
Dietary Management of Metabolic Acidosis in Chronic Kidney Disease
Metabolic acidosis is an acid-base disorder common in patients with chronic kidney disease (CKD) when the glomerular filtration rate (GFR) falls below 30-40 mL/min/1.73 m2 1,2. It is often associated with increased risks for kidney disease progression and mortality, and correction of acidosis may improve kidney function and slow the progression of CKD2,3. Although metabolic acidosis can be corrected with pharmacological administration of oral alkali as sodium bicarbonate, correction can be achieved with an increased intake of fruits and vegetables and a low-protein diet with a greater use of vegetable proteins1,4,5.
Defining Metabolic Acidosis
The kidneys play an extremely important role in regulating the acid-base homeostasis of the body by excreting nonvolatile acids as ammonium ions (NH4+) and titratable acid in urine, reabsorbing the filtered bicarbonate ions (HCO3-) and generating new bicarbonate2-4,6. As renal function declines, reductions in the excretion of nonvolatile acids and the reabsorption and regeneration of bicarbonate occur, resulting in acidaemia and consumption of bicarbonate in order to buffer the acid retained4,7. In fact, metabolic acidosis is a hallmark of patients with advanced CKD8.
Metabolic acidosis is clinically defined as serum bicarbonate concentration <22 mmol/L, and is a common complication of CKD when the GFR falls below 30-40 mL/min/1.73 m2, accounting for 2.3-13% of patients with Stage 3 CKD and 19-37% of those with Stage 4 CKD1,2,4. It is often associated with increased risks for kidney disease progression, bone demineralisation, skeletal muscle catabolism and mortality3. As a risk factor for the progression of CKD, timely correction of chronic metabolic acidosis is essential2.
Correction of Metabolic Acidosis
To maintain normal serum bicarbonate concentrations, clinical practice guidelines recommend alkali therapy for CKD patients with serum bicarbonate concentrations of
<22 mmol/L9. However, while clinical evidence of the efficacy and safety of oral alkali in correcting metabolic acidosis in CKD patients has yet to be established, prevention and correction of chronic metabolic acidosis can be achieved through dietary modifications. In fact, diet is known to be the most important individual factor affecting acid-base status, whereas the types of diets strongly affecting acid-base balance are those providing acid or base precursors2-4.
Acid and Alkaline Foods
Under normal circumstances, the daily acid load is largely determined by the metabolism of dietary constituents to hydrogen ions (H+) and bicarbonate (base). The hydrogen ions are produced mostly from the metabolism of the sulfur-containing amino acids methionine and cysteine, and cationic amino acids such as lysine, arginine and histidine, whereas base is produced from the metabolism of anionic amino acids like glutamate and aspartate, and organic anions such as citrate and malate2-4,6,10. Also, the type of protein affects the acidity of the diet. Animal proteins have an elevated amount of phosphorus that contributes to acidification of body fluids. Vegetable proteins, on the other hand, have phosphorus in the form of phytate, which is less bioavailable and does not have the same acidifying effects4. Fats and sugars, unless incompletely metabolised, have only a small effect on acid-base balance5. In addition, an increased intake of dietary salt, such as through heavy consumption of processed foods, is associated with an increase in net acid production and a decrease in the concentration of serum bicarbonate4,5,11.
In general, meat, eggs, cheese and fish are foods with the highest acid loads, while fruits and vegetables have a high alkalising potential (Figure 1)2,4. However, some fruits, such as cranberries, prunes, plums and some berries, contain benzoic and quinic acids, which are metabolised by gut bacteria to hippuric acid, and can increase acid excretion5. Citrus juices are rich sources of citrate and can therefore be nearly completely metabolised to bicarbonate. However, the consumption of citrus juices and fruit juices should be limited because of the high energy, sugar and potassium content2. Milk is considered neutral, as its quantity of phosphorus can be compensated by that of calcium4.
