

Department of Anaesthesia and Critical Care
University of Lorraine, France
Understanding Neuromuscular Blocking Management in Elderly
While multi-morbidity peaks in older patients and frailty, the chance of patients undergoing an array of surgical and non-surgical procedures with anaesthesia will increase as age advances. Notably, postoperative deaths have been reported to be the third most common cause of death globally in 20161. This highlights a major unmet need in the overall quality of care, particularly in elderly. To reduce the risk of possible complications in major surgical operations, neuromuscular blockade (NMB) is an essential component of general anesthesia. Nonetheless, in view of various confounding variables such as multiple comorbidities, managing NMB in elderly patients can be challenging. In a recent lecture, Prof. Thomas Fuchs-Buder outlined the potential risk of postoperative adverse outcomes in elderly and highlighted the key to optimise NMB by selecting the appropriate NMB agents and reversal agents.
Risk of Perioperative Adverse Outcomes in Elderly
Appropriate dosing, monitoring, and reversal strategy are essential in NMB for elderly patients since NMB agents undergo a significant degree of organ-dependent elimination while reduced organ function is common among elderly. Lee et al (2016) reported that the onset time of NMB agents is usually prolonged in the elderly irrespective of the drug used as compared to younger patients. Moreover, the use of higher doses (2–3 times the ED95 as their initial dose) of NMB agent in elderly patients were reported2.
Prof. Fuchs-Buder illustrated the increased risk of perioperative adverse outcomes in elderly based on a recent European prospective cohort study involving 9,497 patients aged 80 or older under anaesthesia. The results indicated the estimated 30-day all-cause mortality rate was 4.2%. The report further identified multi-morbidity, frailty, and limited mobility as the independent risk factors for the mortality outcome. Notably, anaesthesia technique, including general, regional, sedation, and combined, was not a significant risk factor for mortality. Of importance, the report highlighted the association between age and 30-day all-cause mortality that older patients were at higher risk of fatal outcome (Figure 1)3.
In addition to the independent risk factors stated above, postoperative pulmonary complications (PPCs) account for a substantial proportion of risk related to surgery and anesthesia and are a major cause of postoperative morbidity, mortality, and longer hospital stays. Hence, Prof. Fuchs-Buder presented the findings of a prospective cohort study including 2,464 surgical patients from 59 hospitals in Spain. The results identified advancing age was an independent risk factor for PPCs that an age over 80 was significantly associated with higher incidence of PPCs4.
Prolonged NMB Duration in Elderly
