
A Journey Through Glaucoma
Glaucoma is a collection of diseases which inadvertently causes an increase in the intraocular pressure (IOP), thereby, affecting the optic nerve and the visual fields. It affects about 70 million individuals and is the second leading cause of blindness globally. Notably, the risk factors for glaucoma includes having refractive error, chronic topical or systemic corticosteroid use, head or ocular trauma, previous ocular history and family history of glaucoma. Clinically, glaucoma can be divided into open-angle and closed-angle glaucoma, both of which can have primary or secondary causes1. Not surprisingly, 80% of all cases of glaucoma are open-angle glaucoma (OAG), a chronic, progressive, and irreversible multifactorial optic neuropathy that is characterised by optic nerve head changes, retinal nerve fibres layer thinning, and progressive loss of peripheral vision1. Primary OAG (POAG) is the commonest subtype, characterised by increased resistance to drainage in the trabecular meshwork.
However, the drainage angle between the cornea and iris remains open, but due to the blockage, the intraocular pressure (IOP) gradually rises causing optic nerve damage and progressive visual loss1. Considering glaucoma is typically an asymptomatic disease in its early stages, it is not uncommon for late diagnosis to occur with advanced glaucomatous damage already present2. Interestingly, the guidelines from the National Institute for Health and Care Excellence (NICE) suggested that patients presenting with advanced disease should be offered trabeculectomy as a primary intervention over the medical treatment; however, due to lack of evidence supporting primary surgery in such cases, most patients with advanced glaucoma often receive medical management initially, followed by trabeculectomy if medical management remains unsuccessful3. Nevertheless, some argued the validity for such approach since recent studies have suggested patients with advanced glaucoma may benefit from early surgical management to optimise their treatment outcome, in addition to improve their quality of life (QoL)4.
A Surgical Approach to Advanced Glaucoma
Visual impairment resulting from glaucoma is often preventable if it is diagnosed and treated early. However, since most patients with glaucoma remains asymptomatic during the early phase of the disease, they often present with symptoms when the disease is in more advanced stages. In fact, around 25% of patients with glaucoma demonstrate advanced disease in at least 1 eye at presentation in the United Kingdom (U.K.) and reducing IOP remains the only proven effective treatment against glaucoma with raised IOP4. Currently, there are two treatment options for patients with an advanced disease and they include the medical management and surgery. Remarkably, a Cochrane systematic review comparing primary medical versus surgical treatment for OAG based on 4 trials involving 888 patients with previously untreated OAG concluded that trabeculectomy may lower the IOP more than the medical treatment in patients with glaucoma; however, the trial excluded patients with more advanced disease, thus, these findings may not be applicable for patients with more advanced disease5. However, a 5-year multicentre randomised controlled trial by King et al., (2024) evaluated the effectiveness of primary trabeculectomy against medical treatment in patients with advanced glaucoma.
