

Specialist in Clinical Oncology, Management Committee Member, HKBCF

Head of Breast Cancer Support Centre, HKBCF
Caring Bodies, Caring Minds
Treatments and Paramedical Support for Breast Cancer Patients and Survivors
Breast cancer remains the most common cancer among women both globally and locally. According to 2018 GLOBOCAN, approximately 2.1 million cases worldwide were diagnosed with breast cancer and about 630,000 died from the disease1. In Hong Kong, 4,618 women and 27 men were diagnosed with breast cancer in 2018, whereas the number of diagnosed female breast cancer cases has increased by 4 times from 1993 to 20182. Although a wide spectrum of therapies for breast cancer is currently available, the prognosis of the disease varies by different biological subtypes and stages. Moreover, the quality of life as well as mental wellbeing of the patients and their families would be adversely affected by the disease regardless of severity. In particular, a substantial proportion of breast cancer survivors would suffer from lymphoedema. Hence, long-term medical care and paramedic support are needed for the prevention and/or management of breast cancer-related complications. In a recent interview, Dr. Lawrence Li and Ms. Doris Cheung of the Hong Kong Breast Cancer Foundation (HKBCF) shared their expertise on breast cancer treeatment and their insights on holistic care for breast cancer survivors.
Overview of Breast Cancer Treatments
Dr. Li outlined that there are 3 major aspects for breast cancer treatment including surgery, radiotherapy and pharmacological treatment. For pharmacological treatment, in turns, there are 4 classes of therapies, namely chemotherapy, hormonal therapy, targeted therapy and immunotherapy. Patients with invasive cancer are usually treated with multimodality treatments, whereas less aggressive and local treatments are given to patients with in situ cancer. “Breast cancer stage and its biological subtype are the 2 factors governing the selection of treatments,” stated Dr. Li.
The biological subtype of breast cancer can be defined by hormone receptor (HR) expression and human epidermal growth factor receptor 2 (HER2) amplification. It has been reported that the median overall survival for patients with metastatic triple-negative breast cancer (TNBC) is approximately 12-18 months, compared to 35-55 months for HR positive/HER2-negative breast cancer3.
Dr. Li highlighted that HER2-positive cancers are generally more aggressive and at higher risk of recurrence than HER2-negative ones, thus targeted therapy coupled with chemotherapy is often required. Besides, multimodality treatments involving chemotherapy and immunotherapy are usually prescribed for TNBC. On the other hand, breast cancers of stage 0 or I can be treated with localised lumpectomy with radiotherapy, whereas total mastectomy with subsequent radiotherapy covering larger regions would be required for later stage diseases. Essentially, Dr. Li addressed that different types of treatment are associated with different outcomes, such as development of treatment-related side effects and the need for breast reconstruction surgery.
