

Specialist in Psychiatry
Tackling the Unmet Need for the Treatment of Depression
Mental disorders are common in Hong Kong that the prevalence among Chinese adults aged between 16 and 75 is 13.3%, whereas depression is one of the most common disorders with a prevalence of 2.9%1. Although the health burden of depression and other mental disorders is substantial, the utilisation of local mental health services remains suboptimal that only 26% patients with common mental disorders had consulted mental health services, while less than 10% consulted general practitioners or family physicians1. In order to uncover the unmet need of depression treatment and strategies for optimising treatment outcomes, Dr. King Yee Chong, specialist in psychiatry, shared her insights and clinical opinions on managing depression.
Enhancing the Awareness on Depression
“The reported data cannot reflect the actual burden.”
Dr. Chong commented on the reported local prevalence of depression. “Some respondents may not be aware of the disorders they suffered from,” she explained. Hence, this suggests that the actual burden of mental disorders is likely underestimated in reported data. In response to the inquiry on high-risk populations for depression, Dr. Chong outlined that females, suffering from serious illnesses and certain personal history such as being widowed, personal traumas as well as experiencing social unrest and wars are risk factors for depression. Additionally, she stated that elderly people with chronic diseases and certain personality behaviours such as perfectionism are at increased risk for depression as well.
Practically, general practitioners are the first healthcare professionals reached out to by patients. Nonetheless, only a small proportion of patients would consult general practitioners for depression. Dr. Chong suggested this is partly due to the patients’ perception of the presence of depression. For instance, some patients believe that they have no depressive problem but are simply upset by other people or incidents. Besides, general practitioners may not be aware on the influence of depression among the wide spectrum of potential diseases during diagnosis. Thus, Dr. Chong emphasised the importance of professional education in enhancing awareness on depression. “Diploma program on mental health is beneficial for physicians. In particular, clinical case sharing, continuous medical education (CME) and symposia are essential for enriching knowledge on psychiatry and hence increasing the awareness on mental disorders for general practitioners,” she addressed.
The Underlying Reasons for Non-adherence
As reported, only a limited proportion of patients with depression receive appropriate psychiatric treatments. Aside from the awareness on depression, treatment discontinuation and/or non-adherence also contributes to the low treatment rate in patients with depression. Dr. Chong stated that patients’ perceived need for care is a common reason for refusing treatment. “Some patients realise their depressive symptoms, but attempt other ways to relieve the symptoms such as talking with friends,” she said. Besides, some patients on medications discontinue treatment due to intolerance. On the other hand, common side effects of antidepressants include weight gain, sexual dysfunction and somnia, which are common reasons contributing to poor adherence.
Medication Matters
As medications facilitate the brain to manage moods, they are also a core part in managing depression. Clinically, selective serotonin reuptake inhibitors (SSRIs) are common options for the treatment of depression along with psychotherapeutic interventions, but many patients either do not respond or are intolerant to the undesired effects of the medications. Former studies indicated that remission rates following 2 trials of an SSRI are less than 50%2.
Selective serotonin-norepinephrine reuptake inhibitors (SNRIs), such as desvenlafaxine, act selectively on the serotonin and norepinephrine transporters. The medication also affects the hypothalamus which is an important regulator of biological functions such as mood, sleep cycle, stress response, sexual behaviours, temperature, and pain sensations. Essentially, desvenlafaxine lacks significant affinity for numerous receptors, including muscarinic cholinergic receptors, and thus possibly reducing the risk of adverse effects related to these receptor sites2. Hence, international consensus advocates SNRIs as a first-line treatment option for pharmacological management of depression3.
Dr. Chong addressed that desvenlafaxine is safe with low risk of drug-drug interactions (DDIs) in general. She stated that heart beating and constipation are reported in some patients with anxiety, whereas the symptoms are probably triggered by anxiety but unlikely the side effect of desvenlafaxine. Moreover, the symptoms are mostly mild and self-limiting. Besides, Dr. Chong agreed that desvenlafaxine is beneficial for patients with pain. Of note, previous multi-center, Phase III randomised control trial involving 474 patients with major depressive disorder demonstrated that desvenlafaxine (100 mg/day) significantly reduced overall pain (p=0.041), back pain (p=0.031) and arm, leg, joint pain (p=0.006), reflected by Visual Analog Scale-Pain Intensity (VAS-PI), as compared to placebo4. On the other hand, Dr. Chong noted that, as an SNRI, desvenlafaxine would unlikely induce hypersomnia. Hence, Dr. Chong’s opinions complied with the findings in former studies and confirmed the safety profile of desvenlafaxine5-7.
