
A Unique View on Infertility Pandemic
Infertility is defined as the failure to achieve pregnancy after 12 months of regular unprotected sexual intercourse and currently affects around 8.8% of females aged between 15 and 49 in the United States (US)1. Locally, infertility affects one in six couples and health care professionals (HCPs) often attribute infertility as a medical problem with psychological consequences rather than a sociocultural issue2. Moreover, the individual and societal burden of infertility is high since the prevalence of infertility in females affects all countries regardless of their socio-demographic index (SDI)3. Of note, approximately 85% of infertility couples have an identifiable cause with aetiology often related to ovulatory dysfunction, male factor infertility, and tubal disease1. The remaining 15% of infertile couples often are considered to have “an unexplained infertility aetiology.” As such, lifestyle, and environmental factors, such as smoking and obesity, are often considered an attributable factor which adversely leads to infertility.
Interestingly, ovulatory disorders account for approximately 25% of infertility diagnoses and 70% of females with anovulation have polycystic ovary syndrome (POS)1. Other factors, such as the age of birth of the first child, are recognised as major risk factors for infertility and continue to rise because of longer education, difficulties in accessing stable employment, and the fragility of marital and non-marital unions3. Hence, infertility may lead to tremendous societal repercussions other than personal suffering. Social effects related to infertility can have a profound effect on a female’s emotional well-being since infertility often affects social relations, economic, and inadvertently their marriage2. To understand the complexity of infertility, we shall first indulge ourselves in the cause of infertility, followed by understanding the current treatment advanced related to infertility and the persistent unmet needs.
Infertility: Inherited or Acquired?
Due to a wide range of reasons, the prevalence of infertility is on rise globally4. Low and ultra-low fertility, that is, a total fertility rate (TFR) at or below the replacement level of 2.1 live births per woman, is an increasing global trend in 83 of 201 countries5. It is assumed that by the year 2050, the average global fertility rate is predicted to decline to 2.1. In some countries in Asia and Europe, ultra-low fertility rate is becoming more prevalent5. Interestingly, studies have shown that individuals have fewer children than they wanted, particularly in the Asia-Pacific region (APR), due to broader socioeconomic changes in education and labour force participation5. So, what are the issues related to low fertility? Well, low fertility may lead to shrinkage of the workforce, reduced productivity, lower ethnic diversities, and cause a national decline5.
Furthermore, since females often spend longer time in formal education, and their career trajectories demand long working hours, inflexible work situations, and limited support during and after pregnancy (such as lack of parental leave and childcare), many females may choose to postpone or not marry and delay childbearing. In many East Asian contexts, there is also an expectation of long and inflexible working hours in person required for promotion, benefits, and seniority5. Emerging studies have found on average, females often devote more time to unpaid care and domestic work. For instance, females often spend 314 minutes compared to the 190 minutes per day spent by males on unpaid care and domestic work5.
But is infertility the same as sterility? The answer to this is no since infertility relies on a restricted period, whereas sterility is a permanent state of infertility6. It is important to note that infertility is not only found in females. Instead, males account for 20-30% of infertility cases and contribute to 50% of cases overall, according to epidemiologic data6. Factors that may lead to infertility include disease and non-disease related. Disease-related infertility may affect both genders or be specific to one gender, as illustrated in Figure 16.
