

Chair Professor
Department of Medicine & Therapeutics
The Chinese University of Hong Kong
Big Data Analysis and the JADETM Program
In clinical practice, there are large amounts of data generated from patient record keeping. Nowadays, most of these medical data are digitised which can be used to support a wide range of functions, such as clinical decision, quality assurance, disease surveillance and population health management1. The use of big data analysis to improve quality and efficiency of care for chronic diseases, such as diabetes mellitus (DM) may reduce healthcare expenses and disease burden. There are more than 230 million individuals living with DM in Asia, which accounts for 55% of the world’s DM population2. A previous survey suggested that 4.5% of people in Hong Kong of working age had DM, portending a growing epidemic with increasing westernisation and personal affluence3. While there is global interest in the development of data-driven DM management programs, the Joint Asia Diabetes Evaluation (JADETM) Technology has been developed by physician scientists in Hong Kong since 2007 with proven effectiveness. The web-based technology enables care providers to set up a register for quality assurance whilst empowers users with personalised risk prediction and self management. It incorporates a care protocol to guide data collection for analysis by a validated risk engine to issue a personalised report with decision support. In a recent interview, Prof. Juliana Chan shared her experience and insights during the design and implementation of the JADETM assisted integrated care (JADETM Program).
Big Data in Medicine
Thanks to the advancement in data science and network technology, the medical industry has entered an era of big data in the 21st century. In medical terms, big data refers to all large and complex electronic health datasets that cannot be easily handled using conventional data management tools. The totality of data related to patient’s healthcare and well-being, constitutes a huge resource including electronic patient records, decision support systems (e.g. laboratory tests, imaging), clinical notes, prescriptions, emergency care data and articles in medical journals1.
Due to the huge healthcare and societal burden of chronic diseases, the use of big data analysis to improve health outcomes has received interest from many sectors. In 2019, Makino et al constructed a prediction model for diabetic kidney disease (DKD) and complications using artificial intelligence (AI) based on a big database consisting of electronic medical records (EMR) from 64,059 patients with an accuracy of 71% (Figure 1)4.
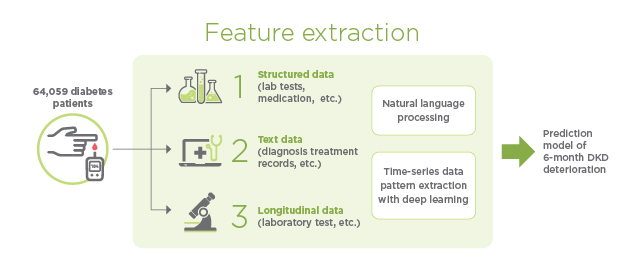
Figure 1. Clinical feature extraction for a prediction model of diabetic kidney disease (DKD) deterioration4
The Joint Asia Diabetes Evaluation (JADETM) Program
Prof. Chan commented that early detection and control of blood cholesterol, blood glucose, blood pressure and body weight in patients with diabetes mellitus (DM) can lead to long term benefits. “Both patients and clinicians need to recognise the additive effects of these common risk factors and the importance of attaining control of multiple treatment targets early,” she mentioned. Here, delivery of protocol-driven care has been confirmed to improve survival and clinical outcomes in patients with type 2 DM (T2DM)5. In order to combine the concepts of risk stratification and protocol-driven care, Prof. Chan’s team developed the JADETM Program in 2006, which aims at translating evidence to good clinical practice assisted by information technology in T2DM.
