
With the recent outbreak of melioidosis in Hong Kong accounting for 34 cases reported up till late October1, it has become apparent that the public is concerned whether this is another new infectious disease like COVID-19. Melioidosis is endemic across tropical areas, especially in Southeast Asia and northern Australia.2 There have been cases recorded in Hong Kong each year, but the numbers are scarce. The symptoms can be asymptomatic, or the occurrence of pulmonary infection, bloodstream infection, local infection or disseminated infection. Diagnosis is based on clinical observation, epidemiological features, and bacterial culture. If not treated, the case fatality rate is 10-50%.3
Epidemiology and Risk Factors
The Gram-negative environmental bacterium Burkholderia pseudomallei causes melioidosis, which is found in contaminated soil and water. It is spread to humans and animals through direct contact with the contaminated source, but not contagious, and human-to-human transmission has been rarely reported.2 Zoonotic transmission to humans resulting in contact with livestock is extremely rare.3 B. pseudomallei has rarely been detected in the air.2 A review of hospitalised human cases of culture-confirmed melioidosis in the last twenty years showed an increasing trend in the incidence of the disease (Figure 1), of which 61 culture-confirmed cases of melioidosis were identified during this period. The overall fatality rate was 31.1%.4 Hence, this is a good reminder that melioidosis, though less prevalent, should not be neglected due to its high mortality and rising incidence.
The most common risk factor predisposing individuals to melioidosis is diabetes mellitus, which is present in over 50% of all patients with melioidosis worldwide.5,6 Other known risk factors include exposure to soil or water, male sex, age greater than 45 years, excessive alcohol consumption and liver disease, chronic lung disease, chronic kidney disease, thalassemia and prolonged steroid use/immunosuppression.3 Nonetheless, more than 80% of paediatric patients and around 20% of adult patients have no recognised risk factors.2
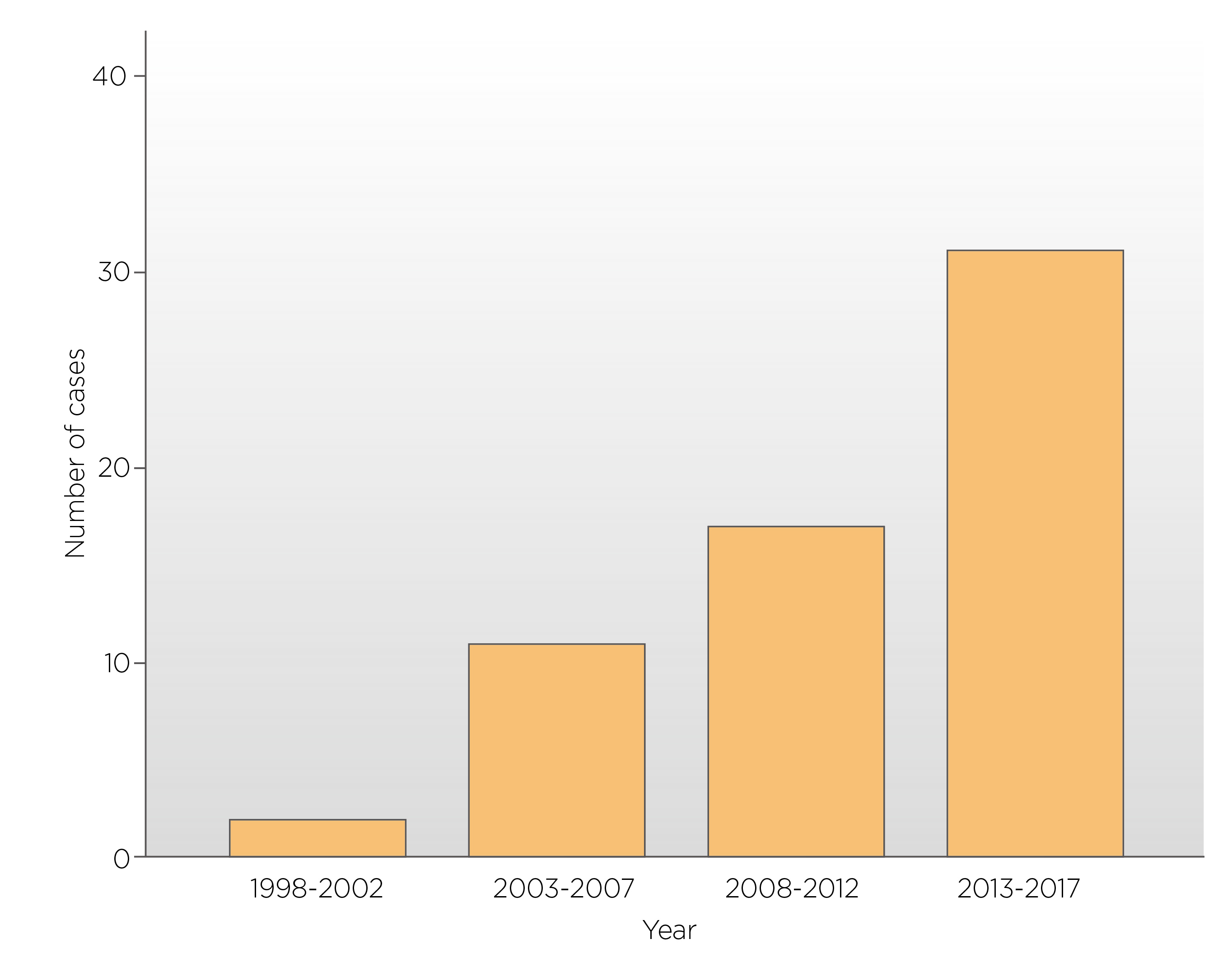
Figure 1. The number of culture-confirmed human cases of meliodosis over a 20-years period.