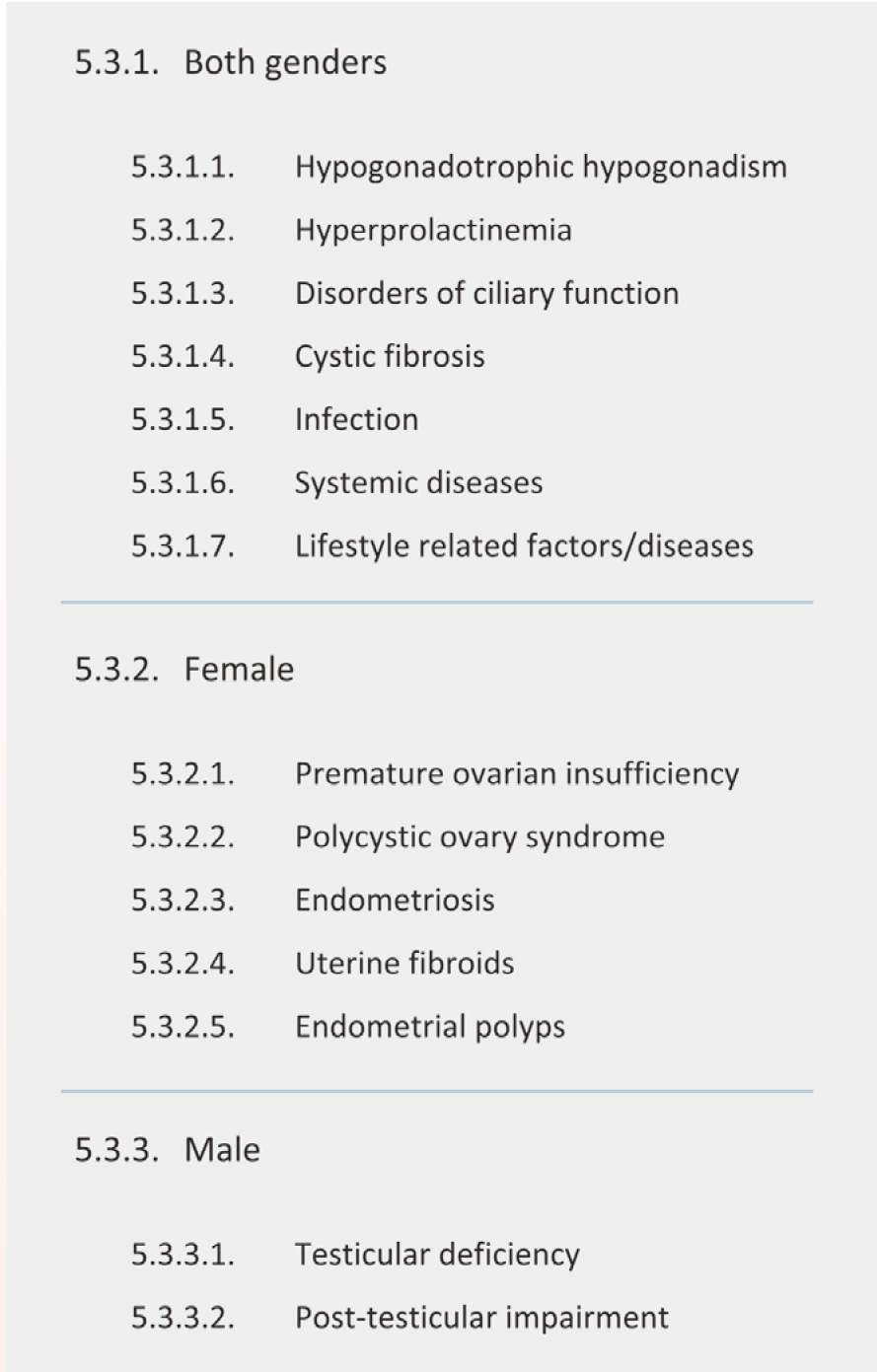
Figure 1. Disease-related infertility6.
Non-disease-related factors include consanguineous marriage, which is defined as marriage between a male and female who are related as second cousins or closer6. In fact, more than half of the world’s population lives in areas where consanguineous marriage is widespread. The association between reproductive outcome and the degree of a partner’s consanguinity has been the focus of an observational study that showed parental consanguinity is associated with female infertility and prematurely reduced ovarian reserve. Surprisingly, these inherited fertility issues are not prevalent in male offspring, regardless of the consanguinity. Other problems with consanguineous marriages include increased incidence of inherited recessive disorders that affect reproductive and health parameters6.
Suffering from Infertility? Why Keep Silent?