Clinical data of patients were systematically collected through a web-based portal (JADETM Technology) on an anonymous basis and encrypted in the database. The collected data were analysed automatically to stratify patients into several risk categories using a validated risk engine. Prof. Chan explained that the risk categories enable the care team to personalise and optimise care. One of the key objectives of the JADETM Technology is to enhance the quality of team-based care. The JADETM Program guides care providers to gather data systematically to stratify risk, empower patients and individualise care with decision support for both patients and physicians. The report generated contains trends and targets of four major modifiable risk factors, i.e. glycated haemoglobin (HbA1c), blood pressure and low-density lipoprotein cholesterol (LDL-C) and body weight with practice tips based on attained targets6. Using a validated risk engine, the estimated 5-year risk of major complications is displayed in bar charts to improve data visualisation. By turning these complex clinical data into an easy-to-read personalised report, we can use data to empower patients to improve self-management and facilitate physicians to individualise treatment plan (Figure 2).
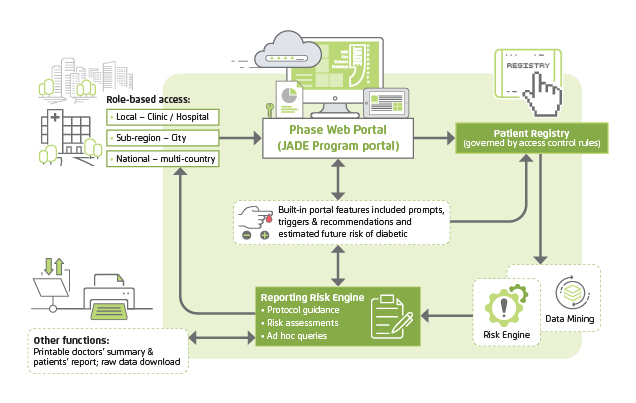
Figure 2. Logistics and components of the electronic portal of the JADETM Program6
The objective of the JADETM Program is to help practitioners establish a register, improve patient management and document improvement. Patients in different risk categories may have different health outcomes. A risk prediction tool along with an individualised care plan would enable a dialogue that helps physicians target specific risk factors and patients improve self-care through joint decision-making.
The Impacts of Big Data Analytics in DM Management
The utility of data-driven integrated care model in benchmarking performance and identifying care gaps has been reported. For instance, Yeung et al (2014) evaluated the control of risk factors in 41,029 patients from 245 outpatient clinics in 9 Asian countries or regions who were registered in the JADETM Program. Among these patients, 18% had young-onset DM (diagnosed before the age of 40 years) with a mean age at diagnosis of 32.9 years compared to 53.9 years amongst those with late-onset DM. Fewer patients with young-onset DM achieved HbA1c <7% than those with late-onset DM (27% vs. 42%, p<0.0001, Figure 3). Patients with young-onset DM also had higher mean HbA1c, LDL-C and were more likely to have retinopathy than those with late-onset DM7. These data highlight the value of using the JADETM Program to conduct collaborative international research. By promoting delivery of holistic and evidence-based care, the JADETM Technology also enables ongoing collection of real-world data using similar protocols to discover new knowledge.
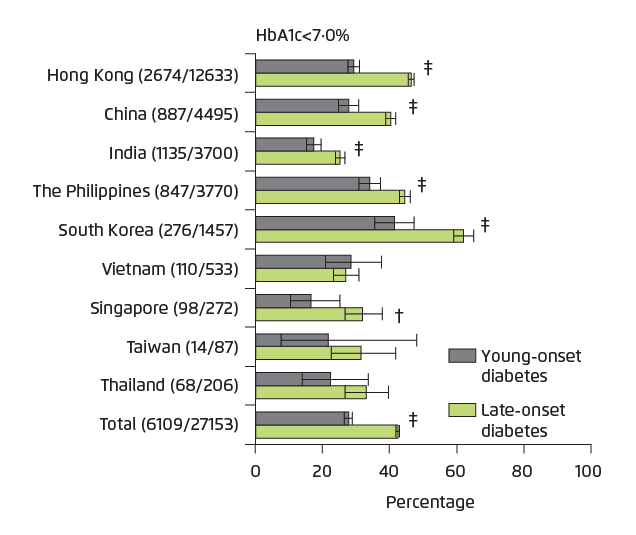
Figure 3. HbA1c attained by patients with young-onset versus late-onset T2DM in different Asian countries
(†p<0·01, ‡p<0·001; Error bars indicate 95% CI)7
Prof. Chan noted, “the JADETM Program creates research opportunities and career development for graduate students and different professionals such as data analysts, nurses, pharmacists, computer scientists and geneticists.” In particular, the creation, verification and management of big databases fosters a culture of knowledge discovery, sharing and application in all sectors. Besides, Prof. Chan mentioned that, the establishment of these big databases accompanied by biobanks, can provide huge opportunities for testing hypothesis and discovering biomarkers for the development of therapeutics for precision medicine through academic-industrial partnerships.