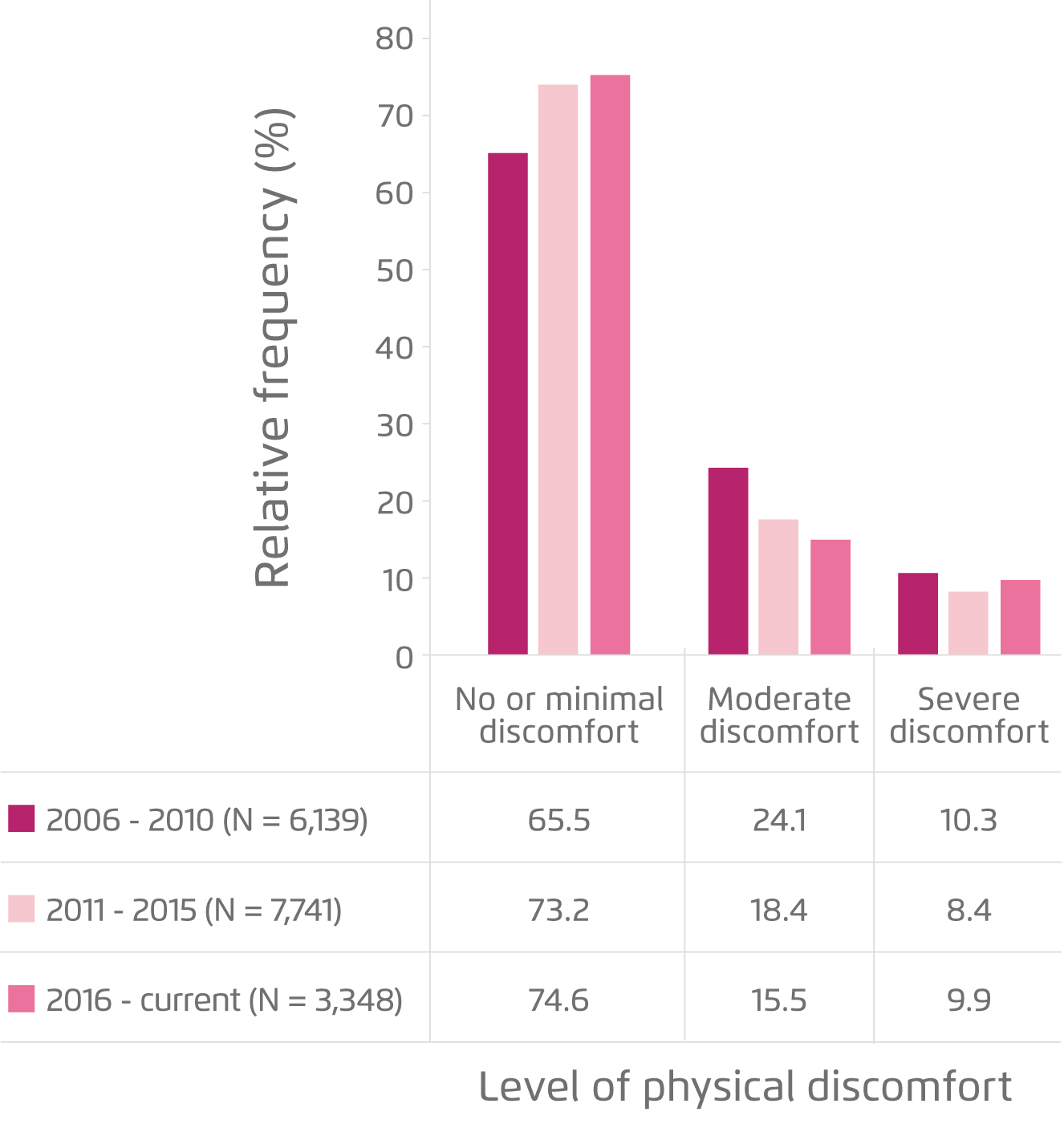
Figure 1. Level of discomfort after surgery4
After the Treatment
Dr. Li presented that the 10-year survival rate after treatment of breast cancer is almost 100% for stage 0, and over 90% for stage I, whereas that of stage II varies between 85-90%. However, as stage III breast cancer can be classified into several substages, the 10-year survival rate ranges between 60-70%. Clinically, stage IV diseases might not be curable, while the 5-year survival rate can reach 30%.
Besides survival rate, potential physical discomfort is often a concern for the survivors and their families. A recent investigation involving more than 17,000 local breast cancer patients recruited in 3 cohorts (2006-2010, 2011-2015 and 2016-current) in the Hong Kong Breast Cancer Registry (HKBCR) demonstrated that 74.6% of patients who had surgery experienced no or minimal physical discomfort, while 9.9% experienced severe discomfort (Figure 1). Wound pain was the most common form of discomfort after surgery4. Dr. Li stated that current treatments for controlling post-operative pain are effective in general. However, fibrosis occurred underneath the scar would trap peripheral nerve and cause pain, whereas the fibrous tissues would be tightened after prolonged period and thus further worsening the condition.
In the case of radiotherapy, about 74.0% of the patients reported no or minimal physical discomfort and 13.2% experienced severe discomfort, whereas dry skin and pain were the 2 most common forms of discomfort reported. On the other hand, 33.6% of patients received chemotherapy had no or minimal physical discomfort and 40.8% experienced severe discomfort (Figure 2). Notably, loss of appetite and weakness were the 2 most common treatment-related side effects reported after chemotherapy4. Of note, Dr. Li reminded that there are many types of newly developed targeted therapies, such as anti-HR positive targeted therapy, in addition to conventional anti-HER2 targeted therapy. Certain types of treatment-related side effect including neutropenia have been reported upon treatment with these new targeted therapies.
In reducing the impact of side effects experienced by the patients, Dr. Li addressed there are 2 aspects which frontline clinicians are responsible for. Particularly, he emphasised the importance of appropriate selection of treatment for the patients. “Potential side effects can be avoided when the appropriate therapies are selected,” claimed Dr. Li. He quoted that extensive axillary dissection may not be required for many breast cancers where sentinel lymph node removal can suffice, thus preventing the side effects of axillary dissection.
Dr. Li highlighted the clinical significance of personalised medicine. He mentioned that there are genomic tests of breast cancer currently available for providing comprehensive information on the biology of the patient's tumour and the risk of recurrence. Essentially, the test results help clinicians in evaluating the expected outcomes of chemotherapies and hence reducing the risk of adverse events by making the right choice of treatment.