Given the increased risk of perioperative mortality and complications in elderly patients, optimised surgical conditions and tracheal intubation achieved by proper NMB agents are thus essential. Nonetheless, declined organ function is prevalent among elderly patients while the changes may influence the pharmacodynamics and pharmacokinetics of drugs administered during anaesthesia leading to great variation in onset time and duration of action of NMB agents.
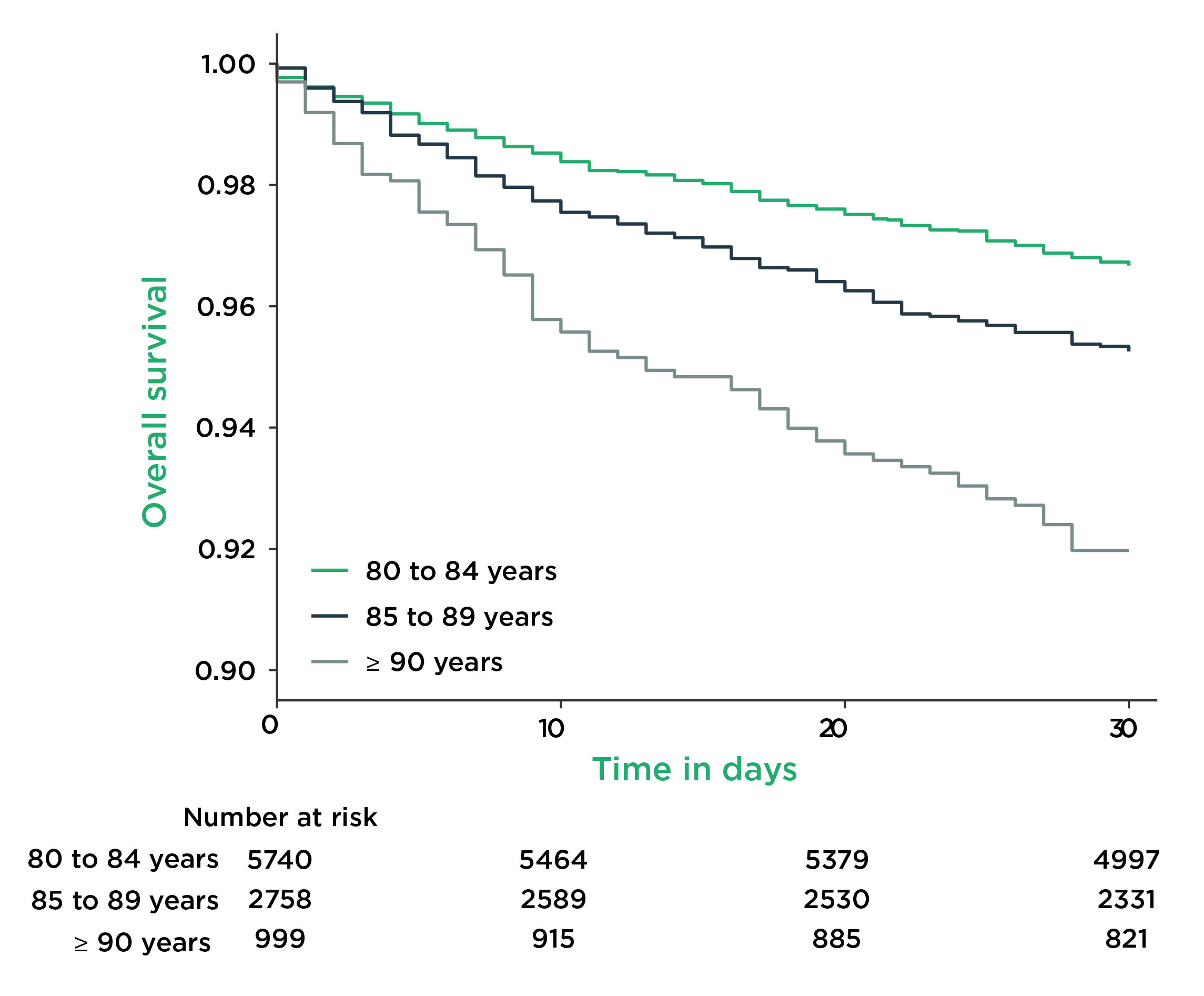
Figure 1. Overall survival (OS) of elderly patients under anaesthesia stratified by age3
The differences in pharmacodynamic response of rocuronium (0.6 mg/kg) between elderly (aged >80, n =16) and young patients (aged 18-40, n =16) was visualised in a prospective study by Bjerring et al (2020). The results showed a significant difference in onset time between young patients (mean =90 secs) and elderly (mean = 135 secs, p <0.001). Also, the average duration of action in elderly was significantly longer than that in young patients (81 mins vs 53 mins, p <0.001)5. Prof. Fuchs-Buder speculated that, in view of the prolonged duration of action of rocuronium, a higher incidence of residual paralysis may be expected among the elderly patients.
Prof. Fuchs-Buder presented the findings of a comparison on the time course of rocuronium NMB between patients aged 80 or older (n =16) with those aged under 50 (n =16). Similarly, significantly longer onset time (190 vs 123 secs, p <0.001) and duration of action (52 vs 36 mins, p <0.001) were observed in elderly patients as compared to young adults6. Of note, Prof. Fuchs-Buder highlighted that elderly patients had more comorbidities and a higher American Society of Anesthesiologists (ASA) score than the younger patients6. “The difference in ASA score may be explained by the significantly higher incidence of cardiovascular and renal comorbidities among the elderly patients” Prof. Fuchs-Buder commented.
Clinical Implications of Residual NMB in Elderly
Prof. Fuchs-Buder claimed that, as the duration of action of NMB agents is long and the recovery is slower in elderly, there is an increased risk of incomplete neuromuscular recovery at the end of surgery. A prospective study by Murphy et al (2015) reported that the incidence of postoperative residual NMB in elderly patients (mean age = 75, n = 149, 57.5%) was significantly higher than that in young patients (mean age = 38, n = 150, 30.0%, p <0.001), whereas severe postoperative residual NMB, defined as train-of-four (TOF) ratio <0.7, was observed in 16.8% of the elderly group and in 6.0% of the young group (p = 0.004)7.
In terms of clinical outcomes, 38.3% of elderly patients had episodes of oxygen saturation (SpO2) 90-94% in post-anaesthesia care unit (PACU), which was significantly higher than that in young patients (17.3%, p <0.001). The results further indicated that 15.4% of elderly patients had developed any pulmonary complication during hospitalisation, and that was only 2.0% among young patients (p <0.001)7. Importantly, the results demonstrated that the incidence of hypoxemic events was significantly higher in patients with residual NMB, in both elderly and young patient cohorts. Furthermore, signs and symptoms of muscle weakness in the PACU were observed more frequently in the elderly group compared with these in the younger group7.
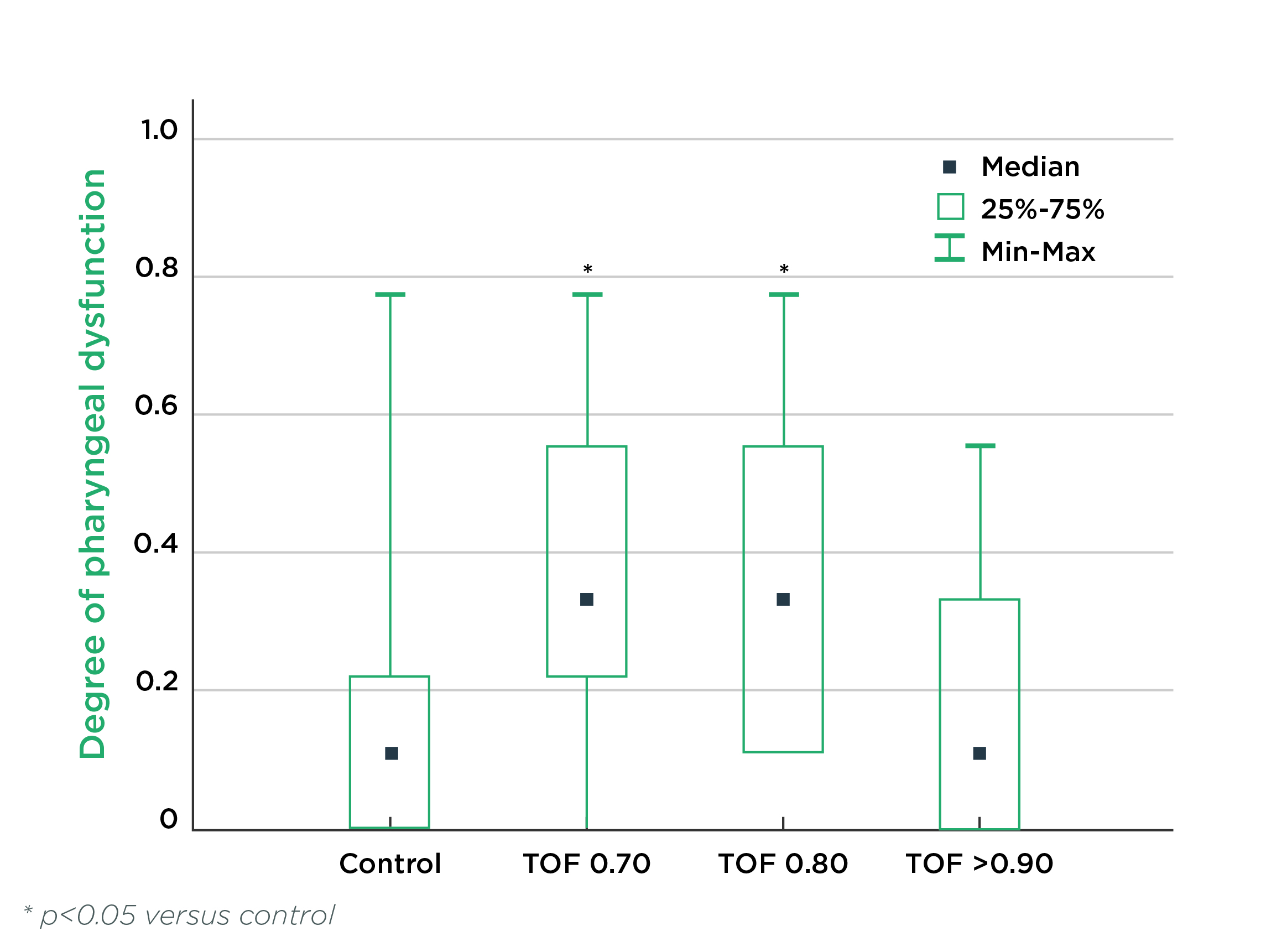
Figure 2. Degree of pharyngeal dysfunction at different levels of partial NMB8
Given that elderly have altered pharyngeal function which is associated with increased risk of aspiration, Cedborg et al (2014) evaluated the effects of partial NMB on pharyngeal function, coordination of breathing and swallowing, and airway protection in healthy individuals older than 65 years (n = 17). The results revealed that pharyngeal dysfunction increased significantly at TOF ratios 0.70 and 0.80 to 67% and 71%, respectively, compared with 37% at control recordings (n = 6, Figure 2), and swallowing showed a more severe degree of dysfunction during partial NMB8. The results complied with the illustration by Eikermann et al (2012) that minimal retroglossal upper airway diameter increased markedly during forced inspiration without NMB, whereas the increase was attenuated in partial NMB (Figure 3)9. These findings suggested that partial NMB would increase incidence of pharyngeal dysfunction and hence impair the ability to protect the airway.
