The Clinical Impacts of COVID-19 on Patients with Atopic Dermatitis
Atopic dermatitis (AD) is a disease with a complex pathophysiology involving immune-mediated reactions leading to skin lesions that are typically localised and recurrent. While the COVID-19 pandemic is still growing rapidly, its impacts on the outcome of AD have gained clinical concern. In particular, the influence of immunosuppressants used in AD on the course of COVID-19 infection is a challenging clinical problem in managing AD during the current pandemic. While vaccines against COVID-19 are the most effective weapons to prevent infection, or to make it less aggressive, clinical data on their safety in AD patients are limited. Here, this article aims to review certain clinical issues of COVID-19 in patients with AD.
Risk of COVID-19 Infection among AD Patients
The pathophysiology of AD is complex and multifactorial, which is known to involve immune dysregulation and environmental factors. Of note, AD is characterised primarily by Th2 skewing, with an increased susceptibility to viral infections. Moreover, elevated expression of Th2 cytokines in serum, such as IL-4, IL-10 and IL-13, was reported in patients with COVID-19, especially during the cytokine storm1. This leads to concerns on the risk for COVID-19 incidence among patients with AD.
In a recent case-control study by Fan et al (2021), health data from 58,760 adults identified in the National Institutes of Health database were analysed. In the cohort, there were 11,752 cases of AD and 47,008 matched controls. The results indicated that patients with AD were more likely to have a diagnosis of COVID-19 (4.2% vs 2.8%, P <0.001) compared to controls. Additionally, AD patients were more likely to have other diseases, such as hypertension, type II diabetes mellitus (DM), autoimmune diseases, and etc. However, AD remained significantly associated with COVID-19 diagnosis after adjusting for demographic factors and comorbidities (odds ratio [OR]: 1.29, p <0.001)2.
In another large-scale population-based retrospective cohort study, which included 39,417 AD cases and 397,293 non-AD controls, a small increased risk of contracting COVID-19 was indicated among adults with AD (incidence rate ratio [IRR]: 1.18), after adjusting for demographic factors and baseline comorbidities3. Although certain factors such as the issues of asymptomatic infections and the fact of more frequent visit to healthcare facilities for AD patients were not considered in the population-based studies above, the consistent findings in the large-scale studies suggested the potential increased risk of COVID-19 infection among AD patients.
Multi-dimensional Impacts of COVID-19 on AD Patients
Besides the potentially increased risk of COVID-19 infection, the severity of complications in AD patients infected with the virus is noteworthy. Although no skin conditions are included on the Centers for Disease Control and Prevention (CDC) list of COVID-19 risk factors4, the broad spectrum of clinical responses observed in the course of COVID-19 is largely associated with comorbidities and conditions modifying immunity, which may worsen the course of infection. Moreover, the use of immunosuppressants against AD may predispose patients to a more severe course of COVID-19.
In a nation-wide cohort study by Yang et al (2020), which included health data obtained from the Health Insurance Review & Assessment Service of Korea, the association between allergic disorders, including AD, allergic rhinitis and asthma, and COVID-19 and the clinical outcomes were analysed. There were totally 219,959 patients included in the analysis, among which 136 patients were with AD and tested positive for COVID-19. The results showed no significant association between AD and severe clinical outcomes of COVID-19, whereas the mean length of hospital stay were 22.3 days and 22.4 days in patients with and without atopic dermatitis, respectively5.
On the other hand, in a web-based survey evaluated the impact of COVID-19 among AD patients by Hernández et al (2021), 116 out of 155 (75%) AD patients reported AD worsening, and 59.4% of the patients reported sleep problems. Uncertainty, anxiety and pessimism were frequent during the pandemic. Nonetheless, only 1.3% of the patients were tested positive for COVID-19, whereas the results suggested that COVID-19 infection was not significantly associated with disease flaring, psychiatric disorders, sleep disturbances or immunosuppressive therapy. Remarkably, compared with the periods before and during pandemic, significant differences were observed in economic dependence and monthly income6. This highlighted the social and economic effects of the pandemic on AD patients.
