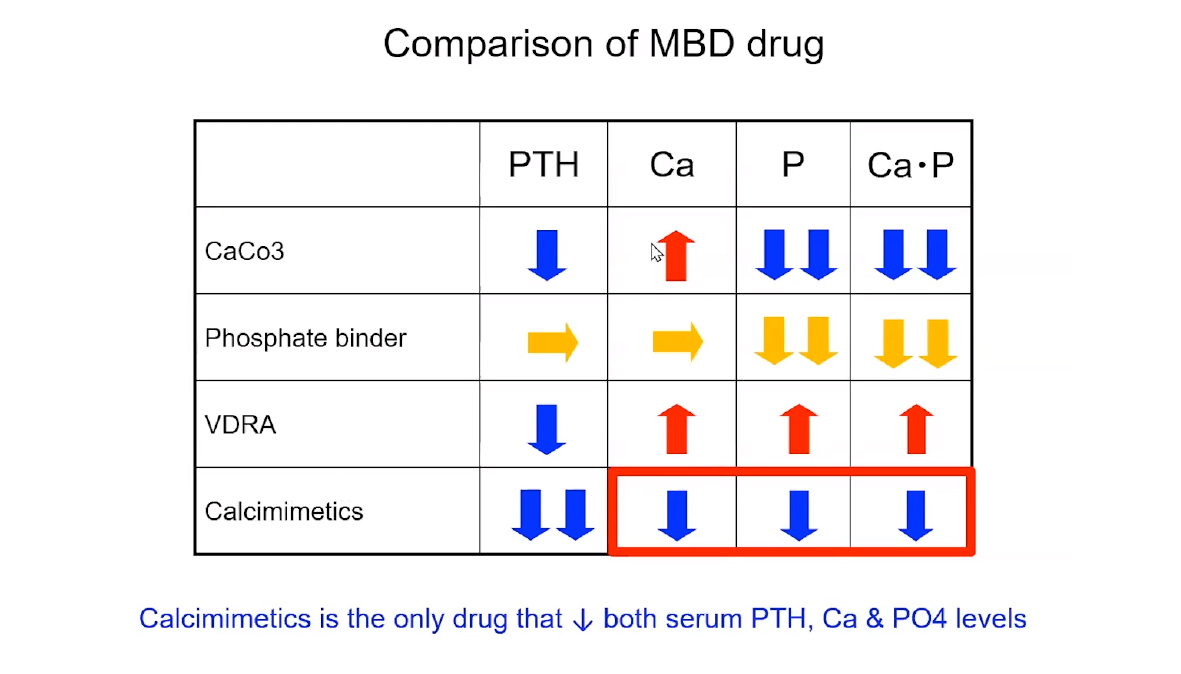
Dr. Yap compared the pharmacology of calcimimetics with other MBD medications





