Associate Consultant,
Honorary Clinical Assistant Professor,
Department of Medicine,
Queen Mary Hospital, University of Hong Kong
Combating Relapsed and Refractory Multiple Myeloma in Local Clinical Setting
While the development of immunomodulatory drugs (IMiDs) has significantly improved the survival of patients with multiple myeloma (MM), proper management of relapse/refractory disease (RRMM) remains challenging for frontline clinicians. In a recent sharing, Dr. Gloria YY Hwang of the Queen Mary Hospital presented the clinical management and the outcomes of a RRMM patient treated with IMiDs.
Background of the Patient
The patient was a 53-year-old female with good health record. In 2010, the patient presented with some bone pain and proteinuria (2.5 g/day). However, evaluation on albumin level did not indicate renal impairment.
Dr. Hwang claimed that the only abnormality observed in the patient at the time of presentation was the significantly increased alkaline phosphatase (ALP) level (467 U/L), which supported the diagnosis of MM. Subsequent serum protein electrophoresis (SPE) exhibited a weak monoclonal band. Moreover, the free light chain analysis revealed elevated free kappa (725 mg/L) and skewed kappa/lambda free light chain ratio (98.77). In the urine protein electrophoresis, 63.7% of free kappa bands was found in the urine.
Skeletal survey reflected no abnormal lytic lesion. Although bone scan was not recommended as a standard imaging assessment in myeloma, the procedure was one of the options for diagnosis in the resource-limited setting in a decade ago. In particular, the bone scan detected multiple foci of uptakes in bilateral ribs (Figure 1A) and left calcaneum (Figure 1B). The observations explained the chest pain complained by the patient and the elevated ALP. Besides, renal biopsy showed no immunoglobulin or light chain deposits. Nonetheless, results of bone marrow examination confirmed the diagnosis of MM.

Figure 1.
Bone scan showing multiple foci of uptakes in (A) bilateral ribs and (B) left calcaneum
Non-responsive to Initial Lines of Treatments
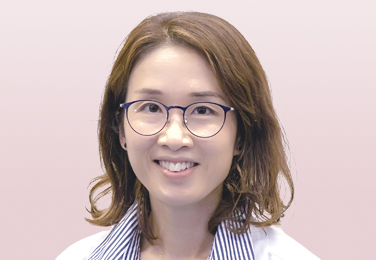
While MM was diagnosed, Dr. Hwang prescribed the first-line bortezomib, thalidomide, and dexamethasone (VTD) treatment. “The choice of this treatment mainly because it was supported by the government as a front-line option in that generation,” she addressed. Unfortunately, the patient did not respond to the treatment that the free kappa level increased after 6 cycles of treatment (Figure 2). Repeated bone marrow examination after 6 cycles of first-line treatment showed persistent myeloma, whereas the condition of proteinuria remained static (2.8 g/day) with slightly elevated serum creatinine (97 µmol/L). Moreover, bone scan showed similar uptake in bilateral ribs.
Figure 2.
Free kappa level of patient after first-line VTD treatment
Dr. Hwang prescribed lenalidomide with dexamethasone (Rd) therapy as second-line treatment. However, the second-line therapy yielded no response as reflected by the high free kappa level (Figure 3). Hence, the patients was off-treatment from September 2012 to early 2015 since treatment option available was limited and the patient’s myeloma status remained static with no increase in free kappa level nor worsening of renal function. The patient did not complained on any adverse conditions during the period.
