
Specialist in Neurology
Consultant Neurologist
Hong Kong Adventist Hospital, Hong Kong

Emertius Professor &
Honorary Professor
Division of Neurology, Department of Medicine & Therapeutics
Faculty of Medicine,
The Chinese University of Hong Kong

Senior Consultant
Division of Neurology
Department of Medicine
National University Hospital, Singapore

Professor of Neurology
Chairman of the Department of Neurology
Director of the Essen Headache Centre
The University of Du-isburg-Essen, Germany

Professor of Neurology
Director of NIHR Clinical Research Facility
King's College London,
United Kingdom
Migraine remains the second among the world's leading causes of disability and first among young females.1 Migraine attacks significantly impair a patient's quality of life and contribute to substantial economic burdens. In this regard, preventive migraine treatment is essential for reducing the frequency and intensity of migraine attacks. In a recent symposium, world's renowned scholars and clinicians from overseas and Hong Kong highlighted the development of eptinezumab, a novel calcitonin gene-related peptide (CGRP) therapy which targets the pain transmission pathways and presented its efficacy in treating debilitating symptoms of migraine in a clinical setting.
Migraine is a neurological disorder responsible for approximately 42.1 million years lost to disability (YLD) globally in 2019. The disorder imposes a substantial health and economic burden, as well as indirect cost related to absence from work.2 Furthermore, Prof. Goadsby highlighted that the prevalence of migraine is highest between age groups 30 and 39 years and is three times more common among females compared to the males (Figure 1).3
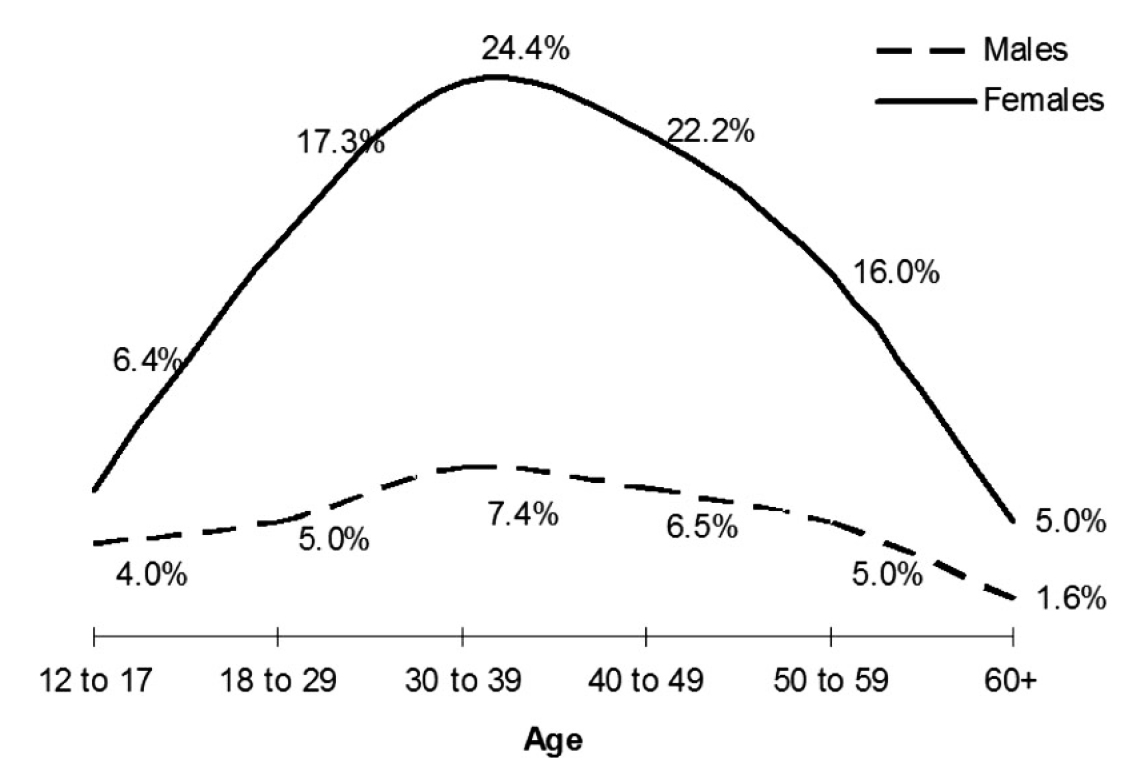
Figure 1. One-year period prevalence of migraine by age and sex3
Prof. Goadsby advised that clinicians tend to focus on the number of migraine days or hours when evaluating the impact of the disorder. However, awareness on migraine-related functional impairment is equally important. According to the American Migraine Prevalence and Prevention (AMPP) Study, about 54% of female patients with migraine reported to suffer from severe impairment or required bed rest, whereas only 7% claimed to work normally.4 Notably, patients with episodic migraine (EM) often progress into chronic migraine (CM), which is characterised by ≥15 headache days per month with a high severity for more than 3 months, which, on at least 8 days per month, has the features of migraine headache, at a rate of about 2.5% per year.5 To reduce the number of migraine days, Prof. Goadsby recommended a good sleeping habit, a healthy diet, balanced with physical activities. In addition, he suggested reducing caffeine intake and managing stress appropriately.
