

Specialist in Nephrology
Preserving Kidney Health in Type 2 Diabetes Mellitus
Chronic kidney disease (CKD) is a common and serious complication of diabetes mellitus (DM)1. According to a recent report by the Hospital Authority, nearly 40% of DM patients are diagnosed with diabetic kidney disease whereas around 20% of DM patients are recognised as at the CKD stage of 3a or beyond2. Apart from adopting a healthy lifestyle, initiating a blood glucose-lowering agent as early as possible is the key to better management of the disease. The phase III EMPA-REG OUTCOME trial and recently the EMPEROR-Reduced trial have delivered remarkable messages about the renal benefits of using empagliflozin in DM patients with CKD. In this review, Dr. Ho Chung Ping shared his opinions on the renal benefits of empagliflozin, as well as offering some clinical advice in optimising the outcomes in the management of DM patients.
Early Blood Glucose Control as the Key to Preventing and Delaying Progression
DM is the leading cause of CKD worldwide. The Hong Kong Central Renal Registry reported that diabetic nephropathy (DN) accounts for nearly 50% of patients who undergo dialysis treatment in the Hospital Authority in Hong Kong1. “Compared with non-diabetic CKD patients, DM patients with CKD may suffer from more significant symptoms such as worsening of blood pressure control, frequent urination and proteinuria, etc., while their daily lives are also greatly affected. Most DM patients with CKD are not alerted at the early stages until disease progression or performing a medical check-up. To prevent or delay the progression of DM and CKD efficiently, initiating sodium-glucose cotransporter-2 (SGLT-2) inhibitor therapy as early as possible is strongly recommended,” highlighted Dr. Ho.
Lowered Incident or Worsening Nephropathy with Empagliflozin
Empagliflozin, an SGLT-2 inhibitor, is an emerging oral blood glucose-lowering medication available to minimise the risk of hyperglycaemia in patients with type 2 diabetes (T2D). By reducing sodium reabsorption in the proximal tubule, empagliflozin causes vasoconstriction of the afferent arterioles and reduction of renal glucose reabsorption, thereby increasing urinary glucose excretion3-5. “As the action of empagliflozin is independent of β-cell function and insulin secretion, it can also be used in patients with longstanding diabetes with acceptable renal function,” commented Dr. Ho.
