

Clinical Assistant Professor
Department of Psychiatry
School of Clinical Medicine
The University of Hong Kong
Depression is one of the most common mental disorders globally. Given its high prevalence and adverse consequences, the disease burden of depression is significant1. While depression can affect people of all ages, the elderly are particularly vulnerable to the disorder. A local study reported that the prevalence of depression among community adults aged 65 or above was 14.8% for females and 10.2% for males2. Essentially, depression diagnosed after the age of 65, referred to as late-life depression (LLD), may present differently compared to depression in younger adults and thus may be underdiagnosed and undertreated. In a recent sharing, Dr. Cheng Pak Wing Calvin, Specialist in Psychiatry, discussed the clinical challenges related to LLD and highlighted the essence of managing the disorder.
The Hidden Mischief among Elderly
Compared to depression in younger adults, LLD increases personal suffering, caregiver burden, and the risks of hospitalisation, disability, mortality, etc1. Because of the atypical presentation, the diagnosis of LLD is clinically challenging and undertreatment is common3. “LLD differs from adult-onset depression in symptom presentation, causes and prognosis”, Dr. Cheng noted. Remarkably, he highlighted that patients with LLD often complain of somatic symptoms initially instead of the mood problems suffered. He speculated that some elderly patients might not be familiar with describing mood conditions. Thus, frontline physicians are reminded to be aware of the potential LLD in patients to prevent missing diagnoses and delay treatment.