Clinical Diagnosis of Melioidosis and Treatments
Melioidosis, may present with localised infection, such as cutaneous abscess. Besides, pneumonia, meningoencephalitis, sepsis, or chronic suppurative infection are also common. Depending on the site of infection, common symptoms include fever, headache, localised pain or swelling, ulceration, chest pain, cough, haemoptysis, and swelling of regional lymph nodes.7 Bacterial culture remains the primary way in diagnosing melioidosis. B. pseudomallei can grow on most routine laboratory media but might not be recognised, and dismissed as a contaminant, or misidentified as another bacteria, such as Pseudomonas spp. and Bacillus spp.8 B. pseudomallei is never part of the normal human flora, and its isolation from any clinical samples should be regarded as diagnostic of melioidosis. Blood cultures are the most important sample. Other samples such as throat, rectal swabs, pus from abscesses, and sputum can also be used for culture.2 However, culture has a low sensitivity at 60%9. Thus, repeating cultures should be considered in patients with strong indications of B. pseudomallei infection, given it is common to find subsequent samples positive despite the initial negative result. There is an increasing number of clinical laboratories using matrix-assisted laser desorption/ionisation time of flight (MALDI-TOF) mass spectrometry for bacterial identification, as this method can provide accurate identification of B. pseudomallei.10
The selection of antibiotics against B. pseudomallei depends upon the susceptibility of the bacteria. The bacteria are generally susceptible to β-lactam antibiotics, such as ceftazidime, meropenem, imipenem, and co-amoxiclav which would kill the bacteria. Moreover, B. pseudomallei is also susceptible to doxycycline, chloramphenicol, and trimethoprim-sulfamethoxazole. These medications inhibit the growth of the bacteria. However, the bacteria are resistant to penicillin, ampicillin, the first and second-generation cephalosphorin, gentamicin, streptomycin, tobramycin, macrolides, and polymyxins.2
The antibiotic therapy for melioidosis consists of two phases: an initial intensive phase and an eradication phase. The initial intensive phase, which commonly last for a minimum of 10-14 days, consists of ceftazidime for cases in wards or meropenem for patients in intensive care units. Meropenem is the preferred initial intravenous therapy for neurological melioidosis. Consider adding trimethoprim-sulfamethoxazole, which has excellence in tissue penetration, in the doses recommended for the eradication phase from the start of the initial intensive phase in cases of neurological melioidosis, osteomyelitis and septic arthritis, skin and soft tissue infections and genitourinary infection including prostatic abscesses.11 Long-term intravenous therapy (≥4-8 weeks) is recommended for complicated pneumonia, and deep-seated infection, including prostate abscesses, neurological melioidosis, osteomyelitis and septic arthritis. Oral antibiotics are recommended for the subsequent eradication phase to prevent recrudescence of the disease. The eradication phase should last for ≥3 months, whereas extended eradication therapy (≥6 months) is recommended for neurological melioidosis and osteomyelitis. Co-amoxiclav and doxycycline are medications commonly used as the second choice. Essentially, side effects, such as rash, hyperkalemia, renal dysfunction, and gastrointestinal symptoms should prompt the reduction of trimethoprim-sulfamethoxazole doses.2
How to Prevent Melioidosis
Currently, there is no melioidosis vaccine available for human use.2 People are advised to avoid direct contact with soil and water. Rice farmers and gardeners are recommended to wear boots and gloves when direct contact with soil or water, only drink bottled water and avoid exposure to heavy rain or dust clouds. Any wounds should be cleaned up as soon as possible, and cover any cuts or grazes with waterproof dressings. No matter in low-income countries or high-income countries, water should be boiled before consumption. In addition, ultraviolet light treatment is effective for the remediation of water contaminated with B. pseudomallei.12 For the better management of the challenges that melioidosis brings to Hong Kong, an increase in awareness of this disease among the public and physicians is needed. Moreover, epidemiological surveillance should be carried out in the long term run to reduce the impact of the infectious disease.
References
1. The Government of the Hong Kong Special Administrative Region Press Releases. CHP investigates three additional confirmed melioidosis infection cases and plans to include melioidosis as statutorily notifiable infectious disease. https://www.info.gov.hk/gia/general/202210/25/P2022102500757.htm (Accessed on 1st Nov 2022) 2. Wiersinga et al. Na Rev Dis Primers. 2018;4:17107. 3. Cheng AC & Currie BJ. Clin Microbiol Rev. 2005;18:383-416 4. Lui et al. Trop Med Infect Dis. 2018;3:91 5. Limmathurotsakul et al. Clin Infect Dis. 2010;82:1113-1117. 6. Currie et al. Trop Med Int Health. 2004;9:1167-1174. 7. Centre for Health Protection, Department of Health, The Government of the HKSAR. Melioidosis. https://www.chp.gov.hk/en/healthtopics/content/24/101110/html (Accessed on 2nd Nov 2022) 8. Hoffmaster et al. Emer Infect Dis. 2015; 21(2):e141045. 9. Limmathurotsakul et al. PLoS ONE. 2010;5:e12485. 10. Suttisunhakul et al. PLoS ONE. 2017;12:e0175294. 11. Currie BJ. Respir Crit Care Med. 2015:36:111-125. 12. McRobb et al. Am J Trop Med Hyg. 2013;89:367-368.