Recently, enormous attention has been paid to the intriguing clinical findings of empagliflozin in the phase III, double-blind and randomised EMPA-REG OUTCOME study. In patients with T2D at high cardiovascular risk recruited in the EMPA-REG OUTCOME trial, the composite outcome of incident or worsening nephropathy was significantly lower in patients who received either 10 mg or 25 mg empagliflozin compared with placebo. Treatment with empagliflozin is associated with an approximately 40% reduction in the risk of macroalbuminuria progression, doubling of serum creatinine level, initiation of renal replacement therapy or death from renal disease (hazard ratio [HR], 0.61; 95% CI: 0.53-0.70; p<0.001) (Figure 1)5.
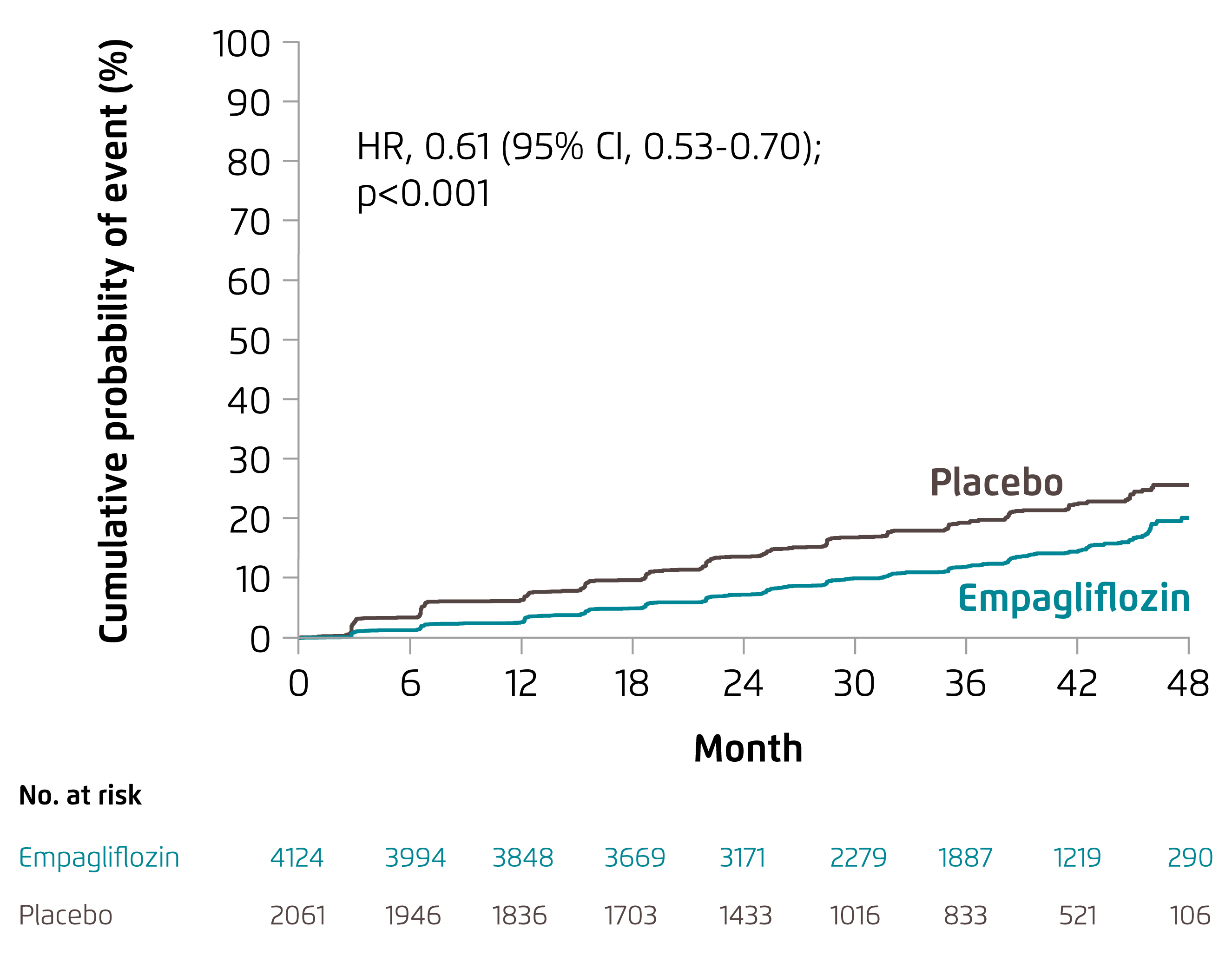
Figure 1. The probability of a first occurrence of a prespecified renal composite outcome of incident or worsening nephropathy5
“This glucose-lowering agent can reduce the surrogate markers of renal complications and lower the risk of clinically relevant renal events among patients with T2D at high risk of cardiovascular events. These results possibly offer an encouraging insight in extending the life expectancy of these patients by slowing down the worsening of kidney function,” emphasised Dr. Ho.
Consistent Renal Benefits regardless of the Presence or Absence of Diabetes with Empagliflozin
Apart from the EMPA-REG OUTCOME study, the renal benefits of empagliflozin were also demonstrated in the phase III EMPEROR-Reduced study. The double-blind, randomised and placebo-controlled trial, which recruited patients with chronic heart failure with reduced ejection fraction to receive 10 mg empagliflozin or placebo. Empagliflozin reduced the risk of composite renal endpoint, which is defined as the need for chronic dialysis, renal transplantation or a sustained reduction in estimated glomerular filtration rate, by 47% in patients with diabetes (HR, 0.53; 95% CI: 0.31-0.90) and by 58% in patients without diabetes (HR, 0.42; 95% CI: 0.19-0.97), with no significant treatment-by-diabetes interaction (p=0.65) (Figure 2)6. The analysis of the EMPEROR-Reduced study has revealed that treatment with empagliflozin can significantly slow down renal function decline regardless of patients’ diabetic condition, suggesting that empagliflozin may help in delaying kidney progression and preventing serious adverse renal events6.
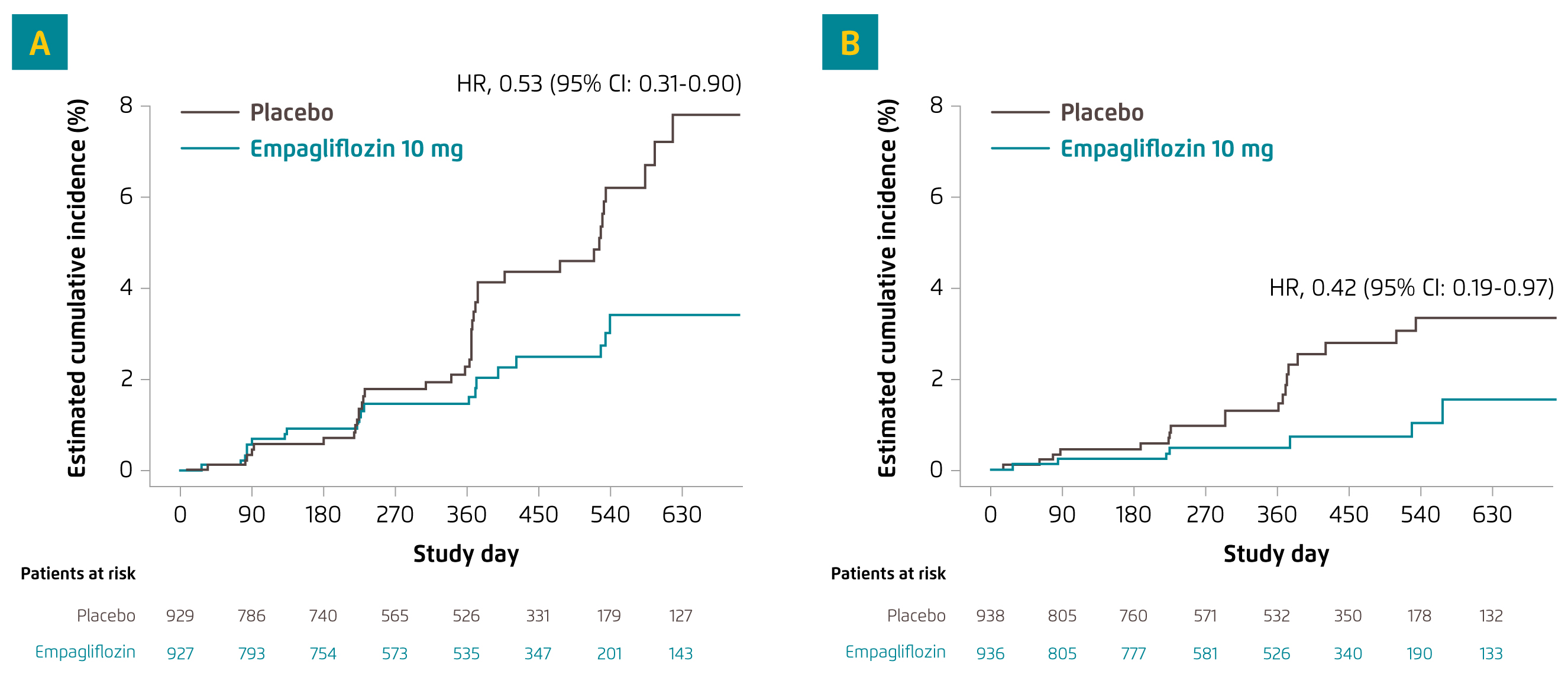
Figure 2. Effect of empagliflozin on renal composite end point in (A) patients with diabetes and (B) patients without diabetes6
“Although the risk of genital tract infections is higher among vulnerable patients who received empagliflozin, the overall tolerability and safety of the treatment with empagliflozin were generally similar between the empagliflozin group and the placebo group in both trials. It is noteworthy that, beyond glycaemia, urinary glucose excretion may be beneficial to obese T2D patients as the use of empagliflozin helps in losing body weight, reducing waist circumferences and lowering the indices of total and visceral adiposity. With the favourable impacts being derived from the use of empagliflozin, the risk of developing other complications due to obesity can be minimised in these patients,” added Dr. Ho.