Based on the findings on impacts of residual NMB, Prof. Fuchs- Buder emphasised that due NMB management, by careful dosing, monitoring, and reversal of NMB, is important in elderly to reduce the risk of residual NMB and the associated complications.
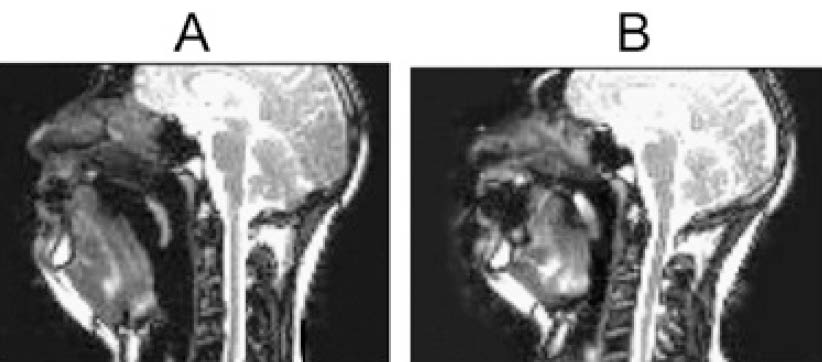
Figure 3. Minimum retroglossal upper airway diameter during forced inspiration (A) before NMB and (B) at TOF = 0.809
Reversal of NMB
Effective reversal of NMB is vital for reducing the risk of residual NMB, and hence postoperative morbidity and mortality in elderly persons. Nonetheless, physiologic aging is linked to a progressive decline in resting organ function leading to the altered pharmacokinetics and pharmacodynamics of many drugs, including neuromuscular blocking and reversal agents, in elderly.
Sugammadex is a modified cyclodextrin that antagonises aminosteroidal NMB agents (rocuronium and vecuronium) through encapsulation resulting in rapid reversal of NMB11. To evaluate the efficacy and safety of sugammadex in reversing rocuronium-induced NMB, McDonagh et al (2011) conducted a phase IIIa trial including 162 adult patients scheduled for surgery with general anesthesia and requiring NMB induced by rocuronium. The efficacy of sugammadex in recovering to TOF ratio to 0.9 or greater was examined10.
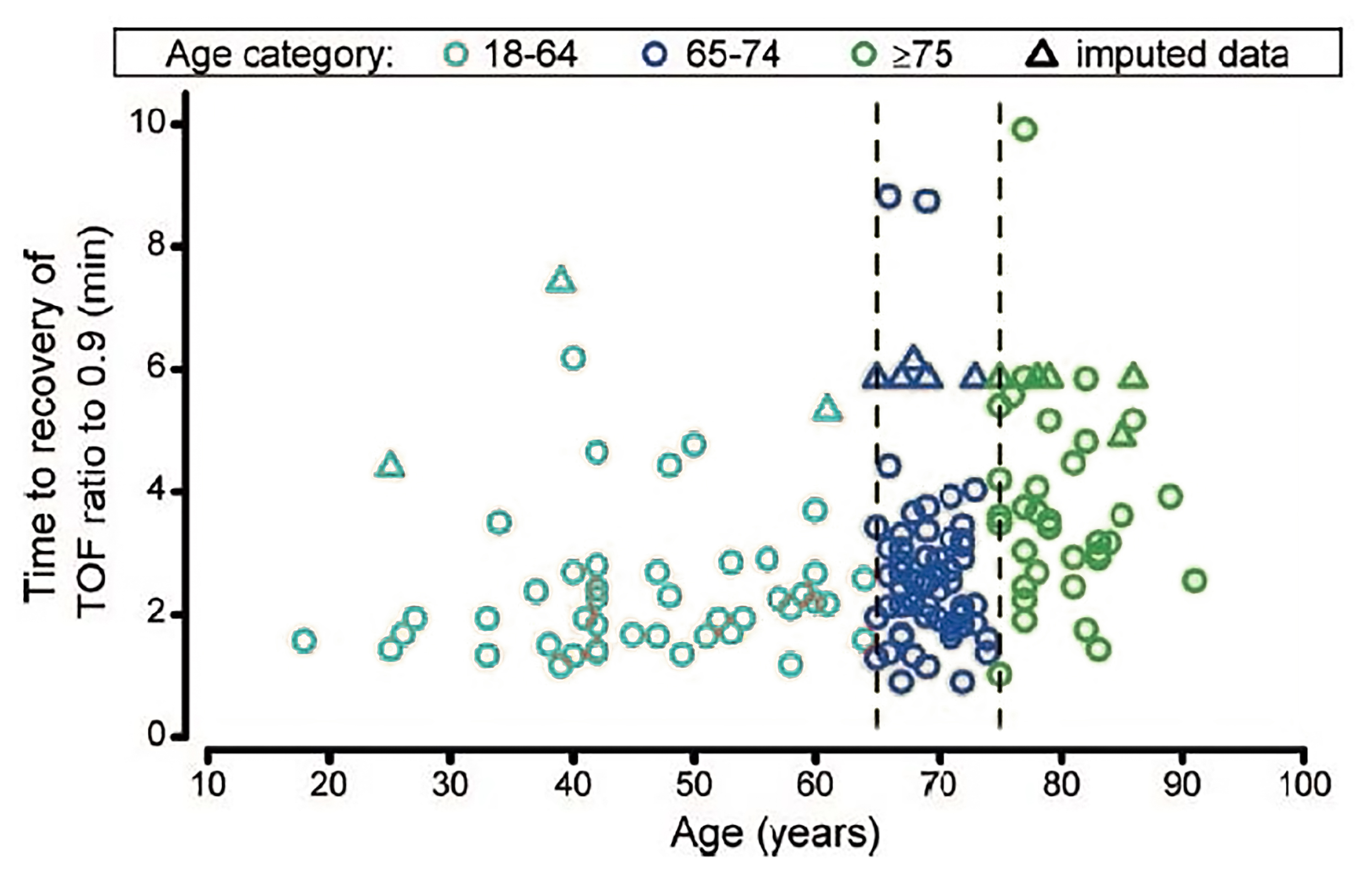
Figure 4. Individual patient recovery times to a TOF ratio of 0.910
The results reflected that the average time required to recover to TOF ratio to 0.9 for patients aged 18-64 was 2.1 minutes, whereas those for patients aged 65-74 and ≥75 were 2.4 minutes and 3.4 minutes, respectively (Figure 4). Significantly longer time was required for patients aged ≥65 to achieved TOF ratio to 0.9 by sugammadex (2.7 