The benefits of using data to assist the delivery of evidence-based DM management have been proven. Tutino et al (2017) compared the effects of the JADETM Program versus and the Diabetes Monitoring Database (DIAMOND) Program. The DIAMOND portal contains the comprehensive assessment (CA) module of the JADETM Technology to guide data collection during annual assessment for risk stratification and personalised reporting with decision support. The JADETM portal contains an additional follow up (FU) module to facilitate structured FU visits. In a randomised trial, 3,586 Chinese patients with T2DM from 6 sites from 3 cities in China were randomised to DIAMOND or JADETM intervention, with the latter including at least two FU visits by nurses. After a median of 12.5 months, 2,559 patients returned for CA. The proportion of patients that attained ≥2 treatment targets (defined as HbA1c <7%, BP <130/80 mmHg, LDL-C <2.6 mmol/L) increased in both groups (JADETM: 40.6% to 50.0%; DIAMOND: 38.2% to 50.8%, Figure 4). The JADETM group was more likely to self-monitor blood glucose (50.5% vs 44.2%; p=0.005) and had fewer defaulters (25.6% vs 32.0%; p<0.001) compared to the DIAMOND group8. These results demonstrated that delivery of technology-assisted and data-driven integrated care improved attainment of multiple treatment targets. With additional support by nurses, implementation of the JADETM Program also improved health-related behaviours in patients with T2DM.
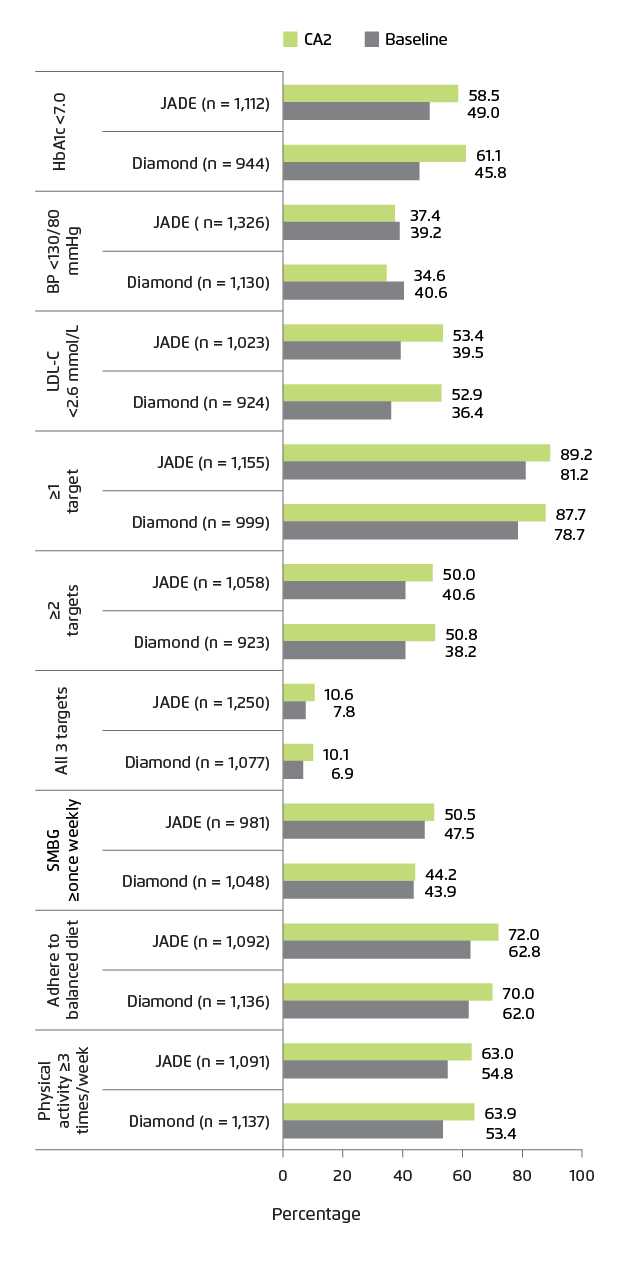
Figure 4. Proportions of patients attaining treatment targets at JADETM-assisted comprehensive assessment (CA2) at 1 year compared to baseline. All p-values for within-group comparison were <0.01 except for blood pressure (p=0.239)8
Scaling Up the JADETM Concept through Partnerships
Given the proven utility of the JADETM concept, the Hong Kong Hospital Authority (HA) integrated an adapted JADETM protocol in the territory-wide EMR and introduced structured risk assessment and management program in 18 hospital-based DM centres and primary care clinics. Meanwhile, Prof. Chan continued to promote the JADETM Program in other Asian regions by sharing best practices with adaptation to suit local needs.
To further scale up the JADETM Program in the community, Prof Chan’s team developed a mobile application (APP) of the JADETM Program through partnerships with other stakeholders. Patients who subscribed to the JADETM Program can access their personalised JADETM report with estimated 5-year predicted risks of complications, along with actionable recommendations. Other features of the JADETM APP