Apart from the pathophysiological impacts, it is essential to be aware of the psychosocial implications of COVID-19. Currently, many countries/regions adopt mass quarantine or isolation measures as a public health strategy to limit the spread of the contagion. Clinical opinions addressed that quarantine/isolation measures have been associated with a range of psychopathological conditions including emotional exhaustion, irritability, anxiety, increased anger and symptoms related to depression and post-traumatic stress disorder (PTSD)7. Notably, increased psychosocial stress may have an impact on the course of many common 'stress-responsive’ skin conditions including AD8. Hence, it is advisable to deal with short-term and long-term psychosocial effects related to the COVID-19 pandemic on AD patients.
Management of AD in the COVID-19 Era
While immunomodulatory medications are commonly prescribed in the management of moderate-to-severe AD or those recalcitrant to topical therapy, immunocompromised patients are highly vulnerable to infections, which is concerning during the current pandemic. For instance, systemic corticosteroids are immunosuppressive medications used to treat AD flares. However, former reports suggested that systemic corticosteroids are associated with increased infection risk. Thus, oral corticosteroids should be avoided to prevent COVID-19 susceptibility9.
Due to the inhibition of specific cytokines, biologic medications are potentially increased susceptibility to and severity of infection. Of note, anti-TNF-α therapies inhibit a crucial immunological pathway, an immunosuppressive effect and increased infection risk are therefore expected. Hence, previous comment suggested that anti-TNF-α biologics should be held during active infection, whereas in uninfected/asymptomatic patients, safer and more effective alternatives should be considered9. Nonetheless, interleukin (IL)-17, IL-12/23 and IL-23 inhibitors are reported to associate with low infection risk, with IL-17 and IL-23 favoured over IL-12/23 inhibitors9.