The pharmacotherapy for migraine can be categorised into acute, bridging, and preventive therapies. According to Prof. Goadsby, triptans are commonly used to treat symptoms of acute migraine, followed by aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), and oral CGRP. Nerve blocks and dihydro-ergotamine are often used during bridging therapies aiming to reduce migraine frequency. Even though beta-blockers and anticonvulsants are prophylactically used to treat migraine, they also have many adverse effects (AEs).1 In fact, around 80% of patients on preventive therapy discontinued treatment within 1 year,6 with lack of efficacy and adverse effects being primary reasons for treatment discontinuation.7
According to Prof. Goadsby, preventive treatment should be considered if a patient reports severe headaches for more than 2 days per month. In patients having ≥6 headache days per month, preventive treatment should be offered.8 Nonetheless, Prof. Goadsby reiterated not to overuse acute treatments. For instance, triptan treatment for ≥10 days should be avoided, and the primary goal of migraine prevention should focus on improving patient's function and reducing disability.
Preventive migraine therapies can be divided into non-specific treatments and migraine-specific treatments. Remarkably, the presence of CGRP in the trigeminovascular system and their release during migraine attacks have been investigated to determine the role of CGRP in migraine.9 Recent studies have shown that CGRP helps regulate the blood flow to the brain and pain-sensitive meninges and is also involved in neurogenic inflammation. Moreover, CGRP plays a role in relaying nociceptive impulses which leads to an increase in pain transmission.10 These findings have led to the development of anti-CGRP monoclonal antibodies (mAb) as migraine-specific preventive therapies for both EM and CM.
Anti-CGRP therapies have been reported to improve tolerability, with high specificity and selectivity for the CGRP receptor or ligand, thereby reducing the risk of off-target binding and toxicity.11 Therefore, the anti-CGRP therapies are effective in preventing migraine, in addition to reducing the use of acute migraine medications and improving the quality of life (QoL) of patients with migraine.11
Eptinezumab is a humanised mAb that prevents migraine by selectively binding to both alpha and beta-CGRP ligands, antagonising them from binding to CGRP receptors. More importantly, eptinezumab dissociates slowly, which explains its rapid onset and longer therapeutic effects.12 While other anti-CGRP therapies such as erenumab, fremanezumab, and galcanezumab, are administered subcutaneously (SC), eptinezumab is administered through intravenous (IV) infusion, hence it achieves a 100% bioavailability by the end of its half an hour infusion.12 Notably, Prof. Goadsby highlighted that humanised mAb carry a lower risk for inducing immune responses in humans compared to animal derived antibodies. He further elaborated that eptinezumab is optimised to bind CGRP with high affinity and specificity.
Preventive migraine therapies are effective in most cases. However, there is a significant proportion of patients who are not able to tolerate traditional therapies or have severe migraine requiring additional treatments. Therefore, migraine specific anti-CGRP therapies are also developed for migraine prevention, apart from treating acute attacks.
