
Doctor at National Health Service (NHS),
United Kingdom (U.K.)
Migraine as we know is a recurrent neurological disorder that is often under-recognised as it is one of the leading causes of disability around the world in individuals below the age of 50. The prevalence of migraine is around 15%, globally, and symptoms of migraine can be debilitating1. Apart from the health impact, migraine also causes tremendous economic losses with an estimated $11-12 billion US dollars (USD) loss reported in 2007. Interestingly, sufferers of migraine often report of gastrointestinal (GI) symptoms such as nausea, vomiting, dyspepsia, diarrhoea, and constipation. More recently, it is believed that migraine may induce the inflammatory bowel disease (IBD) by interfering with the gut-brain axis1. Therefore, to understand this unusual relationship between migraine and IBD, we have invited the Dr. Dwebi, one of the doctors at the NHS, U.K. to share his experience on this phenomenon.
Migraine is a recurrent, chronic disorder that is prevalent in females, and is the 1st cause of disability in those under the age of 502. It is characterised by recurrent disabling attacks of unilateral headaches with nausea, and increased sensitivity to light and sound. Interestingly, migraines are classified according to the Headache Classification Committee of the International Headache Society (IHS) as migraine with or migraine without aura (75% of cases)3. The precise aetiology of migraine remains elusive, but is believed to have a strong genetic component with three times greater risk seen in those with family history of migraine3. Dr. Dwebi added that migraine is highly prevalent, affecting 12% of the population and is ranked as the 2nd leading cause of disability, globally3. More interestingly, migraine has been associated with sleep disturbances since studies have shown a correlation between the sleep quality and migraine frequency4.
Despite the availability of international guidelines for migraine diagnosis and treatment, the management of migraine remains the unmet need due to the delay in diagnosis and some patients receiving improper treatment during the acute flare-ups. Dr. Dwebi explained that the reason behind these may be due to the lack of public awareness, lack of physician knowledge on the condition and management. In addition, he added that there are 80% of patients that are seen in the primary care for migraine, remarkably, less than 20% are correctly diagnosed and treated5. More importantly, according to the World Health Organisation (WHO), in 50% of headache, patients often administer self-treatment and only 10% are actually seen by the neurologist. What does this mean? Well, most of these patients will then go on and rely on analgesics, resulting in medication overuse headaches, which leads to a vicious cycle, Dr. Dwebi suggested5. Therefore, it is important to provide patient education on migraine, in addition to refer those to specialist who experience an inadequate response or are intolerant to standard treatment.
Migraine headaches are often debilitating, and patients often report experiencing gastrointestinal (GI) symptoms such as nausea, vomiting, dyspepsia, diarrhoea, and constipation. Recently studies have also demonstrated a higher prevalence of migraine reported in patients with IBD; nonetheless, the precise aetiology remains elusive. When asked, Dr. Dwebi explained that IBD is a chronic relapsing inflammatory GI disorder that consists of Crohn’s disease (CD) and ulcerative colitis (UC)1. He added that there is an interplay between migraine and IBD through the gut-brain axis. Furthermore, IBD shares some epidemiological characteristics to those of migraine since it is more likely to be diagnosed in children, or young adults and often co-exists with other chronic conditions such as depression, anxiety, asthma, and other neurological disorders6. Notably, recent studies have demonstrated the odds of migraine in IBD patients is approximately 2.6 fold2 and these findings have been corroborated by Pascual-Mato et al., (2024) who evaluated interviews of 283 patients aged between 18-65 years. Astonishingly, 62.2% of patients had headaches with 20.8% meeting the migraine criteria, and female prevalence being higher than that of males. The authors concluded that migraine prevalence, including chronic migraines, is increased in patients with IBD, particularly in female suggestive of a gender-bias of the disease6. But why is there a gender discrepancy? Dr. Dwebi highlighted that the sex disparity in migraine is believed to be partly mediated through the fluctuations in ovarian steroid hormones, especially the oestrogen and progesterone, but the precise cause remains to be explored7.
Since we now know that migraine is more prevalent in IBD patients, is it possible for migraine to cause IBD? Dr. Dwebi suggested that the gut-brain-axis plays a crucial role in development of several diseases, and migraine is no exception. He shared the data from a nationwide population-based cohort study by Lee et al., (2024) that evaluated the relationship between migraine and IBD. A total of 10,628,070 Korean patients aged 20 years or old who had undergone a national health examination conducted by the Korean National Health Insurance Service (NHIS) in 2009 were followed until 2017. The study population was divided into 2 group according to the presence or absence of migraine. Disturbingly, the incidence of newly diagnosed IBD was significantly higher in patients with migraine (adjusted hazard ratio [aHR] with 95% confidence interval [CI] was 1.31 [1.173-1.468], p<0.001) than those without migraine1. After 5-year follow-up, those with migraine showed curves implying cumulative incidences of IBD with a steep increase, especially for CD. Remarkably, the subgroup analysis showed migraine was associated with the risk of UC in males (aHR= 1.431 vs 1.117; interaction p=0.042) (Figure 1). The conclusion drawn from the study was that migraine is significantly associated with the development of IBD, and patients with migraine should be carefully monitored for the development of IBD1.