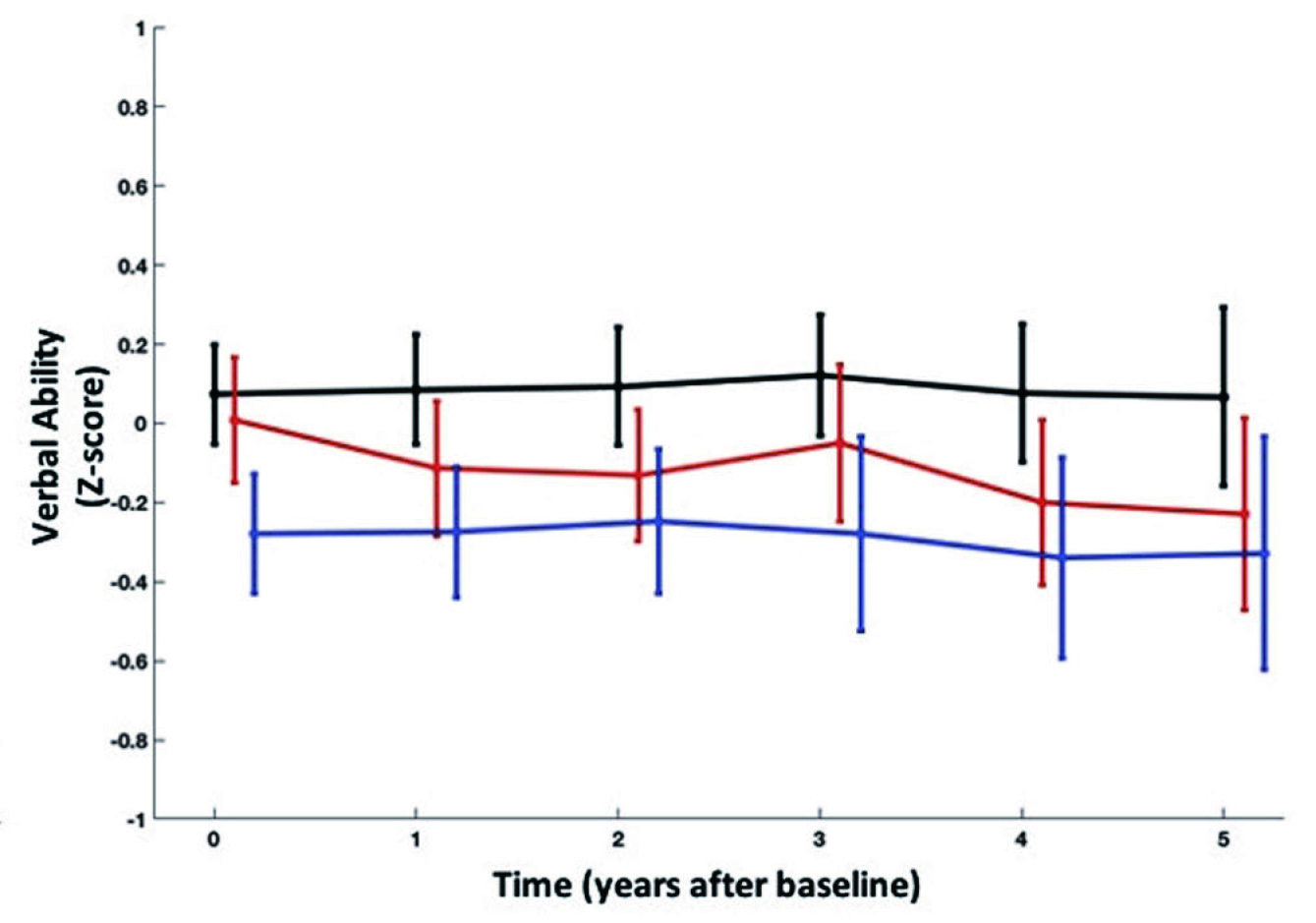
Patients with LLD commonly suffer from disability, functional decline, diminished quality of life and mortality from comorbid medical conditions4. Dr. Cheng pointed out that one of the main differences between depression in the elderly and younger adults is that patients with LLD are often complicated with cognitive impairment, which is less common among younger patients. Recently, a prospective study by Ly et al (2021) reported that LLD is associated with an increased risk of developing dementia, while late-onset depression may represent a more rapid decline in verbal skills and delayed memory (Figure 1A and 1B)5.
A
B
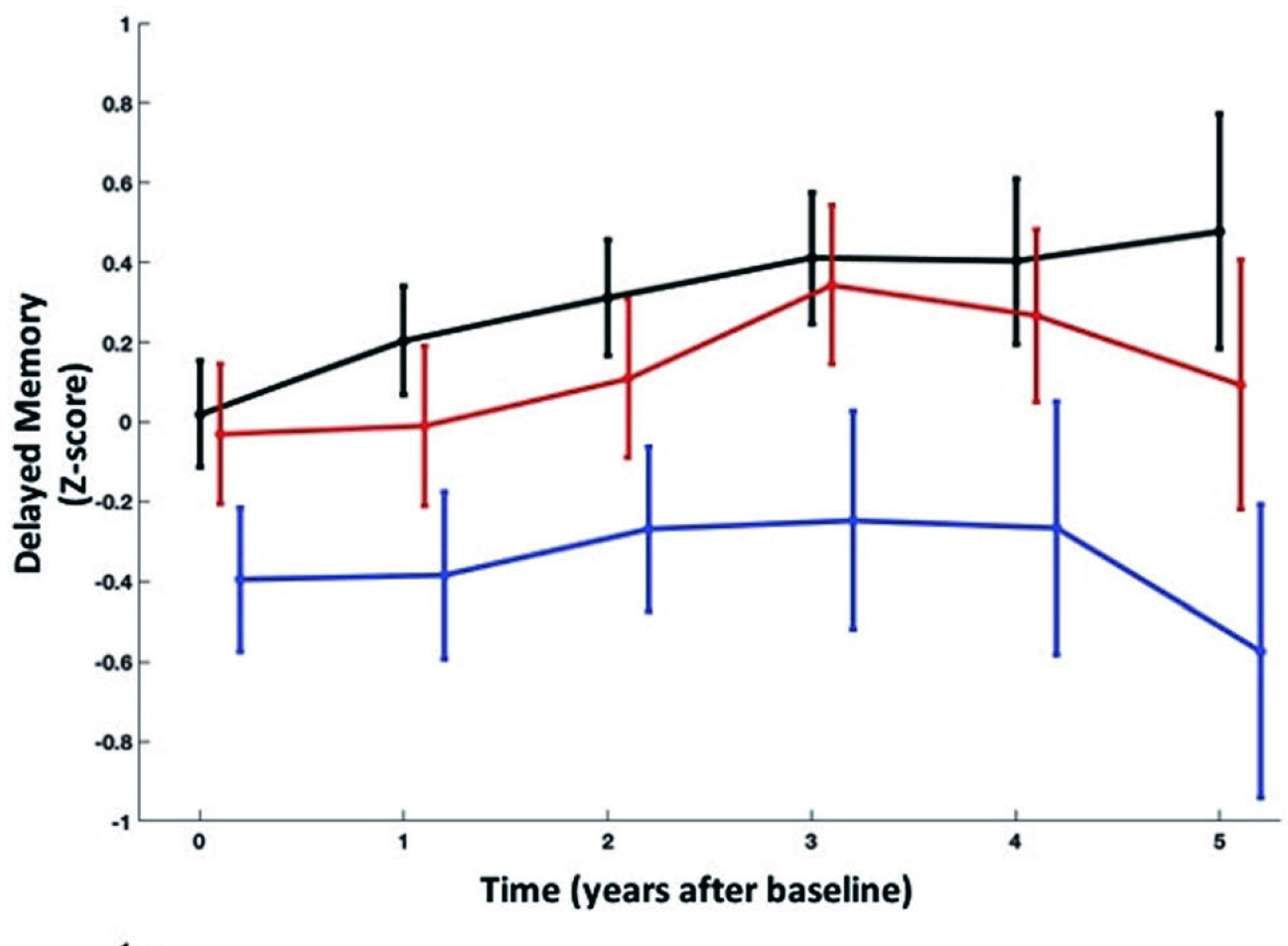
Figure 1. Changes in A) verbal ability and B) delayed memory in NDC, EOD, and LOD5, NDC: never-depressed control; EOD: early-onset depression; LOD: late-onset depression
In view of the pathophysiology of LLD, Dr. Cheng addressed the impact of pathological changes in the vasculature in the brain in LLD. For instance, elderly patients have a greater burden of white matter hyperintensities (WMH), which can be detected by computed tomography or magnetic resonance imaging. WMH has been reported to represent ischemic white matter damage in LLD and is associated with cognitive control dysfunction6. “The vascular complications would make depression more severe and more difficult to be treated compared to early-onset disease,” Dr. Cheng noted. He added that the long-term prognosis of LLD is worse with a higher risk of recurrence than depression in younger adults.
Dr. Cheng stated that the risk factors for depression in elderly would be different from those in younger patients. “Bereavement, such as the death of loved relatives, functional impairment, and physical illness, particularly pain, may trigger depressive episodes,” he said. Notably, loneliness and lack of life satisfaction have been suggested to be relevant risk factors for depression4. Furthermore, in addition to objective loneliness, Dr. Cheng emphasised that subjective loneliness in elderly patients is noteworthy.
LLD ¡V A Difficult but Treatable Disease
In managing LLD, it is essential to realise that many patients with LLD have substantial comorbidities, such as heart failure, diabetes, and cancer. Hence, Dr. Cheng advised that optimisation of medical conditions and selection of antidepressants concerning minimising drug-drug interactions (DDIs) is crucial. Of importance, the potential treatment-related adverse impacts on patients’ existing diseases, such as hypertension and diabetes, should be considered when selecting therapeutics. For instance, a large-scale retrospective cohort study by Mishima et al (2020) demonstrated that long-term antidepressant use would increase the risk of type 2 diabetes onset in a time- and dose-dependent manner7.
