
Since the COVID-19 pandemic, various virtual technologies have become available to allow alternative ways to deliver medical education and training. Clinical anatomy is a critical component of medical education and often requires cadaver dissection, which can be expensive, time-consuming for maintenance and storage purposes 1. To overcome these shortfalls, new virtual immersive technologies such as virtual reality (VR) and augmented reality (AR) have been integrated into medical education since it allows the projection of virtual environments which are user-friendly, thereby aiming to deliver content effectively. So, what is AR and VR? AR is a real-world-based, mixed reality enhanced by digital objects or information. It is usually achieved through a headset or tablet-style device such as a smartphone, through which digital objects are created and surrounded by the actual environment 2.
On the other hand, VR produces virtual images of the real world by utilising three-dimensional (3D) images or environments that can be interacted in a seemingly real or physical way 3. Mixed reality (MR), also known as merged reality, is a new concept, considered a combination of VR and AR or a subtype of AR with new digital holographic image technology 4. MR has become increasingly popular and is slowly gaining user interest, particularly in medical education, since it allows users to manipulate and interact with objects in real-time as part of the real world 5.
What are the benefits of using MR? Currently, MR devices such as HoloLens 2 is a head-mount device that combines several types of sensors aimed to provide a “head-up display” with the ability to place virtual hologram objects within the visual field of users. In addition, it allows live bidirectional communication through video and voice between multiple remote users. In the clinical setting, MR enables multiple users to be connected and interact from remote locations. For instance, patient interactions can be observed remotely by clinicians, with blood and radiological reports viewed as holograms 6. The efficacy of MR devices has been demonstrated in a pilot study where the MR device was used to deliver remote care in a Coronavirus disease 2019 (COVID-19) hospital, as illustrated in Figure 1. The study concluded deployment of MR devices led to a 51.5% reduction in time exposed to COVID-19 for staff, in addition to achieving a staggering 89.3% clinical team satisfaction 7.

Figure 1. Mixed reality (MR) device helps create a first-person view allowing the clinical team to remotely interact with the patient, in addition to reducing their risk of COVID-19 exposure 7.
Despite the increasing interest in MR use in medical education, robust evidence is inadequate to justify its mainstream use in teaching. For instance, anatomical knowledge had traditionally been taught through the cadaveric dissection in both medical education and training. As the amount of health sciences content required of medical students increased overtime, with less curricular time available for anatomy, more efficiently and effective teaching modalities are required. Therefore, the introduction of MR may not solve all the problem but remains a viable option since it allows the delivery of virtual anatomy, which augments the 3D images, and help learners grasp complex concepts. You may then ask if students taught using MR technology performs as well as those taught traditionally and are there merit to such claims. Well, there is a randomised controlled trial (RCT) that compared the effectiveness of MR with that of traditional cadaveric dissection in teaching musculoskeletal anatomy. The study found no significant statistical differences between the two during the anatomy exams, suggesting MR can achieve similar performance to traditional cadaver dissection 8.