453 adults with newly diagnosed advanced OAG in at least 1 eye were recruited from 27 secondary care glaucoma departments in the U.K., 227 were allocated to trabeculectomy and 226 were allocated to the medical management. The primary outcome was vision-specific QoL measured with the 25-item Visual Function Questionnaire (VFQ-25) at 5 years and secondary outcomes were general health status, glaucoma-related QoL, clinical effectiveness (IOP, visual field, and visual acuity), and safety. Remarkably, at 5 years, the VFQ- 25 scores for trabeculectomy and medication arms were 83.3 ± 15.5 and 81.3 ± 17.5, respectively (Figure 1).
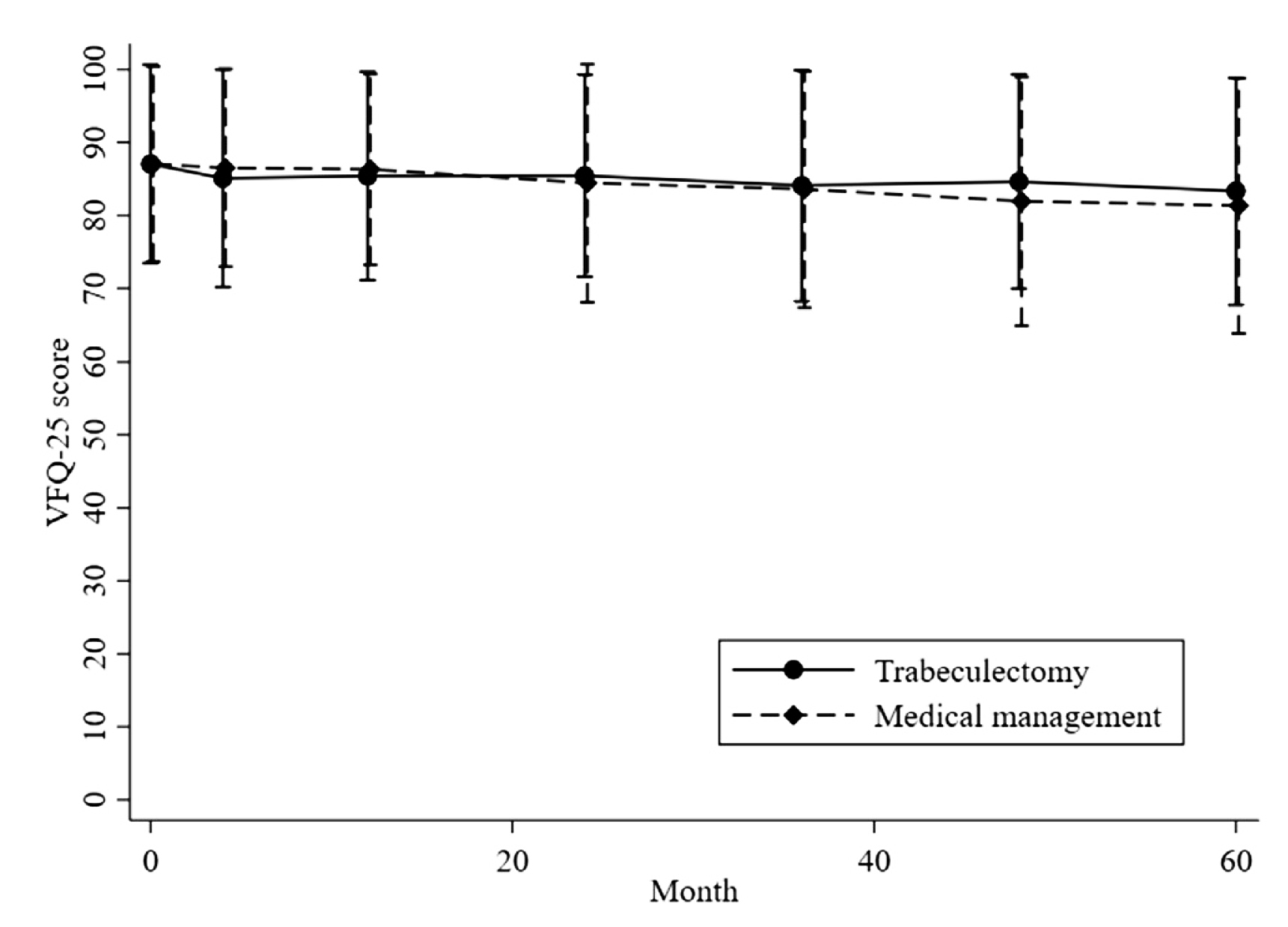
Figure 1. Quality-of-life outcomes up to 5 years for the 25-item Visual Function Questionnaire (VFQ-25)4.
The mean IOPs were 12.07 ± 5.18 mmHg and 14.76 ± 4.14 mmHg, respectively, and the mean difference was –2.56 (95% CI, –3.80 to –1.32; P < 0.001). The study concluded that primary trabeculectomy was more effective in lowering IOP, as well as preventing disease progression compared to the primary medical treatment in patients with advanced disease4.
Minimal Invasive Treatment vs Trabeculectomy
Although the global ophthalmological community still consider trabeculectomy being the gold standard surgical treatment for glaucoma, substantial effort has been made during the last decade to create a more innovative surgical procedure that is as effective as trabeculectomy, but with a better safety profile6. One such procedure is the microinvasive glaucoma surgery (MIGS) which is an innovative, subconjunctival draining using minimally invasive glaucoma device (microshunt) that creates a posterior bleb in the upper subconjunctival space. This reduces the inflammation and the rate of encapsulation during the surgery6. The efficacy and safety of microshunt and trabeculectomy in patients with advanced OAG was assessed in a single-centre study by Fili et al., (2022). Interestingly, 300 patients with moderated to advanced OAG were treated with either MicroShunt (n=150 eyes) or trabeculectomy (n=150 eyes).
During the 12-month follow-up period, 81.3% patients treated with microshunt showed a reduction in IOP by >20% without glaucoma eye drops, compared to 94% of patients treated with trabeculectomy. Strikingly, the number of topical medications administered 12 months after ocular surgery was 0.4±0.8 in group treated with microshunt compared to 0 in patients treated with trabeculectomy. Thus, the findings from this study suggested that microshunt was non-superior to trabeculectomy at reducing IOP after 12 months. In addition, patients undergone trabeculectomy had a better absolute success rates after 12 months compared to microshunt (Figure 2)6.
.jpg)
Figure 2. Mean intraocular pressure (IOP) values with standard deviations for the 12-month follow-up period6.
Despite newer surgical advancement for advanced glaucoma is still emerging, trabeculectomy remains vital since it remains the most commonly performed surgical procedure for medically uncontrolled glaucoma. Furthermore, thanks to peri- and postoperative modifications in recent years7, trabeculectomy has now become more safer and has improved surgical outcomes in patients with advanced glaucoma compared to the past.
References
1. PPMahabadi N, et al. StatPearls Publishing LLC.; 2024. 2. Díez-Álvarez L, et al. Archivos de la Sociedad Española de Oftalmología (English Edition) 2023; 98(1): 18-39. 3. King AJ, et al. Bmj 2021;
373: n1014. 4. King AJ, et al. Ophthalmology 2024; 131(7): 759-70. 5. Burr J, et al. Cochrane Database Syst Rev 2012; (9): Cd004399. 6. Fili S, et al. Cureus 2022; 14(8): e28288. 7. Wagner FM, et al.
BMJ Open 2023; 13(2): e068403.





