
Emerging into Adulthood: A Niche for Nutrition Interventions Targeting Dietary Habits in Tertiary Students
The ever-going information boom following technological advancement has been flooding the society with abundant supply of information of all sources, health-related particularly. One must read some publications with “miracle” title like anti-ageing tips and cancer-fighting diet somehow before. Such phenomenon symbolises the perceived concern over disease prevention by the public, which is one step ahead of detection.
You Are What You Ate Yesterday
Life course approach adopts a temporal and social perspective, conceptualising the origin of ill health can be traced throughout life course trajectories. Exposure to physical and social hazards during previous life stages gives rise to corresponding health outcomes later in life1. In simple words, breastfeeding in infancy reduces the risk of developing type 2 diabetes in adulthood2. The pattern of health and disease is sometimes beyond one’s cognition. The transition between adolescent and adulthood is regarded as one of the sensitive developmental stages, characterised by increasing independence, autonomy, and responsibility. It is the first time period when young adults start to taste and exercise their privileges making decisions about their life, apparently including diet3. Whether the changes in dietary habits during this stage persist over time still remain unclear and require further studies. Yet there is evidence suggesting elevated risk of major chronic diseases is associated with weight gain during early and mid-adulthood4. This life stage, signifying the disruption of pre-existing habits and change-enabling nature, unquestionably holds great potential for preventive interventions3,5.
Where We Are Now
The dietary profile of Hong Kong adults is captured as follows with the results of Behavioural Risk Factor Survey 2016. For fruit and vegetable (FV) consumption, the mean days of eating vegetables per week was 6.4 days with 80% responders reported consumption on daily basis; while the mean days of eating fruits per week was 5 days with only half of them consumed every day. The above figures are seemingly amusing, but the consumption is de facto inadequate because merely 1 out of 5 people met the recommendation of 5 or more FV per day6. Among all age groups, young adults aged 18-24 had the highest prevalence of inadequate FV consumption7. For meat, average 4.8 taels of red and white meat were consumed every day, which is slightly below the daily recommendation of 5-8 taels6,8; the good news is over 60% of people reported consuming processed meat 1 day or less per week6.
A 2018 study on Hong Kong local retail food environment gives some additional details to the profile. It measured the Retail Food Environment Index (RFEI), a ratio of reflecting the relative density of unhealthy food outlets (UFOs)* to healthy food outlets (HFOs)†; a higher RFEI indicates an unhealthier food environment. Hong Kong had an average RFEI of 4.61, suggesting the resident exposed to 4.61 times more UFOs than HFOs within 1000 m of their homes which was comparable to those living in urban California. Residents living in an area with the highest RFEI were 40% more likely to have infrequent FV consumption than those of the lowest RFEI. Hong Kong was also found having high density of both healthy and unhealthy food outlets, 10 times more HFOs with only 6 times more UFOs as compared to New York City. The results above specify the problem of Hong Kong should be the abundance of unhealthy foods rather than limited access to healthy foods9.
The World Health Organization recommends the uptake of price policies to promote healthier diets, like taxes on saturated fats and sugary drinks10. However it may not be as adaptable as proposed for Hong Kong case due to the absence of goods and services tax locally plus the import-biased food supply. Vigorous oppositions against it from general public can be expected as well. Therefore, nutrition intervention seems to be a feasible, sustainable option remained to go with in this sense.