MR provide learners with an accurate 3D perception of human anatomy and allows them to manipulate virtual objects, improving their learning experiences 9,10. Furthermore, MR also helps learners develop clinical judgment and skills through patient interactions during clinical teaching 11. The benefits of MR are not isolated to medical education. Instead, it has also been implemented in endoscopic surgical teaching, which often requires meticulous motor skills. In fact, novice surgical trainees who used MR had noticed an improvement in procedural time, in addition to a boost in performances, thereby further demonstrating the capabilities of MR use in surgical training 12. Moreover, MR also helped reduce mental, physical, and level of frustration among surgical trainees, as illustrated in Figure 2. Some have even suggested MR use in Objective Structured Clinical Examinations (OSCEs) as experimental studies have shown OSCE examination results obtained are comparable between the MR and the traditional in-person OSCE within the undergraduate curriculum 13.
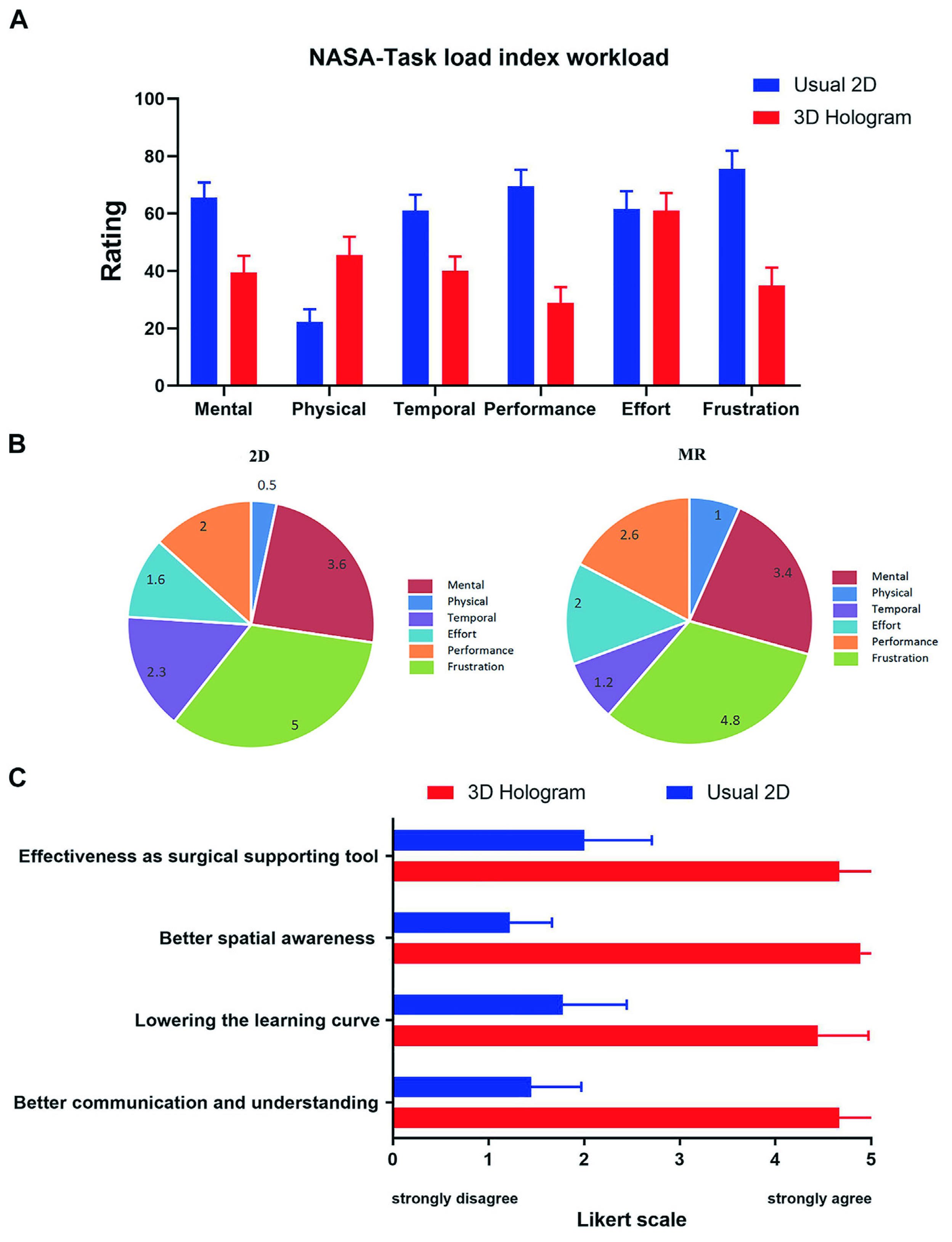
Figure 2. The National Aeronautics and Space Administration-Task Load Index (NASA-TLX) and Likert-scale Questionnaire Scores showed how surgeons experiencing a higher physical demand with MR due to the weight of the headset but lower levels of frustration during surgery compared to usual 2D (non-MR) 14.
The efficacy of MR technology is not limited to medical education. Instead, it can also be used in clinical practice, particularly for the delivery of clinical treatment. For instance, out-of-plane lesions are often difficult to treat since they pose a significant challenge to the delivery of CT-guided interventions. A recent study assessed the use of MR in targeting difficult-to-access lesions concluded that MR utilisation not only helped reduce the time of the procedure from 8.93 minutes to 4.42 minutes, instead it also decreased the puncture rate of non-targeted lesions from 11.9% to 0%.In addition, it also improved the precision of the ideal target trajectory 15. But are there any limitations to the MR? Yes, there is, and eye strain is one of the reasons which prevents MR mainstream use. Prolonged use of MR head-mounts has shown to decrease the blink rate, which may predispose users to eye strain or dry-eye syndrome 16.
Some users have also experienced unwanted side effects, also known as “cybersickness,” that is related to motion sickness during the MR sessions; hence, limiting their applicability 17.
Cybersickness is believed to be caused by the disparity between the physical surface of the screen (accommodation) and the focal point of the virtual simulated world the user gazes at (vergence) 18. In addition, MR equipment is expensive and incompatible with standard appliances considering MR is still in the early developmental stages. Despite these limitations, some see MR as a valuable clinical partner due to its unique properties and multimodal use in different clinical specialties. For instance, arachnophobia, the fear of spiders, has been successfully treated using MR 19. In conclusion, MR technology offers a promising experience to users in both clinical and non-clinical settings. Therefore, further long-term studies are warranted to assess its safety in clinical practice.
References
1. Kolecki R, et al., Translational Research in Anatomy 2022; 28: 100214. 2. Dhar P, et al., Med Educ Online 2021; 26(1): 1953953. 3. Haowen J, et al., BMJ Open 2021; 11(5): e046986. 4. Hu HZ, et al., Curr Med Sci 2019; 39(1): 1-6. 5. Sivananthan A, et al., JMIR Form Res 2022; 6(5): e35674. 6. Kamphuis C, et al., Perspect Med Educ 2014; 3(4): 300-11. 7. Martin G, et al., J Med Internet Res 2020; 22(8): e21486. 8. Stojanovska M, et al., Med Sci Educ 2020; 30(1): 173-8. 9. Kumar N, et al., Aesthetic Plast Surg 2021; 45(3): 1005-11. 10. Maniam P, et al., J Vis Commun Med 2020; 43(1): 17-26. 11. Frost J, et al., BMJ Simul Technol Enhanc Learn 2020; 6(4): 214-9. 12. Al Janabi HF, et al., Surg Endosc 2020; 34(3): 1143-9. 13. Minty I, et al., BMC Med Educ 2022; 22(1): 639. 14. Lu L, et al., Frontiers in Bioengineering and Biotechnology 2022; 10. 15. Park BJ, et al., Scientific Reports 2020; 10(1): 18620. 16. Marklin RW, et al., Hum Factors 2022; 64(2): 305-23. 17. Mazloumi Gavgani A, et al., J Appl Physiol (1985) 2018. 18. Mazloumi Gavgani A, et al., PLoS One 2017; 12(8): e0182790. 19. Bouchard S, et al., Technol Health Care 2006; 14(1): 19-27.