Undoubtedly, vaccines are the most effective weapons to prevent COVID-19 infection, or to reduce its severity. However, clinical trial data on the efficacy or safety of vaccines against COVID-19 in patients affected by chronic inflammatory diseases on immunosuppressive therapy are not available because these patients are naturally excluded from the trials. Dupilumab is a fully human monoclonal antibody, which inhibits the function of IL-4 and IL-13, for the treatment of moderate-to-severe AD. Notably, Ungar et al (2021) demonstrated that patients with moderate-to-severe AD treated with dupilumab (n = 632) showed reduced incidence and severity of COVID-19 symptoms as compared to those treated with other systemic treatments (n = 107) or limited/no treatment (n = 498) (Figure 1)1. This suggested that dupilumab may have a protective effect on antiviral immune response in AD patients. Moreover, a case series of 3 AD patients infected with COVID-19, in which mild outcomes were observed, demonstrated that dupilumab treatment in AD patients with mild-to-moderate COVID-19 should not be discontinued. Nonetheless, careful assessment is needed for each patient10.
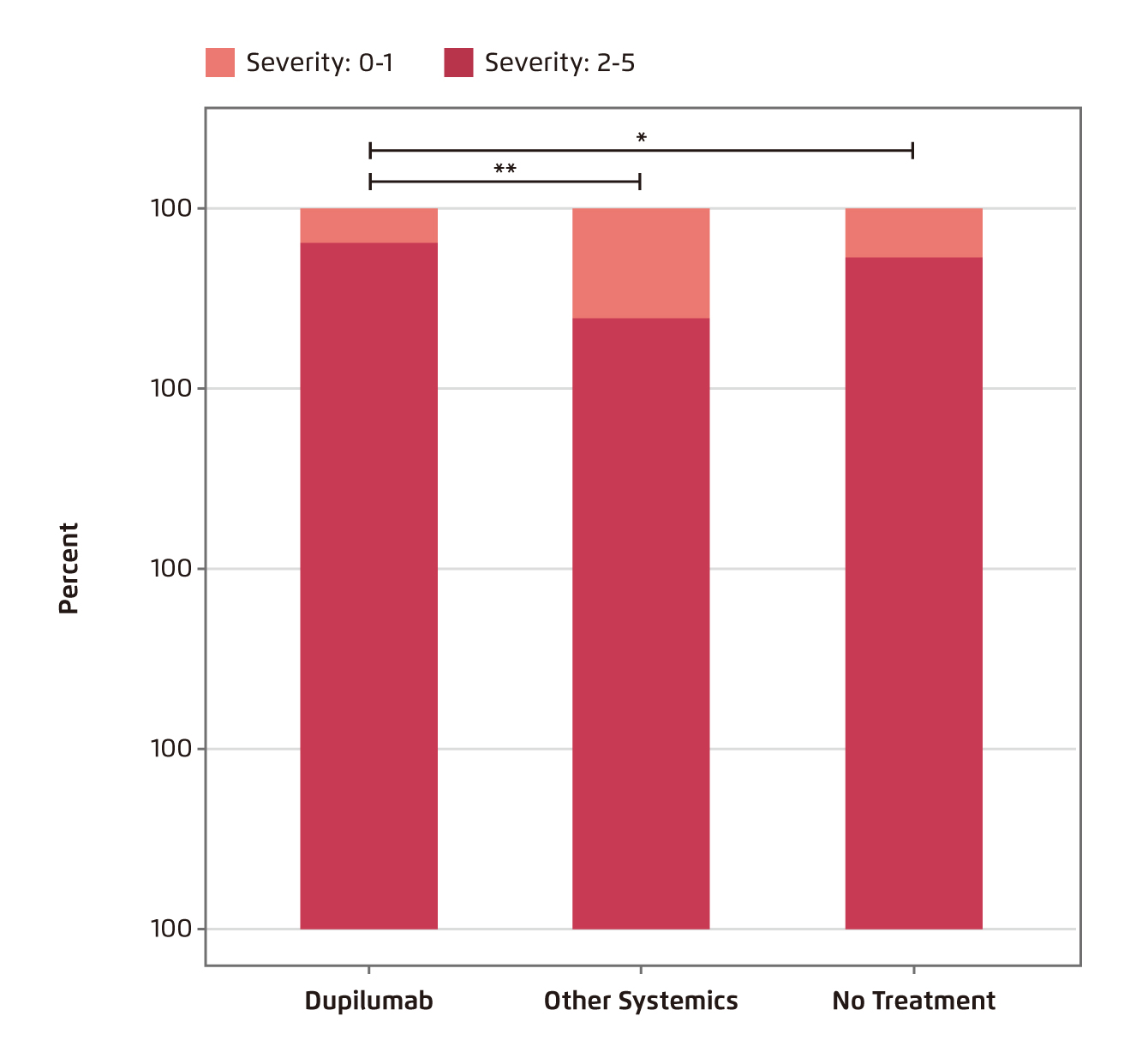
Figure 1.
COVID-19 symptoms in AD patient cohort grouped by treatment1
Summary
While patients with AD appear to have increased risk of COVID-19 infection, the pathophysiological impacts of the infection are comparable to those without AD. However, the potential psychosocial and economic impacts of AD during the current pandemic are noteworthy. Of importance, although clinical trial data on the efficacy or safety of vaccines against COVID-19 in AD patients is unavailable, the current state of knowledge and existing literature suggesting there are no contraindications to vaccinating people with AD, either on immunosuppressive therapy or on dupilumab therapy. To eradicate the COVID-19 pandemic, eligible people should take prompt action and get vaccinated.
References
1. Ungar et al. J Allergy Clin Immunol Pract 2022; 10: 134. 2. Fan et al. JAAD Int 2022; 6: 77. 3. Wu et al. J Am Acad Dermatol 2022; 86: 243-5. 4. CDC. Evidence for Conditions that Increase Risk of Severe Illness. 2021. 5. Yang et al. J Allergy Clin Immunol 2020; 146: 790-8. 6. Hernández et al. World Allergy Organ J 2021; 14: 100571. 7. Polšek et al. Croat Med J 2020; 61: 306. 8. Garcovich et al. J Eur Acad Dermatology Venereol 2020; 34: e293-4. 9. Ricardo et al. Dermatol Ther 2020; 33. DOI:10.1111/DTH.13687. 10. Ceryn et al. Clin Cosmet Investig Dermatol 2021; 14: 1131-8.