

Specialist in Psychiatry
Major depressive disorder (MDD) is a severe, recurrent, and debilitating condition affecting more than 160 million people of all ages globally1. The disorder is characterised by symptoms including persistent depressive mood, anhedonia, and feelings of worthlessness or guilt2, which then substantially impairs the patient's quality of life (QoL). Apart from psychological interventions and neuromodulation, pharmacological treatment is essential in the management of MDD. The efficacy of selective serotonin reuptake inhibitors (SSRIs) or serotonin-noradrenaline reuptake inhibitors (SNRIs) traditionally used in controlling depressive symptoms has been widely reported, in addition to their side effect profile. Remarkably, almost half of the MDD patients on conventional antidepressants experiences emotional blunting3. In a recent interview, Dr. Wong Ming Cheuk Michael discussed the strategy used to manage emotional blunting and highlighted the clinical performance of multimodal antidepressants in counteracting these clinical effects among MDD patients.
Currently, there is no consensus on the actual definition of emotional blunting, and the condition is prevalent among MDD patients. “Patients experiencing emotional blunting may appear desensitised to emotions. For instance, they may not show contentment during a pleasant trip and feel no sorrow when a close relative deceased,” according to Dr. Wong. He emphasised that patients with emotional blunting may still experience emotions, but they are much less apparent than ordinary people.
Emotional blunting is clinically important since it significantly impairs the patient's quality of life (QoL). Dr. Wong reported that patients with emotional blunting tend to be indifferent towards all aspects of daily living, which thereby have a negative impact on their interpersonal relationships and social life. Moreover, these patients may evade from social interactions or ignore their responsibilities resulting in problems at work or school4.
Despite the significant consequences related to emotional blunting, identifying emotional blunting can be clinically challenging. Persistent sadness is considered a symptom of MDD, and some patients may perceive themselves cured of the condition if their sadness is relieved with treatment. However, Dr. Wong highlighted that the impact of emotional blunting can often be concealed when treating depressive symptoms. When considering emotional blunting as a residual symptom of MDD, some depressed patients experiencing numbing emotions may initially feel that they have recovered from the illness. But this may not be the case. In this regard, Dr. Wong stated that the persistent symptoms may induce chronic changes to the brain which further mediate systemic complications seen among these patients. Of note, emotional blunting may thereby contribute to non-adherence to treatment which may then lead to vicious cycle of symptoms and worsening of illness2.
To facilitate the identification of emotional blunting in MDD patients, Dr. Wong suggested that, during consultation, it is important to assess the severity of symptoms by asking patients about their social life and pleasurable moments. “Apart from questions related to sleeping quality and suicidal ideation, simple questions such as whether patient have seen a movie or gone shopping may reveal their emotion further. Patients who are experiencing emotional blunting may not elicit positive emotions,”he added.
Emotional blunting is often considered as a symptom of MDD in existing literature. For instance, a survey by Goodwin et al., (2017) reported a significant correlation between the severity of depressive symptoms on the Hospital Anxiety and Depression-Depression (HAD-D) scale and the blunting scale score (OQESA scores, r=0.521)5, suggesting emotional blunting may likely be a symptom of depression.
Contrary to this, some researchers consider emotional blunting as a side effect induced by conventional MDD therapy. Of interest, in a randomised controlled trial (RCT) by McCabe et al., (2010), 45 healthy individuals were randomly allocated to receive SSRI (citalopram), SNRI (reboxetine), or placebo for 7 days. At the end of drug treatment, the neural response to rewarding (sight and/or flavour of chocolate) and aversive stimuli (sight of mouldy strawberries and/or an unpleasant strawberry taste) was measured with functional magnetic resonance imaging (fMRI). The results showed that SSRIs may diminish the neural processing of both rewarding and aversive stimuli6. This may potentially provide an insight on how patients on SSRI treatment experience the emotional blunting. A study by Sansone et al., (2010) reported the relationship between emotional blunting and SSRI may indeed be dose-dependent since higher doses of SSRI may likely to precipitate emotional symptoms7.