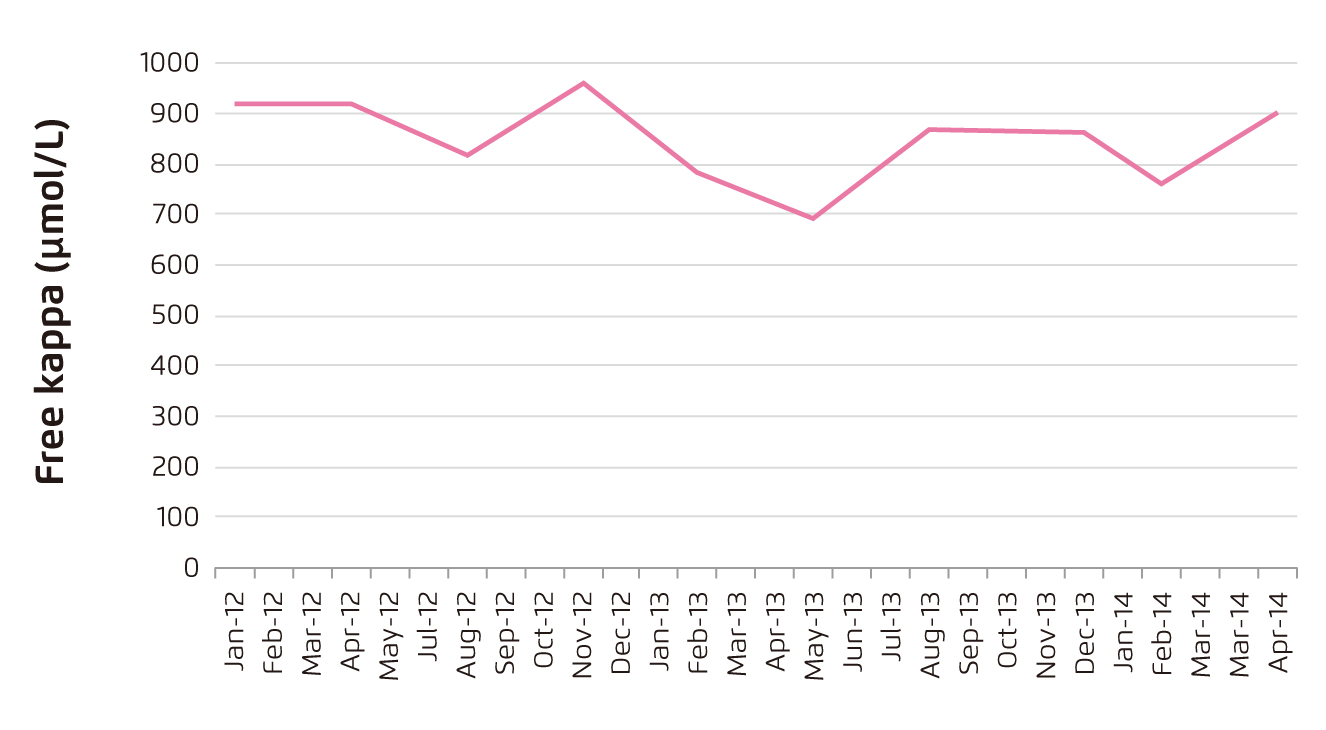
Figure 3.
Free kappa level of patient after second-line Rd treatment
Later in 2015, worsening of patient’s kidney function was noticed with an elevated serum creatinine (130 µmol/L). Additionally, the free kappa was found to have increased (1,940 mg/L). Repeated bone marrow examination showed that 35% of plasma cells were CD20 positive (CD20+). Fluorescence in situ hybridisation (FISH) identified no translocation of t(4;14), gain of chromosome 1q or deletion of 17p. Nonetheless, PET/CT scanning detected numerous lytic lesions in the skull bone and hyper-metabolic fractures in bilateral ribs (Figure 4). In order to control the disease, Dr. Hwang prescribed 5 cycles of velcade-bendamustine-dexamethasone (Vbenda-Dex) treatment between October 2015 and January 2016. Unfortunately, the treatment yielded no response again.