“In comparison, non-specific preventive therapies are less effective than monoclonal anti-CGRP therapies at the same cost,” according to Prof. Diener. A meta-analysis performed on 215 randomised controlled trials (RCTs) by Shamliyan et al. (2013) suggested the evidence supporting the use of non-specific preventive treatments was low due to the risk of bias and imprecision. In addition, the long-term effects(> 3 months) of these agents on QoL remains elusive.13 Prof. Diener explained that preventive medications often require 2 to 6 months prior to patient experiencing maximal response14, nonetheless, the treatment related side effects are experienced immediately.
A systematic review of 20 RCTs performed by Drellia et al. (2021) on both the number needed to treat (NNT) for reducing migraine days by ≥50% and discontinuation due to side effects indicated that all anti-CGRP mAb preventive migraine therapies offered more beneficial effects than harmful effects in cases of EM and CM. Notably, the NNT for reducing migraine days by ≥50% of eptinezumab varied from 5 to 6.15 “These anti-CGRP antibodies are very well-tolerated with a high efficacy,” as per Prof. Diener.
Prof. Diener noted eptinezumab being efficacious in reducing the frequency of migraine days, and the severity of headache, with onset of effect as early as day 1. Moreover, two-thirds of patients on eptinezumab reported a sustained decrease in disability over a 2-year period. Prof. Diener's observations were supported by established clinical data, for instance, in the PROMISE-1 trial involving 888 patients with EM, eptinezumab administration at 100 mg and 300 mg, significantly reduced monthly migraine days (MMDs) across weeks 1–12 and achieved more than 50% migraine responder rates compared to placebo. In summary, the results showed that the migraine preventive treatment was effective on day 1 after eptinezumab administration and well-tolerated by patients.16
Similarly, the efficacy of eptinezumab in patients with CM and medication-overuse headache (MOH) was demonstrated in the PROMISE-2 trial. Eptinezumab-treated patients experienced a greater reduction from baseline in MMDs than placebo. Moreover, more eptinezumab-treated patients were ≥50% migraine responders or ≥75% responders over weeks 1–12. The therapeutic benefits of eptinezumab were observed from day 1 with effects sustained over 24 weeks.17
The DELIVER trial evaluated the efficacy of eptinezumab in patients with severe migraine who had failed to respond to the oral therapies. Among the 865 patients who failed 2 to 4 previous preventive treatments, the change in mean MMD from baseline with eptinezumab was significantly higher than that with placebo at week 12. Moreover, eptinezumab-treated patients had a greater reduction in the percentage of severe migraine attacks, monthly headache days, and monthly headache episodes compared to placebo.18 Particularly, Prof. Diener presented the indirect comparison in ≥50% responder rates in patients who failed prior preventive treatments that eptinezumab yielded promising responder rates (Figure 2).
Figure 2. ≥50% responder rates in patients with prior preventive treatment failures achieved by anti-CGRP therapies, **p=0.002, ***p<0.0001
The onset of treatment effects of eptinezumab (100 mg) during a migraine attack was evaluated in the RELIEF trial involving 480 patients. The results indicated that eptinezumab achieved significantly quicker headache pain freedom (median: 4 hours vs 9 hours, p<0.001) and absence of most bothersome symptom (median: 2 hours vs 3 hours, p<0.001) compared to placebo. Remarkably, 23.5% of patients on eptinezumab showed headache pain freedom and 55.5% reported absence of most bothersome symptom as early as 2 hours after infusion. In addition, there were significantly fewer eptinezumab-treated patients who required rescue medication within 24 hours compared to placebo (Figure 3).19 These findings further substantiated that eptinezumab offers rapid relief. Prof. Diener suggested that the early onset and sustained effects of eptinezumab are likely to improve patient's adherence to treatment.