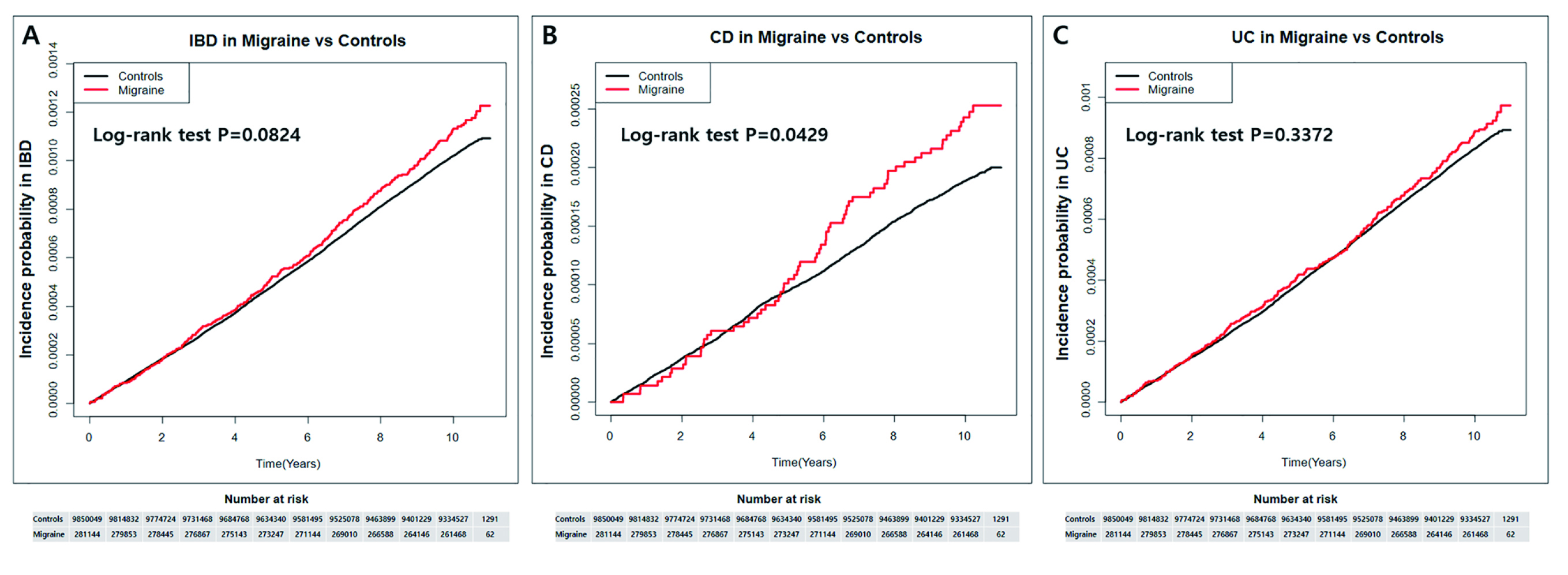
Figure 1. Cumulative incidence of inflammatory bowel disease. Cumulative hazard curves for (A), inflammatory bowel disease, (B) Crohn’s disease and (C) Ulcerative colitis in patients with migraine compared to the general populations, respectively (control)1.
The exact pathogenesis of migraine is still undefined but implies numerous factors, including the gut-brain-axis may be at play. The term gut-brain-axis highlights the bidirectional relationship between the GI system and the central nervous system (CNS). As we know, hormones released by the hypothalamic pituitary adrenal (HPA) axis mediates the stress response which impacts the gut function. On the other hand, the GI system is believed to have a direct impact on the CNS and dysfunction of this axis is implicated to a number of neurological disorders such as multiple sclerosis, mood disorders and anxiety disorders (Figure 2)8. Dr. Dwebi emphasised that the gut microbiome may have a pivotal role in this complicated relationship since gut microbiomes are important producers of the short-chain fatty acids (SCFAs) which helps to maintain the gut barrier and functions8. In addition, the SCFAs have neuroprotective properties and this demonstrates the microbiome dysbiosis may predispose individuals to develop migraine9.