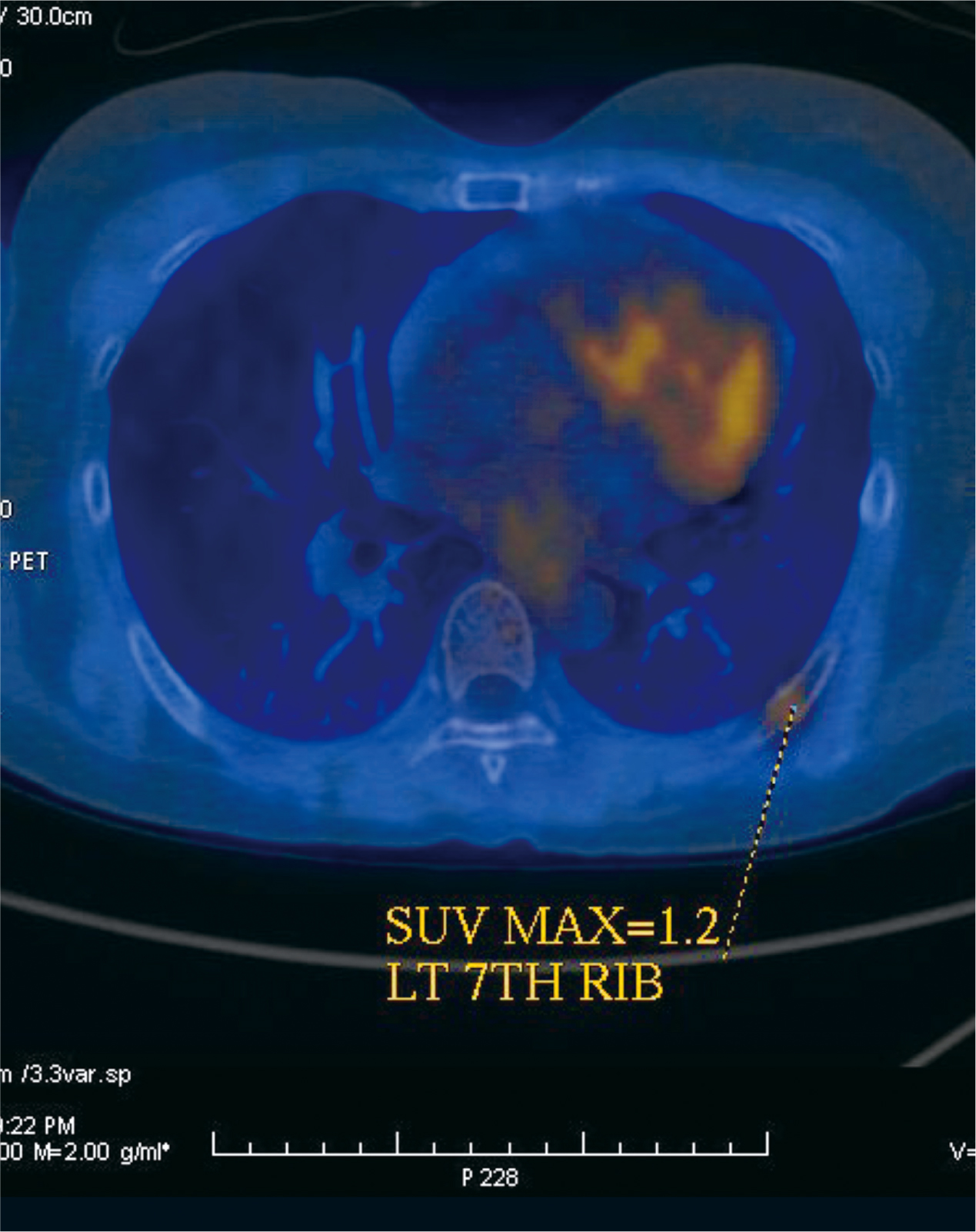
Figure 4.
Hyper-metabolic fractures in bilateral ribs detected in 2015
Therapeutic Outcomes of Pomalidomide-based Treatment
In February 2016, there was a local trial conducted to investigate the efficacy of pomalidomide and the patient was recruited in the trial. The patient was treated with pomalidomide (4 mg/day) with dexamethasone (Pd). The free kappa level was found to decrease dramatically with the treatment. In response to the rise in free kappa level in April 2016, oral cyclophosphamide was prescribed in June 2016 and hence free kappa level reduced (Figure 5).