While cognitive impairment occurs in a significant proportion of the elderly, worsening patients’ cognitive function upon antidepressant treatment is a clinical concern. Sayyah et al (2016) reported that the use of selective serotonin reuptake inhibitors (SSRIs) in patients with depression could cause cognitive dysfunction in the acute phase of treatment8. Hence, Dr. Cheng advised evaluating whether the prescribed treatment would worsen the patient’s cognitive function. Besides, patients’ tolerability towards the prescribed therapy must be considered in managing LLD. “Some elderly patients may be more sensitive and thus not tolerate medications tolerable for other patients. Dose reduction would be needed in these cases,” Dr. Cheng noted.
Dr. Cheng expressed that elderly patients comply well with treatments in general. Nonetheless, medications with complicated dosing, such as requiring multiple doses per day, might risk missing doses and suboptimal adherence. Overall, Dr. Cheng commented that achieving complete recovery from LLD is challenging and prolonged treatment is often involved, whereas the rate of recurrence of LLD is relatively high. Notably, in order to comprehensively examine the treatment outcomes of antidepressants, Dr. Cheng recommended including specific depression-associated symptoms, such as improvement in emotional blunting and anhedonia, in the clinical evaluation in addition to the routine assessment of negative mood reduction.
A new generation of treatments against the Unmet Needs
In view of those difficulties mentioned above, the new generation of treatments for LLD may be the solution of the unmet needs. Dr. Cheng explained that the traditional antidepressants mainly target on SSRI or norepinephrine. However, the new generation of antidepressants also targeting on dopamine and glutamate, which possibly more effective to deal with the anhedonia aspects of LLD. Besides, multimodal antidepressants, such as vortioxetine, act on more than one receptor to produce treatment effects, including improvements in emotional, depressive symptoms and particularly cognitive dysfunction, which commonly existed in LLD. A former report suggested that multimodal antidepressants have shorter onset of therapeutic effects and improved tolerability9.
In reviewing the efficacy, Dr. Cheng commented that there is currently no single class of antidepressants that would outweigh the clinical benefit of other medications, regardless of elderly or younger patients. Remarkably, he added that, considering depression-associated symptoms, the new generation of antidepressants appear to offer treatment benefits against these symptoms. However, further clinical data are needed to confirm this observation.
With the advancement of technology, non-invasive brain stimulation (NIBS) becomes an alternative options. The most common forms of NIBS are repetitive transcranial magnetic stimulation (rTMS) with strong evidence supported. Another form of NIBS is transcranial direct current stimulation (tDCS), which may be used as augmentation therapy with the antidepressants. However, clinicians should aware of the limitations of NIBS, including the effect of cortical atrophy.
The Essential Component of Later Life ¡V Happiness But Not Depression
In summary, Dr. Cheng emphasised the interactions between cognitive impairment and depressive symptoms in the pathophysiology of LLD. Hence, the potential adverse cognitive impacts of antidepressants have to be considered in selecting treatment for patients with LLD. Antidepressants with cognitive benefits are thus preferred. On the other hand, as comorbidities are common among elderly patients, Dr. Cheng recommended that antidepressants with less risk of DDIs, better safety profile, and particularly low burden on kidney and liver should be considered.
The development of the new generation of treatments has provided a promising treatment option for managing LLD. The extra or multimodal mechanism of action of the medication or interventions facilitates the therapeutic effects and improved tolerability.
References
1. Bruce et al. Can J Psychiatry 2018; 63: 439–46. 2. Chi et al. Am J Geriatr Psychiatry 2005; 13: 409–16. 3. VanDamme et al. Int J Gen Med 2018; 11: 113–20. 4. Knöchel et al. Curr Neuropharmacol 2015; 13: 577. 5. Ly et al. Transl Psychiatry 2021 111 2021; 11: 1–10. 6. Respino et al. NeuroImage Clin 2019; 23: 101852. 7. Miidera et al. Diabetes Care 2020; 43: 885–93. 8. Sayyah et al. Psychiatry J 2016; 2016: 1–4. 9. Richelson. Int J Neuropsychopharmacol 2013; 16: 1433.
This work is supported by Lundbeck. The content of this material is based on the authors’ clinical experience and knowledge, and does not necessarily represent the official views of Lundbeck.