Females desiring pregnancy who have not conceived after 12 months of unprotected intercourse or donor insemination should be offered an infertility evaluation. Moreover, earlier evaluation is recommended in females over than the age of 35 who have not conceived for 6 months, and more immediate evaluation is warranted in females older than 40 years. Fertility evaluation is also recommended in females with oligomenorrhea or amenorrhea, known or suspected uterine, tubal, or peritoneal disease (including stage III or IV endometriosis), and male partners with known or suspected male factor infertility (Figure 2).
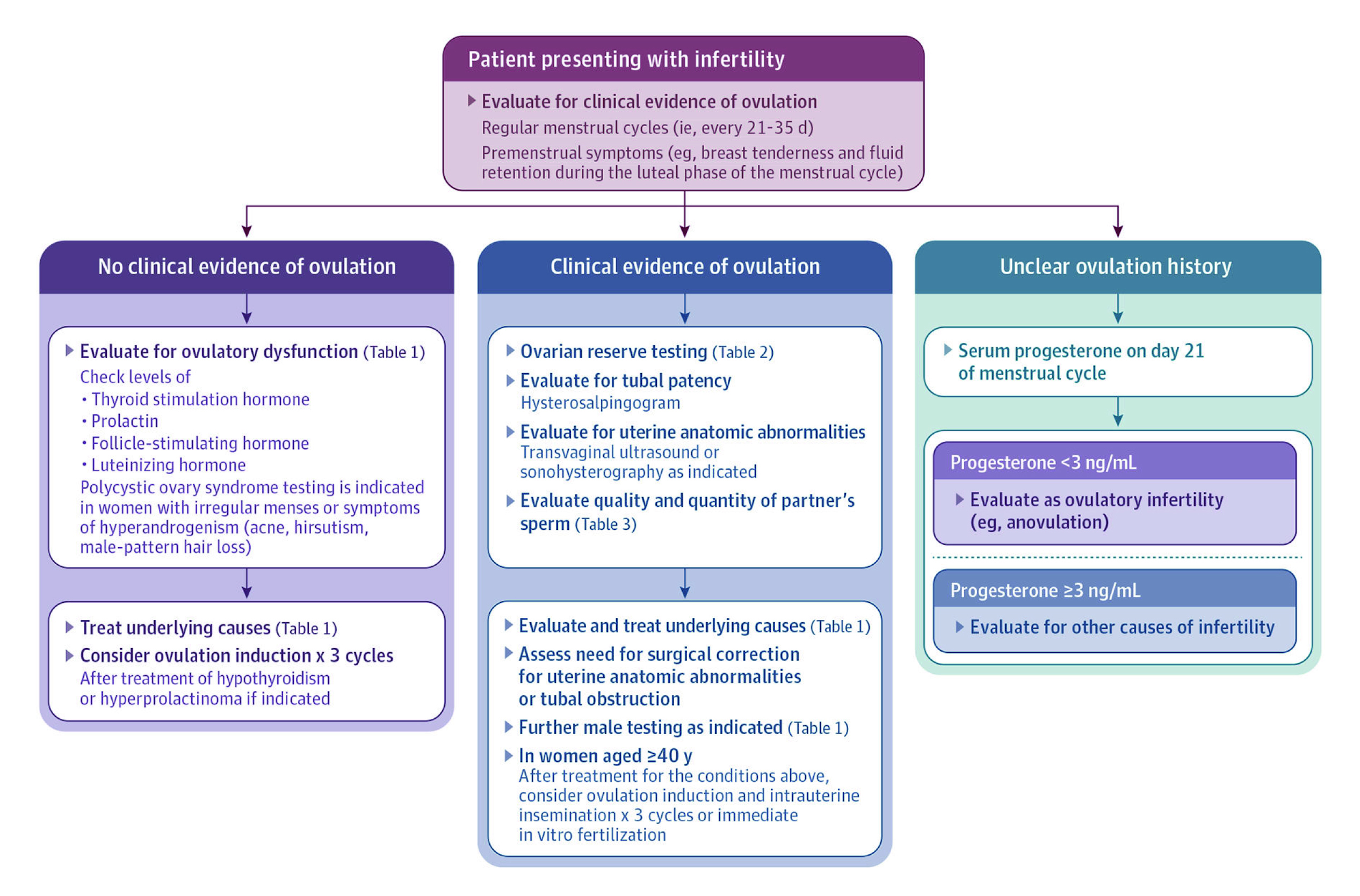
Figure 2. Suggested evaluation for patients presenting with infertility1.