Clinically, a substantial proportion of patients with depression suffers from comorbidities (Figure 1), especially elderly patients, and is already on other medications. Hence, the risk of DDIs is a major concern in prescribing antidepressants. Optimal treatment outcomes are expected through drug selection with minimal potential for DDIs. “If DDI is not a concern, physicians could predict better the treatment progress. Otherwise, physicians would need to titrate the dosage and likely delay the onset of treatment effect,” noted Dr. Chong.
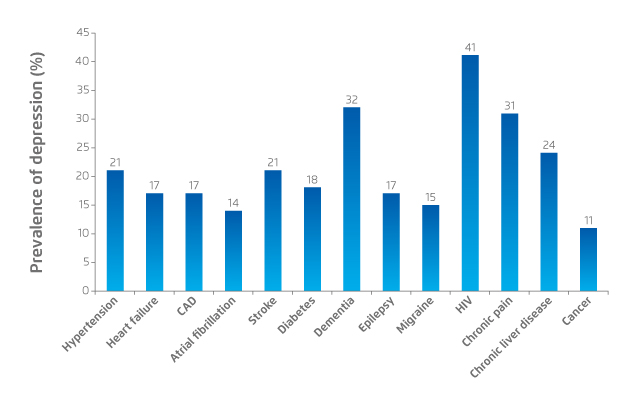
Figure 1. Prevalence of depression in patients with chronic physical conditions8. CAD: coronary artery disease
Essentially, Low et al (2018) suggested that desvenlafaxine exhibits a simple metabolic profile, unique among antidepressants, making it favourable in avoiding cytochrome P450-related pharmacokinetic interactions with drugs of many therapeutic classes. Nonetheless, relevant pharmacodynamic interactions with desvenlafaxine, such as elevated blood pressure and heart rate, should be closely monitored in practice8. “As DDIs are preventable in most cases, why don’t we select one with a lower risk of DDI?” wondered Dr. Chong.
Interaction - The Key for Optimising Treatment Outcomes
The American Psychological Association (APA) guideline advocates that interventions for depression should be aimed at maximising the patient’s level of functioning, such as at work and school, social relationships, and helping patients to set goals according to their functional impairments and symptom severity9. Dr. Chong shared the case of a depressed wife. The relationship between the patient and her husband had been worsened by depressive symptoms, and an antidepressant was prescribed for the patient,” described Dr. Chong, “We need to educate the patients the appropriate way to evaluate the treatment effects. In the case of the depressed wife, I asked the patient to evaluate the improvement based on the number of incidents in which her husband had upset her. The reduced occurrence of marital conflict was in fact the improvement in mood due to anti-depressant”.
Dr. Chong emphasised that close and timely monitoring of therapeutic effects is crucial. She agreed that the improvements for desvenlafaxine can normally be observed within the first 2 weeks since the therapeutic dosage can easily be achieved without titration. In the case sharing, medication effectively improved the depressive symptoms for the patient as reflected by better sleeping quality and an improved relationship between the patient and her husband. Nonetheless, the close interaction between physicians and patients is the key for acquiring comprehensive understanding on the patients’ physical and mental condition as well as underlying difficulties experienced during treatment.
Overcoming Depression
Dr. Chong devoted herself to bringing a healthy life for her patients, such as helping resume work for patients whose career life has been affected by depression. She suggested that physicians are required to understand the needs of their patients. Importantly, she advised that certain tools for diagnosis including patient-reported questionnaires are useful. However, they may not always reflect the actual mental status of patients and using it as a routine procedure is not recommended. Similarly, guidelines are a useful reference in certain cases, especially for general practitioners, providing them the direction for treatment. However, deciding the appropriate treatment protocol relies on the expertise of physicians. Thus, Dr. Chong summarised that the communication between physicians and patients is essential in depression management. With proper communication and effective therapeutics, optimised control of depression is expected. “Witnessing the improvement in patients is a rewarding experience for physicians,” concluded Dr. Chong.
References
1. Lam et al. Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1379-1388. 2. Faquih et al. Cureus. March 2019. 3. Sakurai et al. J Affect Disord. 2020;266:626-632. 4. Liebowitz et al. Curr Med Res Opin. 2008;24(7):1877-1890. 5. Atkinson et al. J Child Adolesc Psychopharmacol. 2018;28(1):55-65. 6. Tourian et al. Prim Care Companion CNS Disord. 2011;13(2). 7. Ferguson et al. CNS Spectr. 2012;17(3):121-130. 8. Low et al. Neuropsychiatr Dis Treat. 2018;14:567-580. 9. Gelenberg et al. Am Psychol Assoc. 2010.