Optimising Outcomes in Patients with DN
“Throughout the treatment course, certain challenges and difficulties may be faced in achieving optimal treatment outcomes. Despite the fact that early intervention using empagliflozin to regulate the glycaemic level is the key to preserving kidney function in diabetic patients, they may neglect the importance of lifestyle modifications. For instance, patients should exercise regularly to maintain a healthy weight and adopt a balanced diet by paying more attention to nutrition. For DM patients with CKD who are unwilling or not ready to start insulin injection but require additional glucose-lowering strategy, oral administration of empagliflozin may be a potential substitution for them,” stressed Dr. Ho. Other than lifestyle changes, Dr. Ho also advised the general public to undergo regular medical check-ups such as performing blood tests or urine tests to closely monitor glycaemic levels and renal functions. Early detection of abnormalities and early diagnosis are crucial for better management of the disease.
Given the valuable findings on the renal effectiveness and benefits, empagliflozin is rapidly establishing its role in the treatment of CKD in diabetic patients. It exhibits nephroprotective effects not only through improving glycaemic control, but also through exerting glucose-independent effects, including blood pressure-lowering and direct renal effects. Along with the improvements in other clinical outcomes, empagliflozin can potentially serve as a widely accepted glucose-lowering option to manage diabetic kidney disease and thus relieve the healthcare burden in the future.
References
1. The Integrated Dialysis Facilities (HK) Ltd. Resources for Professionals. Available at: https://www.dialysis.com.hk/en/resources-for-professionals/ (Accessed on 19 July 2021). 2. Quality Assurance Sub-committee of Central Committee on Diabetic Service HOSPITAL AUTHORITY. Hospital Authority Diabetes Mellitus Care Report 2019/20. 3. Hsia DS, et al. An update on sodium-glucose co-transporter-2 inhibitors for the treatment of diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2017;24(1):73-79. 4. Fioretto P, et al. SGLT2 Inhibitors and the Diabetic Kidney. Diabetes Care. 2016;39 Suppl 2:S165-S171. 5. Wanner Ch, Inzucchi SE, Zinman B. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. N Engl J Med. 2016;375(18):1801-1802.6. Anker SD, et al. Effect of Empagliflozin on Cardiovascular and Renal Outcomes in Patients With Heart Failure by Baseline Diabetes Status: Results From the EMPEROR-Reduced Trial. Circulation. 2021;143(4):337-349.