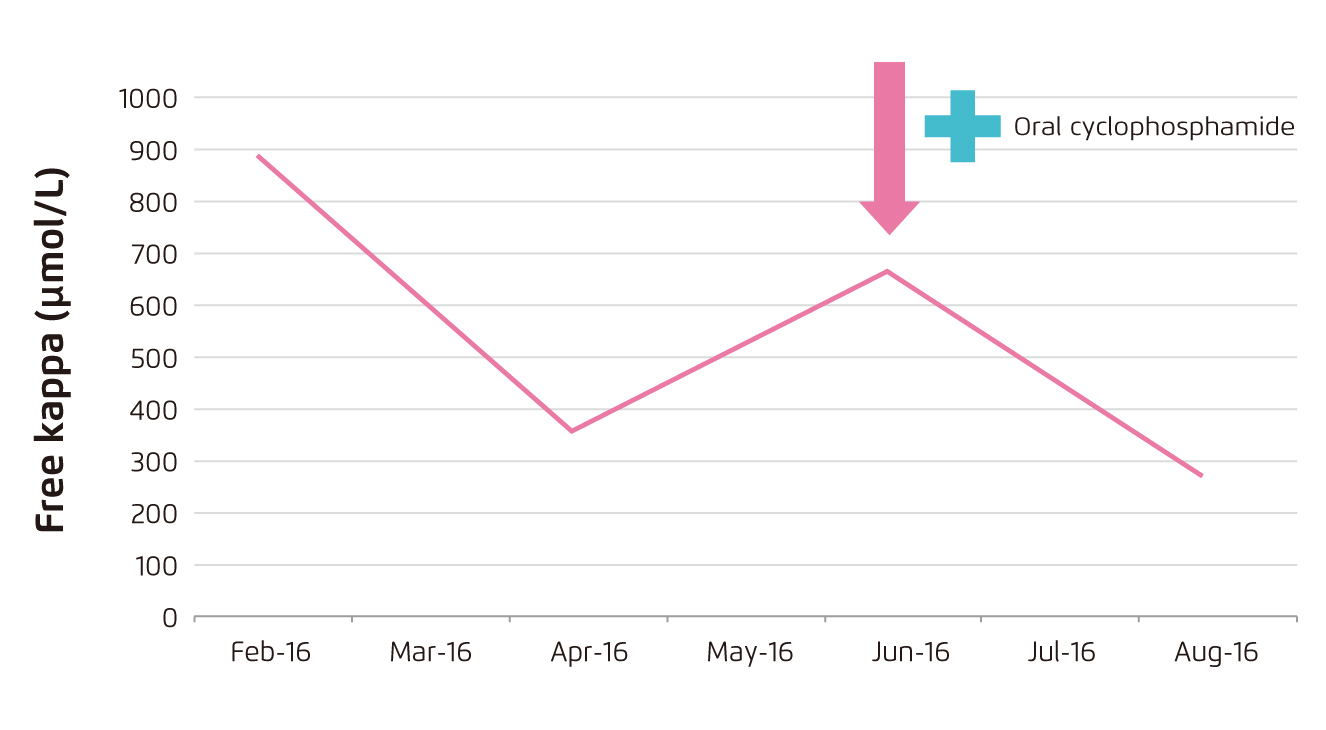
Figure 5.
Decrease in free kappa level upon Pd treatment
Dr. Hwang commented that the patient responded very well to the Pd treatment. Although the patient complained on worsening of bone pain and decline in renal function was detected in April 2018, repeated bone marrow examination indicated no worsening of myeloma that 3.8% of plasma cells were CD20+. In view of the patient’s condition, daratumumab and ixazomib was prescribed since April 2018 and the treatment yielded promising response as reflected by significant reduction in free kappa level. In August 2019, the patient underwent autologous hematopoietic stem-cell transplantation (HSCT) with melphalan conditioning, followed-up with pomalidomide-based treatment (Figure 6).