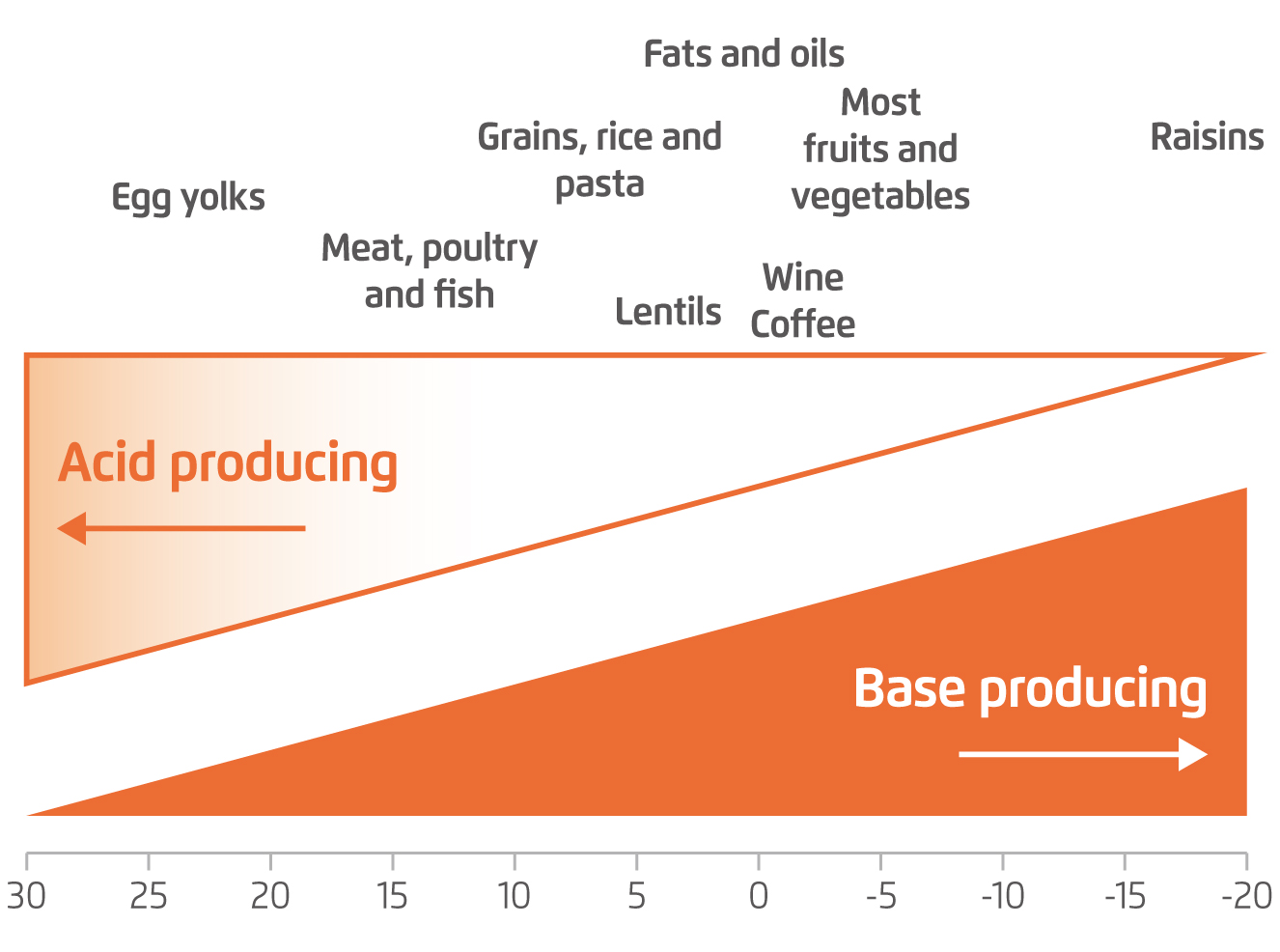
Figure 1.
Estimated potential renal acid load of common foods per 100-g serving3
Since metabolism of potassium salts, such as citrate and malate, leads to an alkalising effect, the quantity of potassium of the food, by and large, indicates its alkalising ability. However, oxalate can form potassium oxalate, which cannot be metabolised, and therefore does not provide any alkali to the body4,5. As many fruits and vegetables are relatively rich in potassium, patients with impaired renal function should receive comprehensive dietary counselling, which should be followed up closely to avoid electrolyte alterations such as hyperkalaemia2.
Dietary Strategies for Managing Metabolic Acidosis
Dietary strategies for managing metabolic acidosis in CKD include reducing the dietary acid load through a low-protein diet with replacements of vegetable proteins, and increasing the intake of base-producing foods such as fruits and vegetables3-5.
Low-protein diet with replacements of vegetable proteins
Low-protein diets have been used in the management of CKD to slow progression of the disease for more than a century5. However, metabolic acidosis may not be effectively controlled by restriction of dietary protein alone, though the high protein content of the diets may contribute to an increased proportion of acid equivalents2,4. As net endogenous acid production also depends on the type of protein, replacing animal proteins with vegetable or plant-based proteins could help cut back on acid production2,4,12. The soy protein, which has gained in popularity in recent years, is considered beneficial for both the kidney disease and metabolic acidosis as it helps reduce the total ingestion of animal protein as well as the dietary acid load4.
Increased intake of fruits and vegetables
Recent studies have shown that adding fruits and vegetables reduces urine net acid excretion in CKD patients with reduced estimated GFR (eGFR) but without metabolic acidosis, and improves metabolic acidosis in those whose eGFR are low enough to be associated with metabolic acidosis. In these studies, the fruits and vegetables prescribed were in amounts equivalent to 50% of the calculated dietary acid load, which amounted to adding 2 to 4 cups of fruits and vegetables per day. Nevertheless, patients involved in these studies were carefully selected to be at very low risk to develop hyperkalaemia in response to the increased potassium load brought by fruits and vegetables11. In fact, as long as serum potassium concentration permits and is monitored, nutritional alkali therapy with fruits and vegetables is warranted in most CKD patients, even those without metabolic acidosis3.
Low-protein diets with increased use of vegetable protein, together with increased consumption of fruits and vegetables, reduce the amount of acid to be managed by the kidneys. This helps reduce stimulating angiotensin II, aldosterone and endothelin, which are required to excrete dietary acid, and accumulating ammonia within the kidney, thus reducing kidney damage5.
References
1. Di Iorio BR, et al. Nutrients 2017;9(1):69. 2. Siener R. Nutrients 2018;10(4):512. 3. Raphael KL. Am J Kidney Dis 2019;47(2):263-275. 4. Angéloco LRN, et al. J Reb Nutr 2018;28(3):215-220. 5. Passey C. J Ren Nutr 2017;27(3):151-160. 6. Nagami GT and Hamm LL. Adv Chronic Kidney Dis 2017;24(5):274-279. 7. Stancu S, et al. Maedica 2018;13(4):267-272. 8. Carrero JJ, et al. Nat Rev Nephrol 2020;16(9):525-542. 9. Levin A, et al. Kidney Int Suppl 2013;3(1):1-150. 10. Poupin N, et al. Clin Nutr 2012;31(3):313-321. 11. Goraya N and Wesson DE. Adv Chronic Kidney Dis. 2017;24(5):298-304. 12. Kraut JA and Madias NE. Am J Kidney Dis 67(2):307-317.





