
Venous thromboembolism (VTE) refers to the condition that a blood clot forms in a vein. The condition can be classified into deep-vein thrombosis (DVT), when a blood clot forms in a deep vein, pulmonary embolism (PE), when a clot breaks loose and travels through the bloodstream to the lungs, or a combination of both1. While DVT may trigger pain, erythema, tenderness, and swelling of the affected limb, PE often presents as sudden breathlessness with chest pain and could result in life-threatening conditions2. This highlights the vital role of VTE prophylaxis for high-risk populations. Notably, among the various mechanical compression methods developed for VTE prophylaxis, intermittent pneumatic compression (IPC) customising the prophylactic therapy based on the individual’s venous refill time is expected to optimise treatment outcomes.
Stasis of blood flow, endothelial injury, and hypercoagulability are the triad of thrombosis contributing to the pathogenesis of VTE3. Practically, obesity, smoking, hypertension, trauma, and particularly surgery are the major risk factors for the disease. Moreover, immobilisation associated with long periods of air travel and certain medical conditions, such as chronic obstructive pulmonary disease, will increase the risk of VTE as well1.
Apart from the pharmacological approach, mechanical prophylaxis by applying compression, which changes the pressure gradient in the compressed region, accelerating blood forward and facilitating venous emptying3, is also prescribed in clinical practice. Of note, conventional compression treatment utilises uniform compression, which generates the same compression cycle in all scenarios. Nonetheless, as the vasculature of patients is specific, the refill time of uniform compression may not match the pace of venous refill leading to incomplete vein evacuation and suboptimal hemodynamic effectiveness4.
In view of the limitation of the uniform compression approach, the IPC with vascular refill detection, which measures venous refill time and adjusts cycle times automatically, has been developed5. Briefly, the IPC device is equipped with a sensor capable of detecting the post-compression refilling of the calf veins and responding by initiating the subsequent cycle when these veins are full6. Thus, the compression cycles generated by the IPC device are personalised that can better match the patient’s venous refill and will be adjusted automatically according to the changes in the patient’s needs over time.