minutes) as compared to patients aged 18-64 (p = 0.017). The results also demonstrated that sugammadex was well tolerated by study participants10. Prof. Fuchs-Buder commented that, clinically, the reversal of NMB by sugammadex is extremely rapid and predictable in elderly, particularly in those aged ≥75. “This (reversal of NMB by sugammadex) is an efficient way to avoid residual paralyses in this age group (aged ≥65), in which the incidence of residual paralyses may be up to 50%. Their risk of developing postoperative pulmonary complications is high,” Prof. Fuchs-Buder expressed.
Summary
While NMB is needed to facilitate surgical procedures, Prof. Fuchs-Buder summarised that the duration of action of NMB agents would be increased in elderly patients, and hence residual paralyses and pulmonary complications are more frequent in these patients. In view of the rapid onset of rocuronium, it is a valid alternative for succinylcholine. Provided the rapid and predictive action demonstrated in patients of all age groups (aged 18 years or older) by sugammadex, Prof. Fuchs-Buder advocated sugammadex as the routine treatment for reversal of NMB in elderly patients.
References
1. Nepogodiev et al. Lancet 2019; 393: 401. 2. Lee et al. J Pain Res 2016; 9: 437-444. 3. POSE-study group. Eur J Anaesthesiol 2022; 39: 198–209. 4. Canet et al. Anesthesiology 2010; 113: 1338–50. 5. Bjerring et al. Acta Anaesthesiol Scand 2020; 64: 1082–8. 6. Schmartz et al. BMC Anesthesiol 2021; 21: 225. 7. Murphy et al. Anesthesiology 2015; 123: 1322–36. 8. Cedborg et al. Anesthesiology 2014; 120: 312–25. 9. Eikermann et al. Am J Respir Crit Care Med 2007; 175: 9–15. 10. McDonagh et al. Anesthesiology 2011; 114: 318–29. 11. BRIDION Hong Kong Product Circular.