But what are the treatment options available for those who suffer from infertility? Commonly infertility treatments include ovulation induction, which refers to the use of pharmacologic treatment to induce ovulation, and ovarian stimulation, which is performed to induce multiple mature ovarian follicles1. Either timed intercourse or intrauterine insemination (IUI) may be used to achieve fertilisation at the time of ovulation. Alternatively, mature oocytes may be retrieved directly from the ovary for fertilisation using an ultrasound-guided needle in a technique known as in-vitro fertilisation (IVF)1. Before infertile couples decide to undergo IVF cycles, they are often required to consider the success rate, cost, and service quality of these procedures.
IVF, what does it do and how successful is the procedure? IVF is a highly individualised, patient-centred treatment approach4, and two oral medications are typically used for ovulation induction. Clomiphene citrate is a selective oestrogen receptor modifier that blocks the negative feedback effect of circulating oestradiol and causes an increased hypothalamic gonadotropin-releasing hormone (GnRH) pulse frequency and subsequent pituitary FSH and luteinising hormone (LH) production, promoting ovarian follicular growth1. The other agent is letrozole, which blocks the aromatase, reducing the serum concentrations of oestradiol and stimulating pituitary gonadotropins. Both clomiphene and letrozole have a multiple pregnancy rate of less than 10%1. Furthermore, for females with PCOS undergoing ovulation induction, letrozole is the first-line therapy based on the pregnancy in the Polycystic Ovary II Trial, which demonstrated that letrozole results in higher live birth rates compared with clomiphene1.
However, females with hypogonadotropic hypogonadism may exhibit limited or no endogenous pituitary gonadotropin response. In these patients, pulsatile GnRH administration restores the physiological stimulation of endogenous FSH and LH to induce follicular maturation and ovulation. Treatment with pulsatile GnRH results in a pregnancy rate of 93% to 100% after up to 6 months. However, these treatments have their limitations, as multiple pregnancies have been reported in 36% of cases, and ovarian hyperstimulation syndrome is seen in 1-5% of cycles, which can cause ascites, electrolyte imbalance, and hypercoagulability with gonadotropin use1. Hence, IUI and IVF are options with IUI often performed by placing sperm into the uterus 24 to 36 hours after an endogenous LH surge or an exogenous ovulation, while IVF involves utilisation of gonadotropin stimulation, followed by aspiration of multiple ovarian follicles which are fertilised in vitro1. However, despite the availability of these treatment options, the unmet treatment needs persist due to the cost, inability to access infertility treatment, geographic disparities, and psychosocial reasons7. A very recent study performed by Minguez-Alarcon et al. (2024) highlighted how stress was positively associated with impaired glucose among females following fertility treatment, particularly the IUI8. Therefore, healthcare providers should empathise with patients on the impact of infertility and provide both informational as well as emotional support to promote mental health and treatment options.
References
1. Carson SA, Kallen AN. Jama 2021; 326(1): 65-76. 2. Tiu MM et al. Int J Qual Stud Health Well-being 2018; 13(1): 1554023. 3. Bourrion B et al. BMC Health Serv Res 2022; 22(1): 512. 4. Pan L-F et al. Taiwanese Journal of Obstetrics and Gynecology 2019; 58(5): 633-9. 5. Boydell V et al. Glob Health Med 2023; 5(5): 271-7. 6. Vander Borght M et al. Clinical Biochemistry 2018; 62: 2-10. 7. Öztürk R et al. J Community Psychol 2021; 49(5): 1121-33. 8. Mínguez-Alarcón L et al. Journal of the Endocrine Society 2024; 8(1).