Besides, management of the side effects by prescribing suitable medications is undoubtedly an important aspect to be handled by frontline clinicians in relieving the discomfort suffered by the patients. Notably, in addition to control symptoms, sometimes therapies are used for reducing the risk of developing side effects.
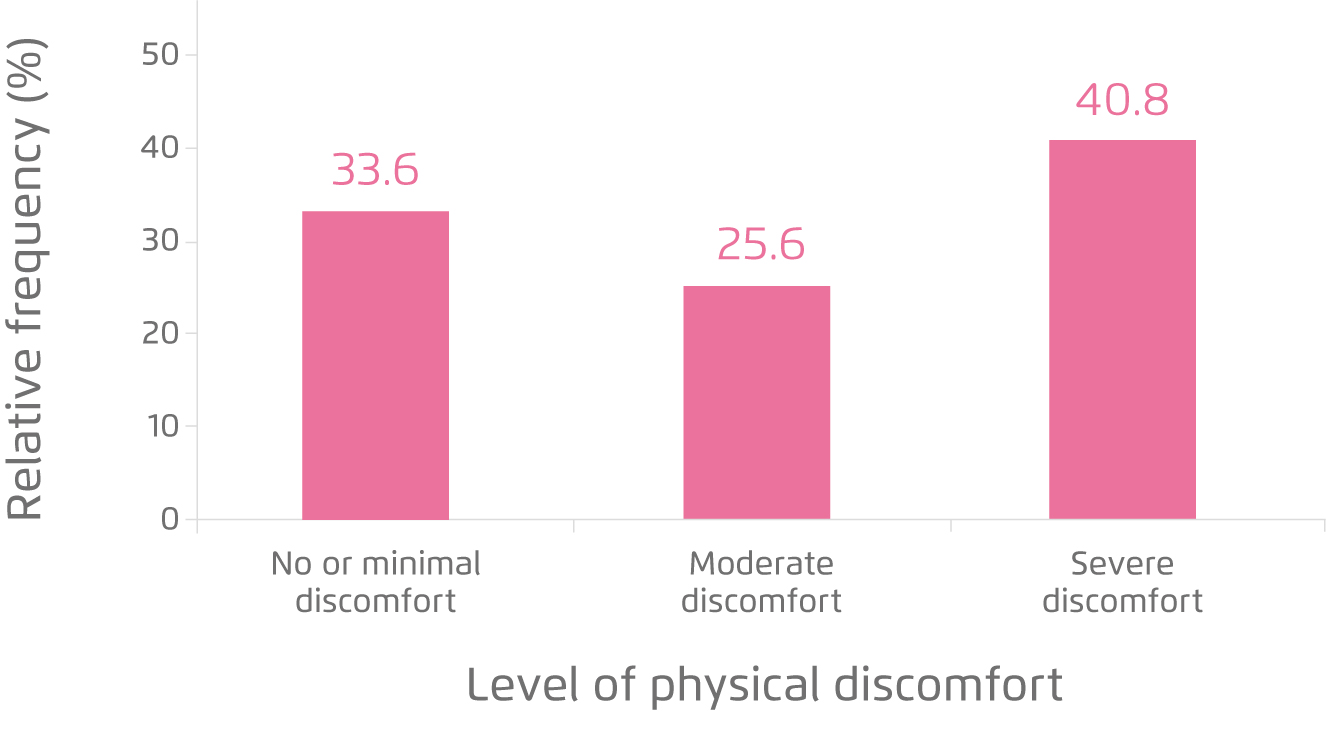
Figure 2. Level of discomfort after chemotherapy4
Psychological Distress of Patients, Survivors and Their Families
Emotional alterations are evident in patients suffering from breast cancer. A substantial proportion of patients (45.5%) perceived their diagnosis in a negative way. For instance, depression and lack of acceptance were reported by the patients, whereas 61.7% of patients after treatment felt life is unfair4. Besides, former report suggested that husbands make up of 30-40% of informal caregivers in chronic diseases, whereas they might fear that they would not be able to support and provide proper care for their wives. Hence, evidence indicates high levels of psychological distress experienced by family caregivers, especially spouses of cancer patients5. Ms. Cheung stated that it is common for husbands of breast cancer patients to seek help in Hong Kong. Hence, the HKBCF provides supporting services not only for patients but also for their families including husbands, parents, and etc.