The hemodynamic impact of IPC device, uniform compression device, and posterior sequential rapid gradient inflation (PSR) device had been compared in a previous clinical trial by Griffin et al (2007) involving 12 patients with primary bilateral varicose veins. The results indicated that all three devices increased flow during compression by 2.5-3 times compared to the median baseline flow (p<0.0001). Remarkably, the total volume expelled per hour during compression by IPC device was 7,800ml, which was significantly higher than both uniform compression device (5,200ml, p<0.028) and PSR device (3,300ml, p<0.005, Figure 1)5. The high volume of blood moved by IPC device was due to the increased volume per cycle and more compression cycles over time. The findings thus confirmed the hemodynamic effectiveness of IPC device.
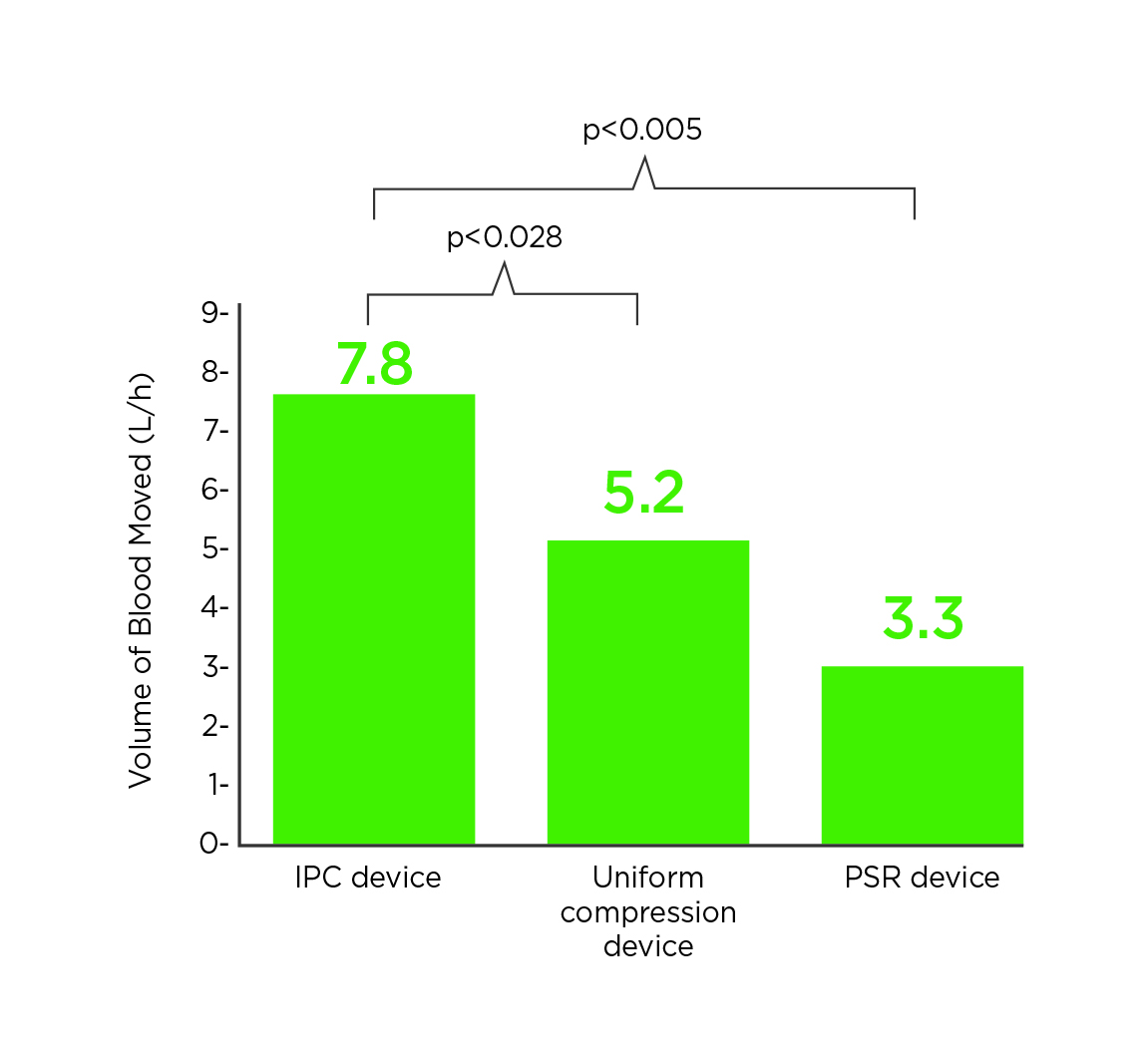
Figure 1. Total volume expelled per hour by various compression devices5
The clinical benefit of IPC device in reducing venous thrombosis was visualised in the CLOTS 3 trial by Dennis et al (2013), which involved 2,876 immobile patients from 94 centres who admitted to hospital within 3 days of acute stroke. The patients were randomly assigned to receive treatment with the IPC device (IPC group) or not receive it (control group). While all patients and investigators were aware of treatment allocation, the radiologist or technician doing the compression duplex ultrasound (CDU) of both legs were masked to treatment group. After 6 months of follow-up, DVT in the proximal veins occurred in 8.5% of patients in IPC group, and that in control group was 12.1%. The adjusted odds ratio (0.65, p = 0.001) for the primary outcome suggested that IPC treatment significantly reduce the risk of primary outcome, i.e. DVT in the proximal veins compared to control. Furthermore, the results indicated that IPC treatment yielded significantly lower risk of death than the control group during the study period (hazard ratio [HR]: 0.86, p = 0.042, Figure 2)7. Based on the results, IPC is an effective method of reducing the risk of DVT and improving survival in patients who are immobile after stroke.
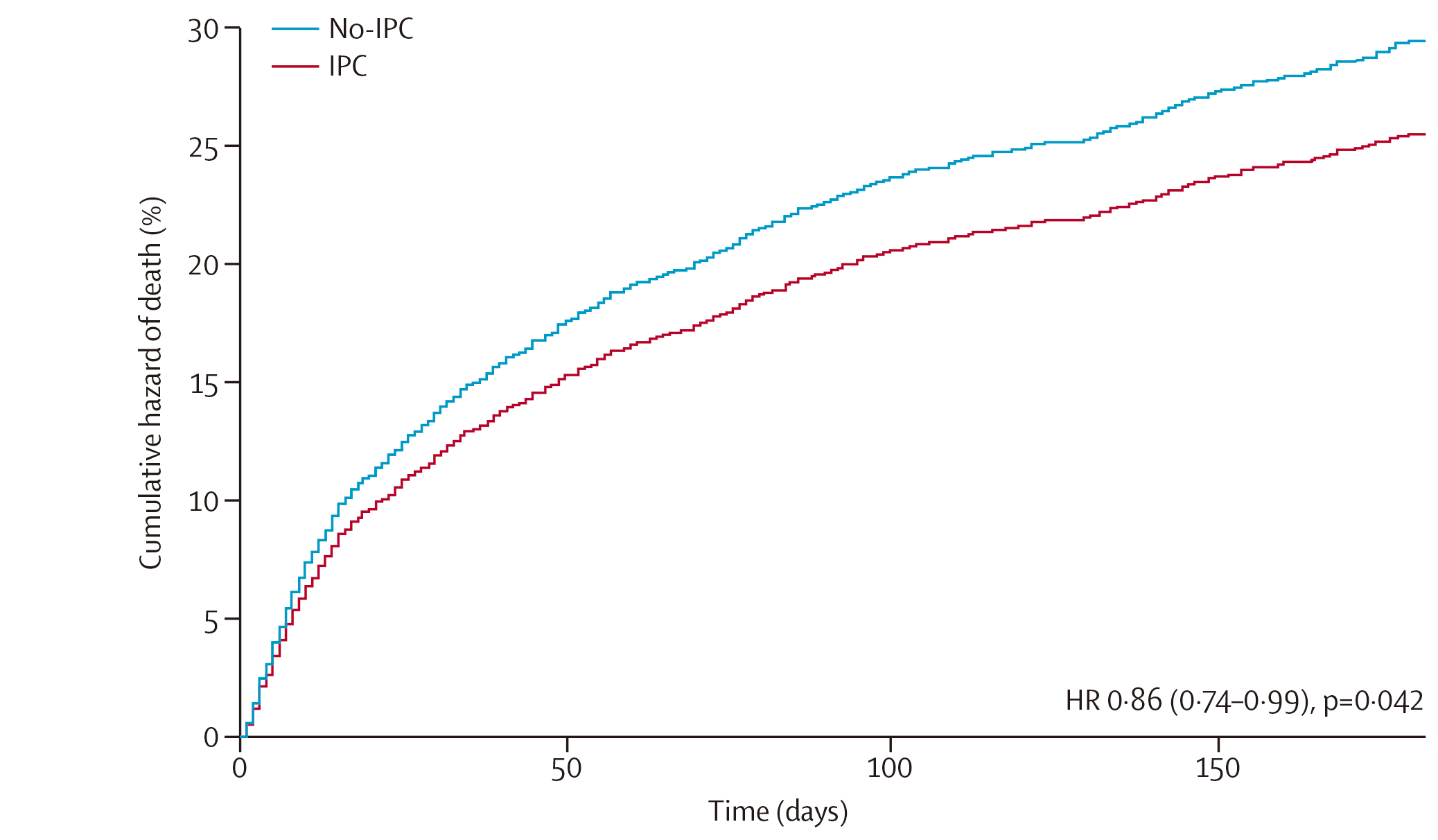
Figure 2. Cumulative hazard of death during the 6 months after randomisation in IPC and control groups7