More recently, an international cohort study involving 1,431 adult antidepressant users from 38 countries revealed that 66.1% of respondents on antidepressants reported experiencing emotional blunting8. These findings further highlighted the close association between emotional blunting and antidepressants.
Given the reported close association between emotional blunting and conventional MDD therapies, some academics advocate on reducing the dose of these offending antidepressant, which may then improve the emotional problems7. However, Dr. Wong questioned the necessity of using a high dose of antidepressants in first place and postulated that the intention of using high dose of antidepressant maybe due to the fact that there had been a suboptimal symptom control with a low dosage of antidepressant. In this regard, it creates a clinical dilemma on whether to treat MDD and risk the treatment effect on emotional blunting or compromise MDD treatment and avoid emotional blunting. Besides, Dr. Wong suggested that if the prescribed dosage of SSRI is already low, it would be impractical to further reduce the dosage. As highlighted, emotional blunting is possibly a residual symptom of MDD that requires special attention.
When managing MDD patients with emotional blunting, Dr. Wong advised that the clinical impact of emotional blunting on patients should be evaluated. He emphasised that it is crucial to determine whether the emotional blunting experienced by the patient is related to the prescribed antidepressant. “Provided that the depressive symptoms are adequately managed, reducing antidepressant dosage may be feasible to determine if the emotional blunting is related to the medication,” he noted. He further elaborated that the status of MDD recovery should be taken into consideration since certain symptoms of MDD require a longer treatment period.
Thanks to recent pharmacological advancement, more efficacious antidepressants with a better safety profile have been emerging. Vortioxetine is a multimodal antidepressant acting both as a serotonin modulator and stimulator. It selectively blocks serotonin re-uptake by inhibiting the serotonin transporter (SERT) in addition to directly modulate the activity of serotonin (5-HT) receptors9.
“SSRIs blocks the re-uptake of serotonin by inhibiting the serotonin transporter (SERT), thereby increasing serotonin availability. In contrast, the mechanism of action of vortioxetine is more than merely inhibiting the SERT. It also has a direct effect on a number of postsynaptic 5-HT receptors. These properties, in particular the modulation of 5-HT3 receptors and the downstream positive effect on dopamine, dampening the depressive symptoms while reducing emotional blunting,”Dr. Wong explained.
The clinical performance of vortioxetine in patients with MDD who experienced an inadequate treatment response to SSRI/SNRI monotherapy was evaluated in the COMPLETE trial by Fagiolini et al., (2021). In the trial, patients were switched to vortioxetine treatment for 8 weeks. Post-treatment, patients (N=143) reported improvement in Oxford Depression Questionnaire (ODQ) total score by -29.8 points (p<0.0001, Figure 1A) and emotional detachment (Figure 1B). 50% of patients reported no emotional blunting in response to the standardised screening question. Moreover, significant improvements in cognitive performance, motivation and energy level (Figure 2A-2C), and overall functioning were observed. 47% of patients were in remission at week 8. The study further substantiated that vortioxetine was safe and tolerable.