Figure 3. Onset of treatment effects of eptinezumab,19 MBS: most bothersome symptom, ***p < 0.001
The long-term safety and efficacy of eptinezumab (300 mg) was assessed in the PREVAIL trial. The results demonstrated that 60% of CM patients with severe disability reported no significant impact of migraine upon eptinezumab over the 2 years course (Figure 4). Furthermore, most treatment-emergent adverse events (TEAEs, 95.6%) were mild or moderate in nature with eptinezumab.20
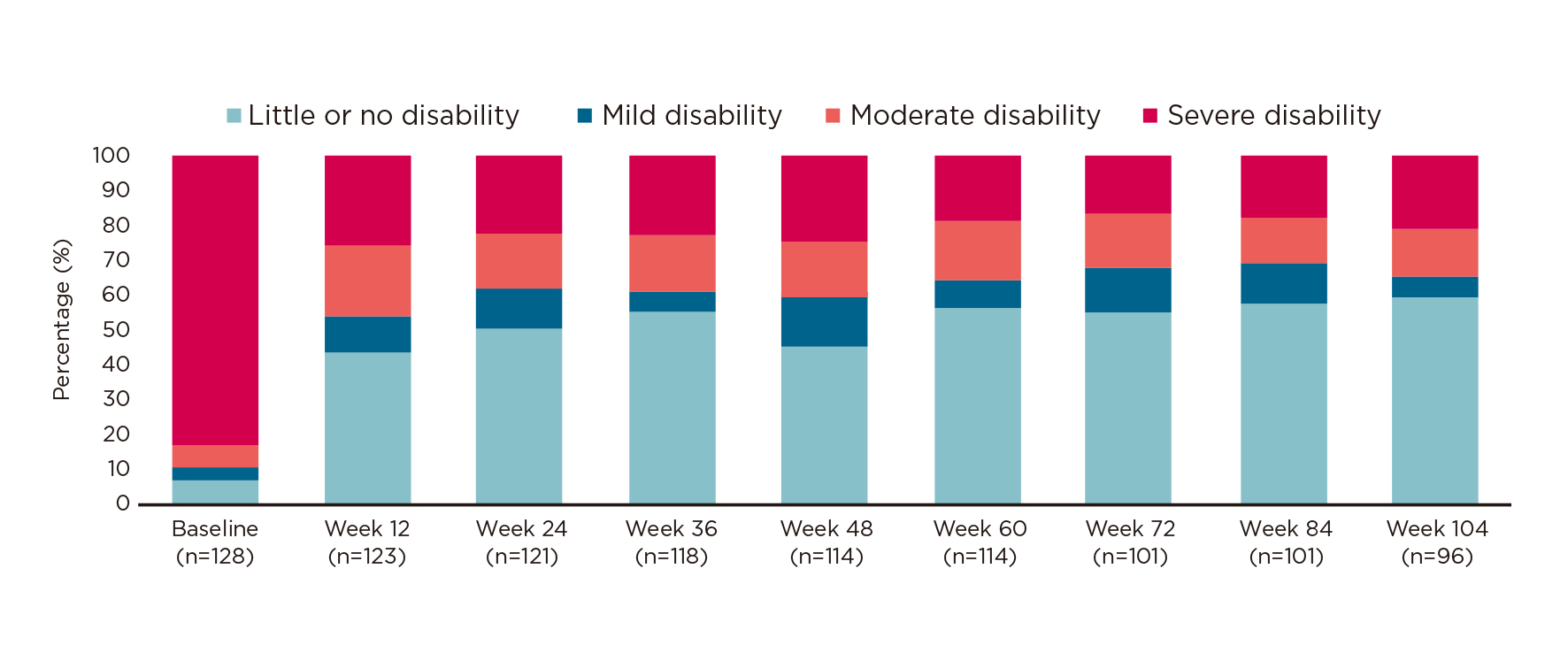
Figure 4. Changes in proportion of patients with severe disability treated with eptinezumab20
Prof. Diener explained that patients with migraine tend to overuse acute medications, and they will become less responsive to the migraine treatment and resulting in MOH, nonetheless, eptinezumab can help intervene this vicious cycle. He further highlighted that while all anti-CGRP therapies are proven to be effective against medication overuse (MO), eptinezumab is the only anti-CGRP therapy with trial data supporting efficacy in both MOH and MO.
To put in perspective the use of anti-CGRP mAb therapy in routine clinical practice, Dr. Ong shared the case of Ms. Linda, a 34-year-old, commercial lawyer who was referred to Dr. Ong with a background of remission in depression. Ms. Linda was a non-smoker but consumed alcohol once or twice a week. She often had 6-7 hours of sleep and exercised regularly.
