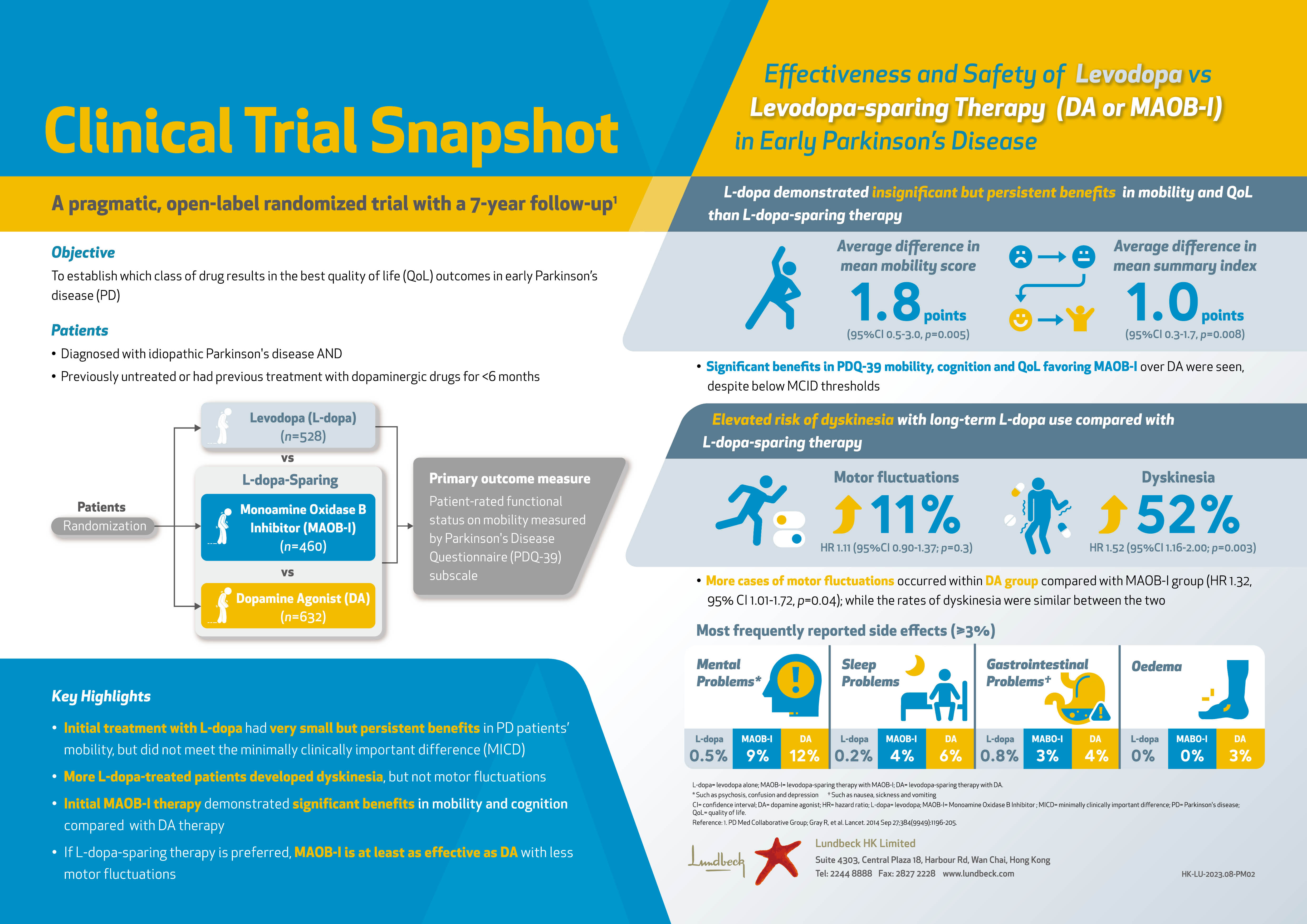
The Potential Risk of Intervertebral Disc Degeneration upon Microgravity Exposure
Low back pain (LBP) is one of the disorders with highest health burden globally. The disorder causes limitations in activity and work capacity leading to considerable economic and medical costs to individuals and their families, as well as governments. Although LBP is non-fatal, it significantly impacts the years lived with disability (YLD). The estimated prevalence of LBP in China was 4.2% in 2016, associated with an YLD of 7.7 million1. Of note, intervertebral disc (IVD) degeneration is reported to be a main cause of LBP that 40% of individuals with LBP suffer from the condition2. Moreover, exposure to microgravity has been reported to increase the risk of cervical and lumbar IVD herniations3. The current article highlights the potential risks of exposure to microgravity on development of IVD degeneration and strategies for countering the disease.
The IVD and Its Degeneration
The IVD is a non-vascular structure composed of 3 anatomical tissues including inner nucleus pulposus (NP), outer annulus fibrosus (AF) and cartilage endplate. The structure of AF is formed by type I and II collagen fibres and elastin fibres arranged in concentric circles, which can withstand the tension produced by the vertebral motion to maintain the position of NP. The NP tissue is constituted by extracellular matrix (ECM) including type II collagen and aggrecan synthesised by NP cells4. Degenerative disc disease (DDD) is a pathologic condition of IVD that has been associated with chronic back pain which typically occurs with age and is most common in the lower lumbar spine. Of note, there are various factors related to DDD such as impaired metabolite transport, cell senescence and death as well as changes in matrix macromolecules and water content5. In addition to pain, DDD is often accompanied with up-regulation of pro-inflammatory cytokines, whereas herniation is a common disc disorder of disc extrusion starting from disc bulging (Figure 1)6.