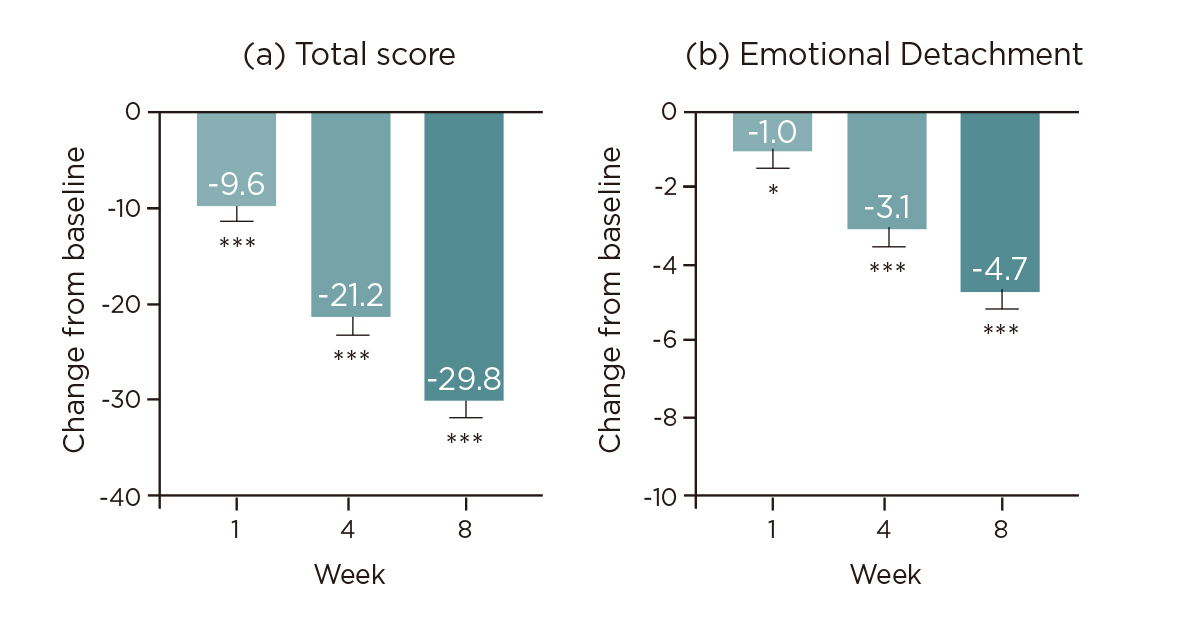
Figure 1. Changes from baseline in ODQ10, *p<0.05; ***p<0.0001
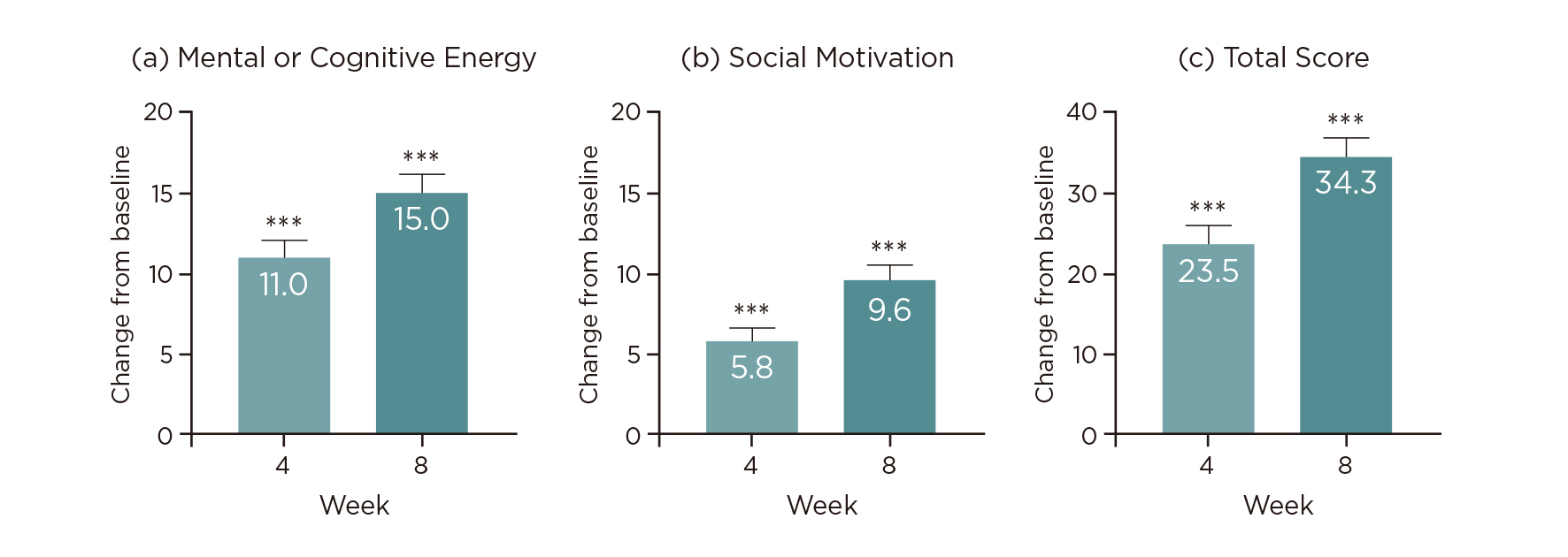
Figure 2. Changes from baseline in Motivation and Energy Inventory10, ***p<0.0001
Based on the pharmacology and the results of the COMPLETE trial, vortioxetine is likely the preferred treatment option in depression, particularly among patients with emotional blunting. Dr. Wong highlighted that when emotional blunting is related to the disorder of depression itself and not a result of antidepressant, vortioxetine could be considered as a treatment of choice.