In the last 6 months, Ms. Linda reported an average of 10 headache days per month, 8 of which were of severe intensity. As per The International Classification of Headache Disorders (ICHD)-3 (2018) criteria, a diagnosis of EM without aura was documented. Ms. Linda was treated with various treatments, such as flunarizine, topiramate, and propranolol. Unfortunately, the treatments were either ineffective or poorly tolerated.
Ms. Linda was referred to Dr. Ong with severe, unremitting, and debilitating headaches that lasted for 4 days. She reported significant nausea, vomiting associated with photophobia and phonophobia. The painkillers remained ineffective. Therefore, Ms. Linda was admitted under the Neurology team after being seen by the Emergency department.
According to Dr. Ong, Ms. Linda was diagnosed with status migrainosus. Her acute treatment was escalated to naproxen for mild attacks and zolmitriptan for moderate-to-severe attacks. For preventive treatment, eptinezumab was initiated. In addition, Dr. Ong's team also advised Ms. Linda to avoid alcohol. The treatment regimen eventually helped to break the vicious cycle of migraine headaches and offered Ms. Linda relief within the first 48 hours. Furthermore, both photophobia and phonophobia resolved. Eventually she was discharged from the Neurology ward on day 3 and on follow-up after 3 months, she reported her migraine frequency continued to improve reaching 3-4 days per month with only 1 severe attack on average. Moreover, she was less reliant on acute treatment and her QoL improved significantly. Of note, Dr. Ong added that Ms. Linda has received an additional dose of eptinezumab and reported sustained benefits.
A second case shared by Dr. Ong involved Madam Sophia, a 62-year-old female retired banker with hypertension and dyslipidaemia. In addition, she previously had nephrolithiasis and cholelithiasis which required surgical intervention. Madam Sophia often avoided caffeine to prevent headaches. Madam Sophia was diagnosed with EM with no aura (ICHD-3 2018). In the past, migraine attacks were more frequent, particularly during menstruation but the frequency reduced upon menopause. Her average MMD was 2-3, with mild-to-moderate intensity during her referral to Dr. Ong.
Madam Sophia contracted coronavirus disease 2019 (COVID-19) in May 2021 and, 2 weeks post-infection, she experienced a gradual increase in migraine frequency to 22 MMDs, with 10 days of moderate-to-severe attacks. During the attack, there were significant episodes of nausea, vertigo, brain fog, nuchal discomfort, and photophobia. Therefore, she was heavily reliant on acute treatment, utilising it for 16-18 days per month and her QoL was substantially affected.
To exclude other causes of headache, blood tests, analysis on cerebrospinal fluid (CSF), and magnetic resonance imaging (MRI) of brain with contrast were conducted but remained unremarkable. Therefore, the diagnosis of CM and MOH to paracetamol was documented. For the acute treatment of MOH, naproxen was mainly used for mild attacks and sumatriptan for moderate-to-severe attacks.
For CM, Dr. Ong initiated erenumab for 2 months with modest response (18 days), and constipation being the main side-effect. Hence, Madam Sophia was switched to galcanezumab with no improvements being observed. Therefore, Madam Sophia was offered onabotulinumtoxin A injections, but she refused and decided to proceed with eptinezumab treatment.
After the first dose of eptinezumab, the headache frequency reduced to 10 MMDs, with lower vertigo and brain fog episodes reported. The MMD was further reduced to 7 days after the second dose of eptinezumab, and non-painful symptoms showed significant improvement. Moreover, after the third dose, the headache frequency reduced to 4-5 days and the attacks were primarily mild-to-moderate. In addition, the beneficial effects of sumatriptan and naproxen became more consistent as Madam Sophia became less reliant on acute medications and her QoL improved immensely.
In the cases of Ms. Linda and Madam Sophia, the early onset action of eptinezumab permits its use in acute setting in both EM and CM with MOH. Moreover, eptinezumab was efficacious in reducing migraine days, duration, and intensity in both cases. While oral and other anti-CGRP therapies failed in Madam Sophia’s case, eptinezumab remained effective and exhibited positive outcomes on non-painful symptoms. More importantly, these clinical cases demonstrated that eptinezumab is safe and well-tolerated.