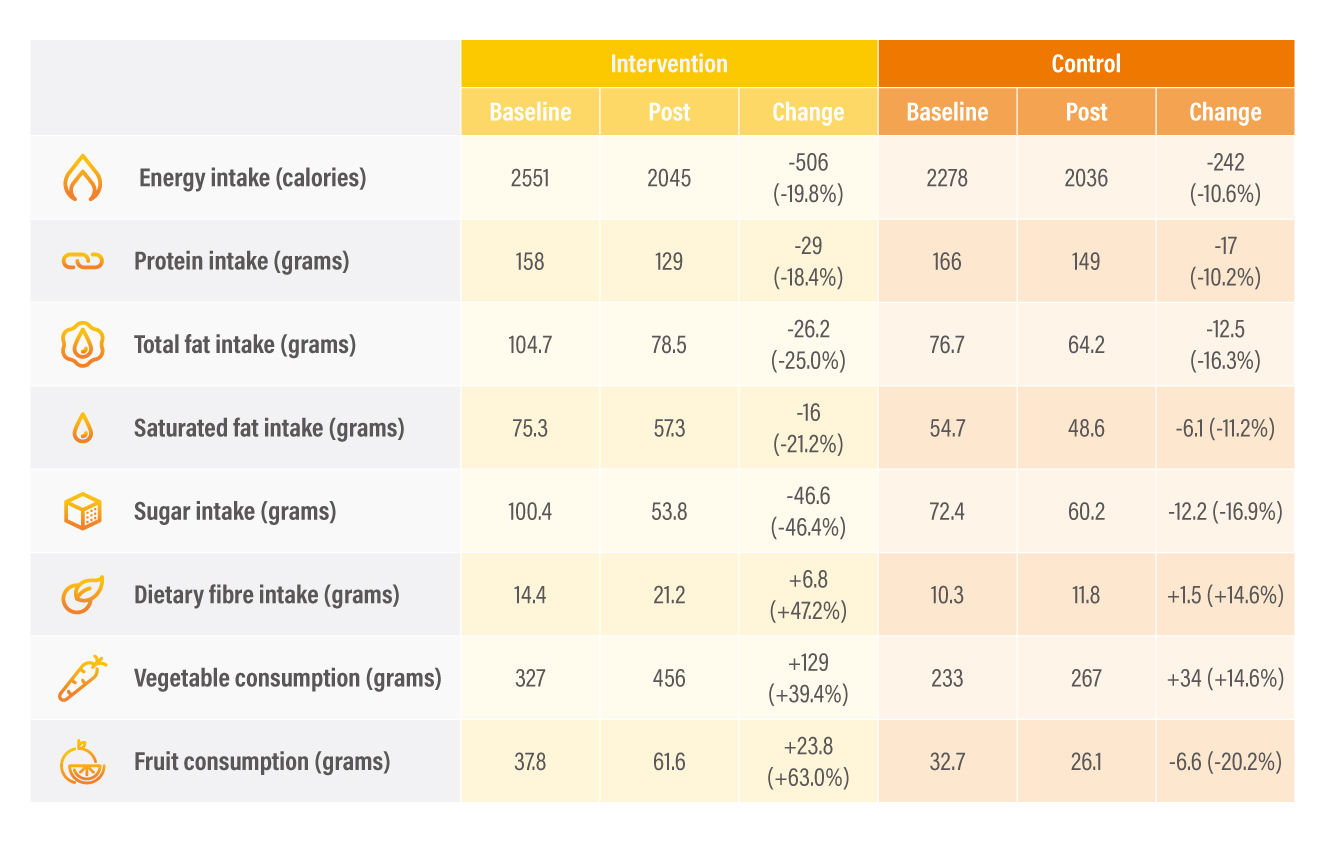
Table 1. Result of selected indicators11
Where we ought to go
Nutrition intervention can be of any method that passes on knowledge and/or skills about healthy eating or alters one’s eating behaviours. A 2021 local study investigated the changes in dietary behaviours in young adults aged 19 - 31 with the utilisation of mobile applications. Both intervention and control groups received a three-hour nutrition seminar. Dietary monitoring with the app was exclusive to the intervention arm. There were significant increase in FV consumption and decease in sugar intake with mobile apps monitoring of 12 weeks (Table 1)11. The results have demonstrated the potential of “nudge” which gently pushes people towards healthy behaviours without restricting choice.
Given the wide spectrum of nutrition intervention, it can also be in form of cooking class delivering cooking skills. However it is disappointing to find out that improvement in cooking skills does not necessarily get translated into healthier dietary habits in oversea university students12,13. Even so, cooking skills are not entirely irrelevant to healthy dietary habits. Contradicting though, self-perceived cooking skills can be a predictor for nutrition-related outcomes of later life. Those described their cooking skills adequate at age 18-23 tended to report usual involvement in meal preparation, greater vegetable consumption, and lower fast food consumption 10 years later14. Reconciling these conflicting ideas, an inference of knowledge and skills are not equally influential can be obtained. Nevertheless both contribute to the readiness for initiating change in dietary habits.
There is no magic bullet for the prevailing incidence of chronic diseases. Instead, it is a “Journey to the West” that requires synergy of public health interventions targeting various components at different levels. Emerging into adulthood does not only represent the potential to strive for a healthier population or society, but also aims to have the general public and policymakers to reflect on how many opportunities out there have been forgone. So, is it too late to start pushing forward preventive healthcare? It is better late than never.
References
1. World Health Organization. The implications for training of embracing A Life Course Approach to Health. Available at http://apps.who.int/iris/bitstream/handle/10665/69400/WHO_NMH_HPS_00.2_eng.pdf;jsessionid=BC8933272D1267715D655303E3DECE4A?sequence=1/. Accessed Jan 25, 2022. 2. Owen CG, et al. The American Journal of Clinical Nutrition 2006; 84(5): 1043-1054. 3. Mueller MP, et al. Nutrients 2018; 10(6): 716. 4. Zheng Y, et al. JAMA 2017; 318(3): 255-269. 5. Winpenny EM, et al. Int J Behav Nutr Phys Act 2018; 15(1): 86. 6. Centre for Health Protection. Department of Health. Behavioural Risk Factor Survey (April 2016). Available at https://www.chp.gov.hk/files/pdf/brfa_report_april_2016_eng.pdf/. Accessed Jan 25, 2022. 7. Centre for Health Protection. Department of Health. Diet, physical activity and health: Hong Kong situation. Available at https://www.change4health.gov.hk/filemanager/common/image/strategic_framework/action_plan/action_plan_2_e.pdf/. Accessed Jan 25, 2022. 8. Centre for Health Protection. Department of Health. The Food Pyramid - A Guide to a Balanced Diet. Available at https://www.chp.gov.hk/en/static/90017.html/. Accessed Jan 25, 2022. 9. Zhang T, Huang B. Int J Environ Res Public Health 2018; 15(10): 2247. 10. World Health Organization. Using price policies to promote healthier diets. Available at https://www.euro.who.int/__data/assets/pdf_file/0008/273662/Using-price-policies-to-promote-healthier-diets.pdf/. Accessed Jan 25, 2022. 11. Chung LMY, et al. Nutrients 2021 ; 13(2): 333. 12. Pope L, et al. Nutrients 2021; 13(5): 1674. 13. Rivera Medina C, et al. Nutrients 2020; 12(5): 1408. 14. Utter J, et al. J Nutr Educ Behav 2018; 50(5): 494-500.