To demonstrate the management of MDD and emotional blunting in clinical settings, Dr. Wong shared a case of a female patient in her 50s with depressive symptoms that were well-controlled by antidepressants. Nevertheless, the patient looked dull and lost interest in traveling, which she often did and enjoyed in the past. In addition, the patient had lost interest in playing mah-jong as well. Besides, the patient expressed no sadness when attending a funeral of her close relative. Summarising the observations, Dr. Wong believed she was experienced emotional blunting.
The patient was on paroxetine initially and was switched to vortioxetine gradually by Dr. Wong. After several weeks of treatment, the patient regained interest in her job and planned a trip with her husband. During the follow-up consultation, she told Dr. Wong that the trip was enjoyable and refreshing.
This case highlighted the effectiveness of vortioxetine in treating both emotional blunting and MDD without compromising either. Furthermore, Dr. Wong suggested switching to low dose of vortioxetine initially and then titrating it accordingly.
Dr. Wong emphasised that, apart from depressive symptoms, it is vital for clinicians to be aware of emotional blunting when evaluating patient recovering from depression. “Emotional blunting significantly hinders functional recovery,” he highlighted. He further added that it is essential to educate patients on emotional blunting and the importance of seeking appropriate attention and treatment. Dr. Wong suggested clinicians should explore the symptoms of emotional blunting by simply asking 2 questions during consultation. The first is whether the patient has some enjoyable moments or have experienced some unhappy events. Simply chatting with the patient about his work, hobbies or relation with others would be good enough. The second question is whether the patient has some planning or something to look forward to, for example, a vacation trip. These simple question or seemingly casual chats would be very useful in looking for evidence of emotional blunting and assess the functional recovery of the patient.
Based on the clinical trial and practical case shared by Dr. Wong, vortioxetine appeared to be promising in managing MDD patients with emotional blunting. Moreover, apart from the therapeutic benefits, vortioxetine has also shown to improve cognitive functions10. Last but not the least, Dr. Wong suggested that frontline healthcare professionals should also consider what other interventions can be applied to help the patients in addition to medication. “It is not necessarily formal treatment, such as cognitive behavioural therapy (CBT), but something simple that can be done in daily life. For instance, introducing emotional stimulation through music, massage, and even having food with strong tastes may have beneficial effects. The primary aim here is to allow the patients to regain the feeling of different emotions,” he mentioned. Essentially, a healthy lifestyle with adequate physical exercise is highly recommended for improving the overall physical and mental well-being, particularly among patients with depression.
References
1. Papalexi et al. BMC Psychiatry 2022; 22: 1–10. 2. Ma et al. Front Psychiatry 2021; 12: 2329. 3. Christensen et al. Ann Gen Psychiatry 2022; 21. DOI:10.1186/S12991-022-00387-1. 4. Christensen et al. Ann Gen Psychiatry 2022; 21: 1–12. 5. Goodwin et al. J Affect Disord 2017; 221: 31–5. 6. McCabe et al. Biol Psychiatry 2010; 67: 439–45. 7. Sansone et al. Psychiatry (Edgmont) 2010; 7: 14. 8. Read et al. Curr Drug Saf 2018; 13: 176–86. 9. Sowa-Kućma et al. Pharmacol Rep 2017; 69: 595–601. 10. Fagiolini et al. J Affect Disord 2021; 283: 472–9.





