

Specialist in Dermatology
Custom Approach to Manage Periorbital Dermatitis
Periorbital dermatitis, also known as eyelid dermatitis, is a manifestation of various ocular pathology, dermatological conditions, such as atopic dermatitis, seborrheic dermatitis, allergic contact dermatitis, irritant dermatitis, rosacea and psoriasis, etc, and sometimes the reaction to ophthalmological medications1,2. In Hong Kong, there is no recent epidemiological data on its prevalence, yet reports from Germany suggest the incidence of periorbital dermatitis ranges from 3.9% to 4.8%2. Though the prevalence is not subtle, significance of a meticulous periocular dermatitis management approach remains undernoted.
Why Periocular Dermatitis Matters?
Periorbital dermatitis is comparably prevalent in adults and children with dermatitis on their face3. Common signs and symptoms include itch, reddish, dry, swollen and scaling of skin3,4. According to Dr. Hau Ngai Kingsley Chan, Specialist in Dermatology, patients may experience discomfort and pain of eyelids, inflammation and infection of eyes. Without proper management, periocular dermatitis can deteriorate and result in ophthalmological complications such as conjunctivitis, keratitis and keratoconus4-6.
“A female patient of mine presented with acute eyelid dermatitis due to the use of expired makeup products. She was late to treatment until eye infection occured which might lead to visual deterioration. Her condition was eventually managed through antibiotics. However, periorbital dermatitis could be managed by application of emollient or topical medication if prompt intervention is taken,” recalled Dr. Chan.
Don’t Wait until Ocular Complications Occur
Apart from these cases, data of Denmark study echoes that risk of developing ocular complications increases with severity of atopic dermatitis in mild and severe atopic dermatitis patients (Table 1)5. Though periocular dermatitis is not fatal, early and effective management is vital to protect ocular dermatological and visual health, as well as to defense patient’s quality of life and to avoid preventable complications6.
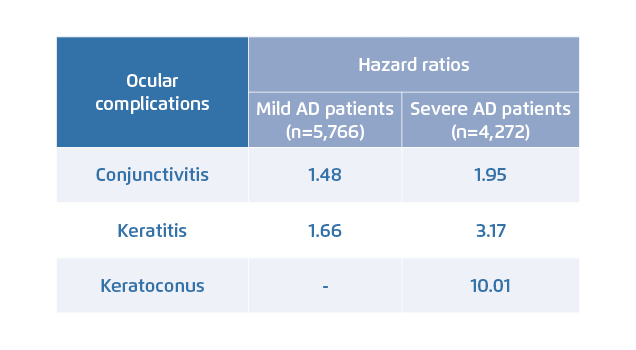
Table 1. Risk of ocular disease in mild and severe atopic dermatitis (AD) patients5
Differentiate the Cause under Medical Advice
Periocular dermatitis should be managed according to its cause and severity, it can also be treated by early interventions3,4. Nevertheless, various dermatitis show similar manifestations on eyelids and custom treatment modalities for periocular dermatitis is scarce, hence differentiation of allergy cause should be the first step to elicit appropriate treatment. “Patient could discuss with doctor for diagnostic test to elicit the cause of disease condition before committing to a treatment,” reminded Dr. Chan.
Go Beyond Pharmaceutical Treatment
In the past decades, topical steroids were often used to relieve dermatitis. Nevertheless, skin of eyelid is 4 to 5 times thinner than skin of other body parts, making it more prone to topical absorption and side effect of steroids. Potential side effects due to prolonged use of steroid such as thinning of skin and increased risk of glaucoma and cataract should be aware. “Even though some first-line non-steroid applications do not lead to skin atrophy and have profound therapeutic efficacy, uncomfortable burning sensation and photosensitivity effect brought along have affect treatment compliance,” said Dr. Chan2,3,7.
Going back to international guidelines, emollient is the first-line treatment for mild atopic dermatitis flare up and remains the backbone management for moderate to severe cases3. Only if symptoms do not subside after using emollient or emollient application on eyelid is not recommended, should mild topical steroids with 0.5% to 1% of hydrocortisone be considered3. According to a recent study by Lowe AJ in 2018, regular use of prophylactic emollients can significantly shrink the expression of atopic dermatitis8.
Among variety of active ingredients usually found in emollients, enoxolone, also known as glycyrrhetinic acid which is an extract from licorice, has demonstrated anti-inflammatory effects in animal testing and exerted therapeutic efficacy in improving atopic dermatitis severity, increasing time of relapse, reducing time of flares and potentiating effects of hydrocortisone in human testing9-11.
Attentive Daily Management Helps
Meanwhile, international guidelines also recommend restoration of skin barrier as mainstay of treatment for atopic dermatitis11. Apart from the well-known merit and common use of hyaluronic acid to restore skin hydration, phytosphingosine, which is a major component of phytoceramides, can also increase skin hydration as well as improve skin barrier function, stimulate epidermal differentiation and exert anti-inflammatory and antimicrobial activities12,13.
Novel study has revealed the virulence properties of staphylococcus aureus in the pathogenesis of atopic dermatitis, suggesting staphylococcus aureus to be an exacerbating factor for atopic dermatitis flare up, and may further deteriorate skin barrier health by destroying epithelial barrier integrity and immune system functioning14. Sucroester characterised with antimicrobial activity against staphylococcus aureus and property to remove existing biofilm infection can therefore help to defend skin barrier health simultaneously15,16.
Take Initiative to Manage Periorbital Dermatitis
Cycle of disease flare up, disease control and remission is normal but not necessary. Long-term management to prevent relapse is the key to successful disease control. Learning through the storm of COVID-19 we are weathering, good hygiene practice is always fundamental to infection control. The same shall apply while managing periorbital dermatitis, in which patients should pay particular attention to their daily habits, for example cleaning of eyelids and avoiding contact with irritants and allergens, especially those in makeup or skincare products, so as to minimise the risk of contamination and infection through any route2.
References
1. Wolf R, et al. Clin Dermatol. 2014;32:131-140. 2. Feser A, et al. JDDG. 2010;8:159-165. 3. National Eczema Society. Eczema around the eyes factsheet. 4. American Academy of Dermatology. Available at: ttps://www.aad.org/eye-problems (Accessed on 29 Feb 2020). 5. Thyssen JP, et al. J Am Acad Dermtol. 2017;77:280-286. 6. Guo Y, et al. Sci Rep. 2016;6:29571. 7. Arkwright PD, et al. J Allergy Clin Immunol. 2013;1:143-151. 8. Lowe AJ, et al. Ann Allergy Asthma Immunol. 2018;120:145-151. 9. Yang R, et al. Pharm Biol. 2017;55:5-18. 10. American College of Toxicology Cosmetic Ingredient Review Expert Panel. Int J Toxicol. 2007;26:79-112. 11. Micali G, et al. G Ital Dermatol Venereol. 2018;153:396-402. 12. Spada F, et al. Clin CosmetInvestig Dermatol. 2018;11:491-497. 13. Choi HK, et al. Arch Dermatol Res. 2017;309:795-803. 14. Blicharz L, et al. Adv Dermatol Allergol. 2019;36:11-17. 15. Matev G, et al. Conference Paper: Challanges in chemistry. 2013. 16. Zhang H, et al. J Ind Microbiol Biotechnol. 2015;4:57-61.