In reality, both mechanical approach and pharmacologic agents, such as unfractionated heparin, low-molecular-weight heparin, and fondaparinux, are prescribed for prophylaxis of VTE. However, while pharmacologic agents effectively reduce VTE risk, their application in patients at increased bleeding risk is not recommended. For these patients, mechanical prophylaxis, preferably with IPC, is advocated over no prophylaxis until the risk of bleeding diminishes and pharmacologic prophylaxis may be initiated8.
Remarkably, previous investigations demonstrated that the combination of IPC and prophylactic anticoagulation, also referred to as pharmaco-mechanical modality, is more effective than the mechanical or pharmacological approaches alone. The recent systematic review by Kakkos et al (2022), which included 34 clinical trials, demonstrated that the addition of pharmacologic prophylaxis to IPC compared with IPC alone reduced the incidence of symptomatic PE from 1.34% (IPC group) to 0.65% (combined group). Besides, the incidence of DVT was 3.81% in the IPC group and 2.03% in the combined group. However, results suggested that the addition of pharmacologic prophylaxis to IPC increased the risk of any bleeding (5.88%) compared to IPC alone (0.95%)9. Thus, the results support the use of combined modalities in people at risk of developing VTE, provided the patients are not at high risk for major bleeding complications.
In summary, existing evidence confirms the enhanced hemodynamic effectiveness of IPC as compared to conventional compression approaches. Essentially, the improved functionality can be translated into clinical benefits on reduced the risk of VTE. As thrombosis is a multifactorial disease, optimised VTE prophylaxis is likely achieved in a multimodal approach. As stated, former trials have provided insight into the synergy of prophylaxis in reducing risk of VTE, which is recommended in clinical guidelines. Hence, further research on the effects of other potential combined treatments would likely facilitate the development of effective treatment strategies.
References
1. Goldhaber et al. Circulation 2002; 106: 1436–8. 2. Michota. Clin Cornerstone 2005; 7: 8–15. 3. Weinberger et al. Curr Trauma Reports 2016; 2: 35–41. 4. Kakkos et al. Int Angiol 2005; 24: 330–5. 5. Griffin et al. Int Angiol 2007; 26: 158–64. 6. Kakkos et al. J Vasc Surg 2001; 34: 915–22. 7. Dennis. Lancet 2013; 382: 516–24. 8. Gould et al. Chest 2012; 141: e227S-e277S. 9. Kakkos et al. Cochrane database Syst Rev 2022; 1. DOI:10.1002/14651858.CD005258.PUB4.