Ms. Cheung claimed that husbands play an important role in the rehabilitation of patients. In addition to fear and hopelessness, Ms. Cheung mentioned that many patients worry about the feeling of their husbands. “Although reconstruction surgery is available, it is different from the original breast and breastfeeding might not be possible. The patients might worry their husbands would dislike them,” said Ms. Cheung. She expressed that it is stressful for the patients at the first time to show their husband the scar after surgery. Thus, the support by husbands is crucial in preventing psychological distress for the patients. In particular, accompany by the husband is important for the patients.
Practically, husbands need to manage the family duties during the recovery of the patient and they also need to help the patients on certain discomfort. Nonetheless, Ms. Cheung highlighted that the practical mindset of husbands might not meet the emotional needs of their wives. Remarkably, education for husbands on the proper way to face the changes in the patients is of great importance. Ms. Cheung stated that some husbands may not know how they can help the patients, such as handling emotions of the patients. Hence, professional guidance and counselling for husbands and family members are required.

Figure 3. Operation of device for measuring lymphoedema index by qualified lymphoedema therapist
The Burden of Lymphoedema and Its Management
Breast cancer-related lymphoedema (BCRL) is the accumulation of lymph fluid in the interstitial space due to insufficient drainage upon damage to the axillary lymphatic system after surgery or radiotherapy for breast cancer. BCRL can cause disfigurement, physical discomfort, and functional impairment. In addition, anxiety, depression, and emotional distress are more common in patients with BCRL6. While BCRL significantly affects the quality of life of breast cancer survivors, Ms. Cheung stated that the job duties of patients may be affected by condition as well. Besides, she presented based on the retrospective data at the HKBCF involving more than 5000 patients that the estimated local prevalence of BCRL was 35.4% of breast cancer survivors.
The level of BCRL is represented by the lymphoedema index, which provides information on the volume of the intracellular and extracellular fluid in the affected limbs. The index can be measured by passing small electrical currents through the limb and measuring the resistance of the current flows (Figure 3). Ms. Cheung explained that lymphoedema index ≥10 indicates the occurrence of lymphoedema, whereas the lymphoedema index of about 270 was observed in the most extreme case.
Dr. Li mentioned that the risk of developing BCRL depends on both patient factor, such as obesity, and the treatment received, particularly the type of surgery and radiotherapy. Essentially, he emphasised that patients at risk of BCRL need to routinely mobilise the shoulders in order to facilitate the flow of lymph fluid. Although shoulder mobilisation exercise has to be a long-term practice for the patients to prevent BCRL, Ms. Cheung said many patients especially those with late onset of BCRL would not be aware of the condition. Hence, continuous education enhancing patients’ awareness on BCRL is needed.
At present, there is no cure for BCRL. Thus, preventing fluid accumulation in the affected limb and regular monitoring on the lymphoedema index are crucial. Upon the onset of BCRL, physiotherapy including shoulder exercises and manual lymphatic drainage may reduce further lymph fluid accumulation. Importantly, education on self-care by the patients is essential in the long-term management of BCRL.
Organisational Support for Holistic Care
Obviously, the physiological and psychological burden of breast cancer imposed on the patients and their families are substantial, whereas psycho-oncological support is urgently needed. Dr. Li said that there are some sponsorship schemes provided by pharmaceutical companies on the medical costs of genomic tests or innovative breast cancer therapies for the patients. Nonetheless, both Dr. Li and Ms. Cheung commented that local psycho-oncological support is inadequate. For instance, Dr. Li addressed that the clinical care and counselling for patients and their families required not only sufficient resources and manpower but also time, it is difficult to cater all the patients’ needs in real-life clinical setting. Furthermore, Ms. Cheung added that the follow-up period for each patient in their centre ranges from 6-9 months, during which rehabilitation training and counselling services are provided for both patients and their families. These facts highlight the demand on resources in local psycho-oncological support.
To conclude, Dr. Li noted that the division of labour among professionals of different disciplines such as counsellors, nurses and qualified lymphoedema therapist is very helpful in optimising the health outcomes for the patients and ensuring the wellbeing of their families. Hence, organisations such as the HKBCF which provide holistic care for breast cancer patients and their families are highly desirable.
References
1. Bray et al. CA Cancer J Clin. 2018;68(6):394-424. 2. Hong Kong Breast Cancer Foundation. Breast Cancer - Local Statistics. 2020. 3. Weiss et al. Cancer Med. 2020. 4. Hong Kong Breast Cancer Foundation. Hong Kong Breast Cancer Registry Report No. 12. 2020. 5. Barani et al. Asian Pacific J Cancer Prev. 2019;20(10):3167-3172. 6. Lacomba et al. BMJ. 2010;340(7738):140.