Figure 1. Structure of a healthy and degenerative human6
Microgravity and IVD Herniation
In addition to the factors stated above, former study on spine health of astronauts after prolonged spaceflight reported a significant decrease in lumbar lordosis and active lumbar flexion-extension range of motion7, which are associated with impaired spine biomechanics and chronic LBP. According to a previous report from the National Aeronautics and Space Administration (NASA), 10% of all astronauts in the United States were diagnosed with IVD herniation after spaceflight compared to 3.5% in the control, Earth-bound, population. The report further highlighted that the incidence was highest immediately upon returning to Earth. Particularly, astronauts with significant pre-flight endplate irregularities reported post-flight chronic LBP and/or disc herniation7, while the most likely cause for lumbar IVD herniation in astronauts would be the swelling of the IVD in the unloaded condition during spaceflight3.
Bone loss in vertebral body during spaceflight would likely influence the IVD. Clinically, people with lower bone mineral density have been reported to have larger IVDs8(Figure 2). Importantly, the reduced bone strength would allow deformation of the vertebral endplate and expansion of the IVDs, whereas a significant proportion of herniation cases occurs as a result of failure at the endplate junction9.

Figure 2. Larger IVD in people with osteoporosis (right) compared to normal control (left)3
Prolonged Bed Rest and LBP
The most commonly used ground-based analog of microgravity is long-duration, head-down tilt bed rest (HDTBR). Long-term bed rest removes physiological diurnal loads from the lumbar spine, which can hypothetically disrupt lumbar stabilisation by deconditioning both the passive, active, and neural stabilising systems7. A 60-day HDTBR has been shown to reduce glycosaminoglycans (GAG) concentration in lumbar IVD10. Additionally, the treatment would significantly increase in disc volume and spinal length with greatest increase at lower lumbar spine, and reduce lower lumbar lordosis. Further, significant atrophies in the cross-sectional areas of the multifidus (MF), erector spinae and quadratus lumborum were observed upon prolonged bed rest11. These changes in lumbar IVD and selective atrophy of the MF muscle highlight the increased risk of LBP upon prolonged bed rest. Particularly, the risk for elderly and bed-bound patients would be a clinical concern.
Countermeasures of IVD Degeneration
Clinical therapies for LBP, such as removing NP tissue surgically, are mainly focused on relieving symptoms rather than restoration4. There are many preclinical and clinical studies investigating the efficacies of mesenchymal stem cell (MSC) transplantation in attenuating IVD degeneration. Nonetheless, the results were inconsistent. For instance, a systematic review by Meisel et al (2019) on the use of cell therapy for IVD repair revealed that the overall strength of evidence for efficacy and safety of cell therapy for lumbar IVD repair was very low because of the substantial risk of bias, small sample sizes and lack of a comparator intervention12. On the contrary, another systematic review on the outcomes of autologous MSC injections for the regeneration of IVD suggested that, in patients underwent conservative therapies prior to injection, remarkable improvement in quality of life were reported at 1-year follow-up13. Although positive findings exist, there are still many obstacles in treating IVD degeneration with cell therapy including survival and differentiation of transplanted MSC under the harsh environment in the degenerated IVD.
Besides cell therapy, tissue engineering based on cell and scaffolds have been researched extensively with positive outcomes for IVD regeneration. For instance, chitosan has been approved by the Food and Drug Administration (FDA) as a compatible biomaterial because of its non-cytotoxicity, biocompatibility, biodegradability and antibacterial characteristic6. However, scaffolds made of natural polymers alone are generally insufficient as a tissue-engineered IVD scaffold. Thus, most studies have fabricated scaffolds by physically or chemically combining a plurality of natural or synthetic polymers. Nonetheless, further clinical trial data on efficacies of functional polymers for IVD regeneration are highly desirable. In summary, there is a wide spectrum of strategies for countering IVD degeneration. Yet, in addition to focus on each of the strategic fields, the fusion of various strategies such as combining cell therapy and tissue engineering would possibly generate promising outcomes in countering IVD degeneration.
References
1. Wu et al. Pain. 2019;160(1):237-245. 2. Liang et al. Medicine (Baltimore). 2017;96(25). 3. Belavy et al. Eur Spine J. 2016;25(1):144-154. 4. Liu et al. World J Stem Cells. 2020;12(4):266-276. 5. Adams et al. Spine (Phila Pa 1976). 2006;31(18):2151-2161. 6. Choi et al. Polymers (Basel). 2019;11(5):872. 7. Bailey et al. Spine J. 2018;18(1):7-14. 8. Kwok et al. Spine (Phila Pa 1976). 2012;37(23). 9. Rajasekaran et al. Spine (Phila Pa 1976). 2013;38(17):1491-1500. 10. Kordi et al. J Musculoskelet Neuronal Interact. 2015;15(3):294-300. 11. Belavý et al. Spine (Phila Pa 1976). 2011;36(2):137-145. 12. Meisel et al. Glob Spine J. 2019;9(1_suppl):39S-52S. 13. Migliorini et al. Int Orthop. 2019;43(4):1027-1036.