or its enhanced version include reminders for CA/FU visits, interactive modules with care providers as well as information on DM from trustworthy sources. However, Prof. Chan commented that scaling up the JADETM Program requires strengthening of the infrastructure to provide both on-line information as well as face-to-face visits, using a “high tech, soft touch” approach. In this data era, the use of Applied Program Interface (API) also allows the JADETM Technology to cross-talk with other systems to promote collaborations.
Infrastructure aside, the involvement of front-line healthcare providers is critically important to ensure the successful implementation of the JADETM Program. In line with international recommendations, Prof. Chan suggested that front-line clinicians should encourage their patients to undergo structured assessment for risk factors and complications every 12-18 months. “This (structured assessment of risk factors and complications) is essential and important given their silent, progressive and interactive nature,” she commented. Front-line clinicians can refer patients to centres that implement the JADETM Program where trained nurses perform structured assessments guided by the JADETM protocol to issue personalised reports and educate/empower patients. The clinicians can use the JADETM report to explain the risk profiles to their patients and individualise treatment plan. Prof. Chan remarked that willingness to pay for these assessment and education programs is a challenge. Including the JADETM assessment and empowerment program as part of an insurance package may increase the adoption of the JADETM Program by medical groups to make this evidence-based care model more accessible and sustainable.
Prof. Chan commented that the trust between clinicians and patients is built on good clinical care, supported by evidence. To address the huge imbalance between private and public care, the JADETM Program can serve as a model where decades of academic research has been translated to an affordable tool to assist patients, care providers and payers make timely decisions in order to reduce the healthcare burden and societal costs of DM.
References
1. Raghupathi et al. Heal Inf Sci Syst. 2014;2:3. 2. Yang et al. JAMA Netw open. 2019;2(4):e192696. 3. Chan et al. Diabetes Care. September 2019:dci190003. 4. Makino et al. Sci Rep. 2019;9(1):11862. 5. So et al. Am J Manag Care. 2003;9(9):606-615. 6. Ko et al. BMC Med Inform Decis Mak. 2010;10(1):26. 7. Yeung et al. Lancet Diabetes Endocrinol. 2014;2(12):935-943. 8. Tutino et al. Diabet Med. 2017;34(3):440-450.