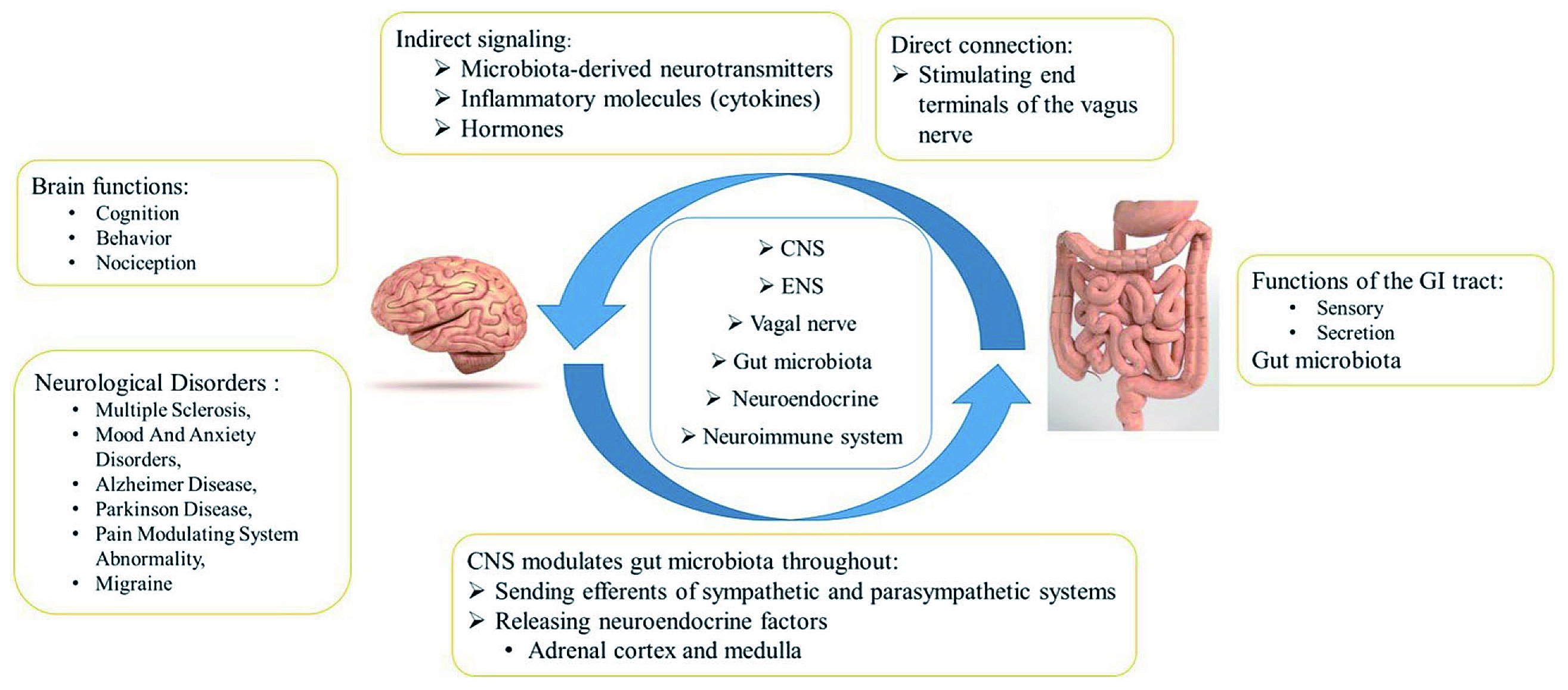
Figure 2. Gut-brain-axis. CNS= central nervous system; ENS= enteric nervous system; GI= gastrointestinal8.
What about the role of calcitonin gene related peptide (CGRP) in these diseases? A study by Pascual et al., (2023) assessed the serum levels of CGRP-alpha (CGRPα) level in patients with newly diagnosed IBD. 62 patients (27 with CD, 31 with UC and 4 with unclassified-IBD [U-IBD]) with newly diagnosed IBD with a mean age of 47.9 years were matched with 71 healthy controls. Samples were collected between 0 and 249 days after IBD diagnosis was established (median 50.5 days). Strikingly, the results demonstrated the serum CGRPα levels in patients with IBD were significantly increased compared to healthy controls. Furthermore, the CGRPα levels remained significantly elevated in IBD patients, regardless of their migraine status. The study concluded that there is a bidirectional, shared pathophysiology between migraine and IBD, which requires further exploration10. Dr. Dwebi advocated that physicians should remains vigilant in patients with persistent headaches since both IBD and migraine have detrimental effects on patient’s quality of life.
References
1. Lee CH, et al. Scientific Reports 2024; 14(1): 1157. 2. Olfati H, et al. Int J Prev Med 2023; 14: 66. 3. Pescador Ruschel MA, StatPearls Publishing LLC.; 2024. 4. Lin YK, et al. Medicine (Baltimore) 2016; 95(17): e3554. 5. Fathy M, et al. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery 2021; 57(1): 118. 6. Pascual-Mato M, et al. Cephalalgia 2024; 44(3): 03331024241233979.
Answers for CME quiz of Focus of Issue 23:





