
Honorary Consultant in Allergy
Specialist in Paediatric Immunology and Infectious Diseases
Hong Kong Sanatorium and Hospital
Improving Skin-barrier to Minimise the Development of Skin Allergy
Skin allergy such as atopic dermatitis (AD) is common. In Hong Kong, one in five people have episodes of eczema in their lifetime and children aged one to two years old have the highest prevalence rate1,2. Recent epidemiological data reveal a tripled prevalence of AD in industrialised countries in the past 30 years. Of which, the prevalence of AD among children and adults are 15% to 30% and 2% to 10% respectively and about half of patients with moderate to severe AD also suffer from other forms of allergies such as allergic rhinitis3,4. Despite the fact that AD is not life-threatening, patients may have their quality of life impacted by the symptoms such as intense itch2. The relentless increment also implies a higher demand on healthcare service and the need of a well-developed holistic approach to manage skin allergy for better prognosis.
Atopic dermatitis is a chronic inflammatory skin disease occurred when the immune system reacts abnormally against harmless antigens5,6. It usually appears with symptoms of itch, rash, lichenification, reddened and swollen skin7. Infected skin may also blister and ooze7. Genetic factors such as the filaggrin gene (FLG) defect and environmental factors such as air pollution and presence of allergens are risk factors of AD7-9. People who have skin-barrier dysfunction and defective immune system are also prone to be affected10.
Months ago there was a young lady who had been tormented by AD ended her life. “We regret to hear about the incidence. The constant breakthrough in treatment options has offered a variety of quality treatments to AD patients.” Dr. Chan Wai Ming, Alson, Honorary Consultant in Allergy from Hong Kong Sanatorium and Hospital said. The incidence provokes reflection on current management approach to AD.
First-line treatment targets skin-barrier
Conventional and commonly-known treatments include the use of corticosteroid, moisturisers, antibiotics and avoidance to allergens11. These treatment approaches target to sooth pruritus, suppress inflammation and eliminate infection11. Yet, when stepping forward beyond the ubiquitous use of corticosteroid, advanced treatments to cure AD is just there. “Desensitisation (immunotherapy) targeting the triggering allergens provides the new hope of cure.” Dr. Chan explained. Though immunotherapy has a history of over a hundred years, it is a relatively novel treatment modality in Hong Kong in the last decade and is utilised to achieve long-term control12. “By simple but targeted diagnostic allergy tests, those culprits of the allergy diseases can be identified. Patients can then relieved from allergic condition by coaching their immune system to adapt the allergens.” Dr. Chan explained. Immunotherapy can be administered through injection or by oral routes.
While allergy testing gives the blueprint for desensitisation, Dr. Chan reminded that not all laboratory testings on allergens have the same accuracy. Authorities including the American Academy of Allergy Asthma and Immunology have commented that blood testing on immunoglobulin G (IgG) which is becoming more common nowadays lacks scientific and clinical relevance13,14. “Patients shall not comply stringent food avoidance recklessly without the use of appropriate allergy test and consultation with doctors. Empirical food avoidance, on the long run, can cause malnutrition and even lead to more allergic sensitisation in eczema patients.” Dr. Chan reminded.
Nonetheless, while immunotherapy brings hope to ameliorate AD, protection of skin-barrier for proper management of AD remains critical. “The first-line treatment of AD is to protect skin-barrier.” Dr. Chan said.
Skin-barrier as the first defense against skin problems
The skin-barrier plays a key part in maintaining skin homeostasis15. Healthy skin-barrier is of paramount importance for long-term management of AD and to prevent AD development15. Serving as the first line of defense, skin-barrier blocks external pathogens and antigens from penetrating through into the body, thus preventing the morbid triggering of immune system which may attenuate skin-barrier further15-18. According to Cork (2006), skin-barrier was thinnest in areas most susceptible to the occurrence of AD16.
The use of moisturisers is a simple measure to restore skin-barrier integrity and soothe itch11. “Applying emollients to improve skin-barrier is the first-line treatment. It brings the least side effects to patients and can prevent the progression of skin allergy.” Dr. Chan commented. Recent study also suggests that interventions to improve skin-barrier function can approximately halve the incidence of atopic dermatitis in neonates18.
Choose between active ingredients in emollients
Routine use of moisturisers can improve skin-barrier health and reduces the use of corticosteroid and rate of flare-ups by 3.7 folds2,18. While there is constant breakthrough in treatment options and treatment quality, nevertheless, choosing emollients with suitable active ingredients is critical to target patient’s need. “We have to take into account different factors when choosing between emollients such as patient’s skin type, root cause of the skin allergy and the texture of the emollient.” Dr. Chan added.
Epigallocatechin gallate (EGCG) is a catechin that can be abundantly found in green tea19. Apart from its antioxidant property, it also demonstrates anti-inflammatory, skin hydration and moisture retention effect by regulating related genes expression, including the FLG19,20. Besides, other active ingredients such as glycyrrhetinic acid and urea can also improve AD and reduce time of flares21. Emollients with ceramide can also ameliorate skin-barrier function by increasing skin hydration22. While many skin-barrier products contain multiple active ingredients, synergistic effect may be beneficial21.