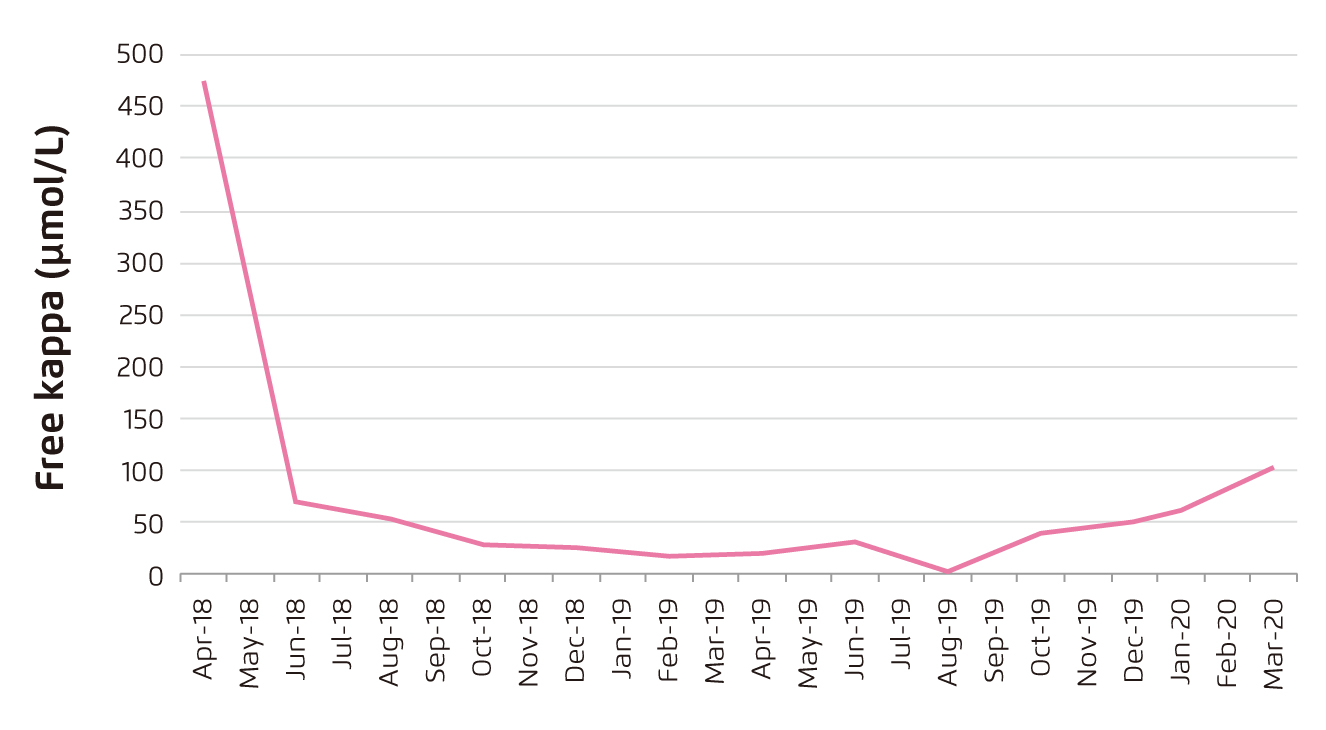
Figure 6.
Long-term efficacy of pomalidomide-based treatment
In the last follow-up in March 2020, no increase in CD20+ plasma cells was observed, whereas free kappa level was 86.9 mg/L and free lambda level was 45 mg/L (kappa/lambda free light chain ratio: 1.93). Moreover, the proteinuria was resolved. The patient has been treated with 4 mg pomalidomide 3 times per week since August 2019.
Summary
The current case visualises the difficulty in managing refractory MM in local clinical settings a decade ago, when there was limited treatment options. While the patients showed no response to the initial lines of treatment, pomalidomide-based treatment yielded promising outcomes and the treatment benefits were shown to be sustainable.