Prof. Wong shared a case of an 18-year-old female boarding school student who was on treatment for both asthma and attention deficit hyperactivity disorder (ADHD). Her father often suffered from severe migraines and the patient reported to have experienced right temporal headaches every other day which lasted for approximately 4-8 hours. The headaches were preceded by visual auras, followed by nausea, vomiting, photophobia and phonophobia.
A diagnosis of CM with aura was made and despite two oral prophylactic medications, her symptoms did not improve. Furthermore, due to asthma, beta-blockers were contraindicated, and she eventually started fremanezumab. Her symptoms showed some improvement, but photophobia persisted which affected her studies. Subsequently, Prof. Wong initiated the patient on eptinezumab and the treatment reduced her symptoms to only mild migraine. No photophobia was reported, and the patient resumed her studies.
Another case shared by Dr. Fong was about a female artist aged 61 who had active EM for 40 years, with around 4-10 attacks per month on average and some of the attacks lasted for 1-2 days. Even though sumatriptan helped relieve headaches, the patient often required more than 20 tablets per month to control her symptoms. In addition, she had tried propranolol but reported no benefit.
Notably, the patient was on carbamazepine for nocturnal epilepsy since 1997. She had a significant family history of coronary artery disease and was on treatment for hypertension and dyslipidaemia. Given that the patient overused sumatriptan, Dr. Fong expressed his concern regarding the overuse of sumatriptan and the tendency of sumatriptan to cause coronary vasoconstriction.
Eventually, the patient was introduced to the anti-CGRP migraine therapies, and she was keen to initiate the treatment. The patient chose to commence on eptinezumab for its established efficacy. 3 weeks post-treatment, she reported no side effect with 90% reduction in migraine frequency and severity. The patient was scheduled to receive the second dose of eptinezumab in 3 months' time.
Summarising the biology of eptinezumab, Prof. Goadsby highlighted that while the high specificity for CGRP ligand of eptinezumab prevents off-target activity, the high affinity for the ligand also facilitates long-duration of therapeutic effects of eptinezumab. Together with the 100% bioavailability, eptinezumab is designed to provide an effective, rapid, and sustainable response against migraine. Prof. Diener added that the quick clinical onset and favourable dosing interval of eptinezumab is likely to improve treatment adherence. On this note, Dr. Ong advocated that eptinezumab is effective, safe, and well-tolerated. In practice, the downtime of eptinezumab is minimal allowing patients to pre-plan their schedules. The local cases shared by Prof. Wong and Dr. Fong demonstrated the effectiveness of eptinezumab in reducing migraine frequency and intensity in different age groups with different comorbidities that are not amenable to oral prophylactic treatment.
References
1. Bentivegna et al. Neurol Ther 2023; 12: 337–42. 2. Salazar et al. Int J Environ Res Public Health 2021; 18: 11145. 3. Lipton et al. Neurology 2007; 68: 343–9. 4. Buse et al. Headache 2013; 53: 1278–99. 5. Lipton et al. Headache 2015; 55 Suppl 2: 103–22. 6. Hepp et al. Cephalalgia 2015; 35: 478–88. 7. Blumenfeld et al. Headache 2013; 53: 644–55. 8. Ailani et al. Headache 2021; 61: 1021–39. 9. Vandervorst et al. J Headache Pain 2021; 22. DOI:10.1186/S10194-021-01335-2. 10. Durham. N Engl J Med 2004; 350: 1073–5. 11. Reuter. Headache: The Journal of Head and Face Pain 2018; 58: 48–59. 12. Datta et al. Cureus 2021; 13. DOI:10.7759/CUREUS.18032. 13. Shamliyan et al. Journal of General Internal Medicine 2013 28:9 2013; 28: 1225–37. 14. Silberstein. Continuum: Lifelong Learning in Neurology 2015; 21: 973. 15. Drellia et al. Cephalalgia 2021; 41: 851–64. 16. Ashina et al. Cephalalgia 2020; 40: 241–54. 17. Diener et al. Headache 2021; 61: 125–36. 18. Ashina et al. Lancet Neurol 2022; 21: 597–607. 19. Winner et al. JAMA 2021; 325: 2348–56. 20. Kudrow et al. BMC Neurol 2021; 21: 1–12.