The possibility and hope to eradicate skin allergy
Eradication of AD is no longer a fairy tale nowadays. “I have some patients with very dry skin whose AD was cured after frequent use (at least three times a day) of emollients for several months. Atopic dermatitis is no longer a disease without cure, yet patients have to adhere to treatment.” Dr. Chan said. In Hong Kong, treatment of AD is not lacking. However, apart from the mainstay of treatment to relief symptoms and the novel technology to tackle the root cause, early interventions to strengthen skin-barrier is vital to improve skin health in general (Figure 1), so as to battle against the soaring incidence of AD5.
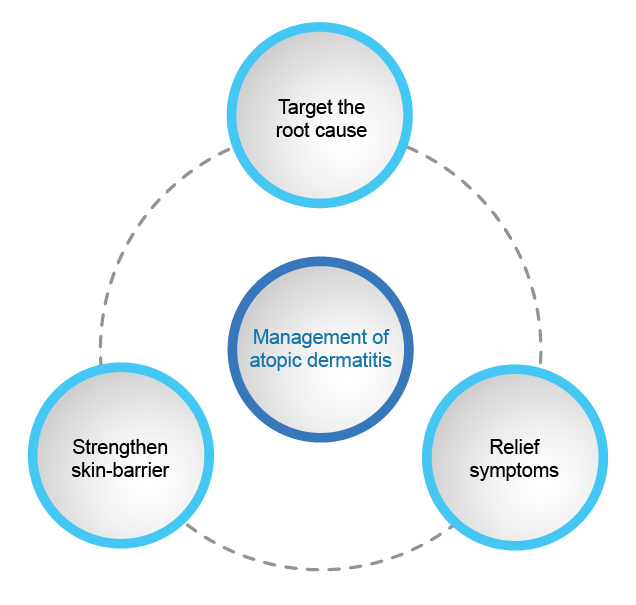
Figure 1. The need of a more holistic approach to manage atopic dermatitis
References
1. The Hong Kong Allergy Association. Eczema. Available at: http://www.allergyhk.org/?page_id=317 (Accessed on 25 Jan 2019). 2. Guo Y, Li P, Tang J, et al. Scientific Reports. 2016;6:1-7. 3. Becker A and Rensberry M. Am Fam Physician. 2018;97:18-19. 4. American Academy of Allergy Asthma and Immunology. Eczema (Atopic Dermatitis) Overview. Available at: https://www.aaaai.org/conditions-and-treatments/library/allergy-library/eczema-atopic-dermatitis (Accessed on 20 Feb 2019). 5. Boguniewicz M and Leung YM. Immunol Rev. 2011;242: 233-246. 6. Roesner LM, Werfel T and Heratizadeh A . Expert Rev Clin Immunol. 2016;12:787-796. 7. Student Health Service, Department of Health. Eczema. Available at: https://www.studenthealth.gov.hk/english/health/health_ophp/health_ophp_tet.html (Accessed on 24 Jan 2019). 8. Irvine AD, McLean WHI and Leung YM. N Engl J Med. 2011;365:1315-1327. 9. Chan WM, Chan KC, Tam YC, et al. Hong Kong Med J. 2016;22:279-285. 10. Kim BE and Leung YM. Allergy Asthma Immunol Res. 2018;10:207-215. 11. The British Society for Allergy & Clinical Immunology. Atopic Eczema (Dermatitis). Available at: https://www.bsaci.org/resources/atopic-eczema (Accessed on 25 Jan 2019). 12. Fitzhugh DJ and Lockey RF. Curr Opin Allergy Clin Immunol. 2011;11:554-559. 13. American Academy of Allergy Asthma and Immunology. The myth of IgG food panel testing. Available at: https://www.aaaai.org/conditions-and-treatments/library/allergy-library/IgG-food-test (Accessed on 20 Feb 2019). 14. Hong Kong Institute of Allergy. Guidelines on Allergy Diagnosis. 15. Egawa G and Kabashima K. Allergol Int. 2018;3-11. 16. Cork MJ, Robinson DA, Vasilopoulos Y, et al. J Allergy Clin Immunol. 2006;118:3-21. 17. Nutten S. Ann Nutr Metab. 2015;66:8-16. 18. Lowe AJ, Leung YM, Tang LK, et al. Ann Allergy Asthma Immunol. 2018;120:145-151. 19. Kim E, Hwang K, Lee J, et al. Int J Mol Sci. 2018;19:173. 20. Chu C, Deng J, Man Y, et al. BioMed Res Int. 2017. 21. Micali G, Paternò V, Cannarella R, et al. G Ital Dermatol Venereol. 2018;153:396-402. 22. Spada F, Barnes TM, Greive KA . Clin Cosmet Investig Dermatol. 2018;11:491-497.





