

Specialist in Dermatology
Persistence and Endurance to Overcome the Hurdles
Keys to Achieve in the Marathon of Atopic Dermatitis Management
Itchiness is the hallmark of atopic dermatitis1. In Hong Kong, one in five people suffers from atopic dermatitis at different stages of life, with symptoms like extensive dryness, redness and swelling2. Apart from physical discomfort that can disrupt their sleeping quality, these patients usually have low self-esteem and lack confidence due to discrimination3. To better manage the symptoms of atopic dermatitis, tailored treatments should be given. Reassuring and educating patients about myths in atopic disease management are essential to improve patients’ compliance as well. Dr. Johnny Chan shared the treatment options for atopic dermatitis and highlighted the potential reasons for treatment non-adherence as well as the strategies to improve treatment adherence in patients with atopic dermatitis.
Why Atopic Dermatitis Matters?
The morphology of atopic dermatitis varies among individuals, which is mainly characterised by ill-defined erythematous patches scattering around joints and extremities with intense pruritus1. Frequent scratching of patches might predispose the patients to secondary bacterial infections, mostly by Staphylococcus aureus, which in turn intensify the symptoms with redness, swelling and oozing2,4. Individuals with either a family history of atopic dermatitis or innate defection in the immune system are prone to develop the disease. Their situations can further be triggered and aggravated by exposure to allergens such as food and atmospheric particles, psychological stress, environmental and immunological changes4,5.
“Apart from physical discomfort, psychological stress, embarrassment, social discrimination and daily activities limitation can affect patients’ psychosocial and quality of life significantly. In addition, frequent scratching resulted from itchiness during sleeping severely disrupts their sleeping quality,” highlighted Dr. Chan.
Seek Out Appropriate Treatments for Atopic Dermatitis
“To ensure the treatment can effectively control the symptoms, it is crucial that dermatologists are able to fully recognise the cause and severity of atopic dermatitis before prescription,” emphasised Dr. Chan.
He further explained that a therapeutic ladder, which involves various strengths of therapies, can be considered depending on patients’ clinical scenarios (Table 1). Instead of pharmaceutical treatment, emollient application and lifestyle changes such as identifying possible allergens are recommended in the management of mild atopic dermatitis6,7.
Table 1. Treatments for Atopic Dermatitis in Different Severities
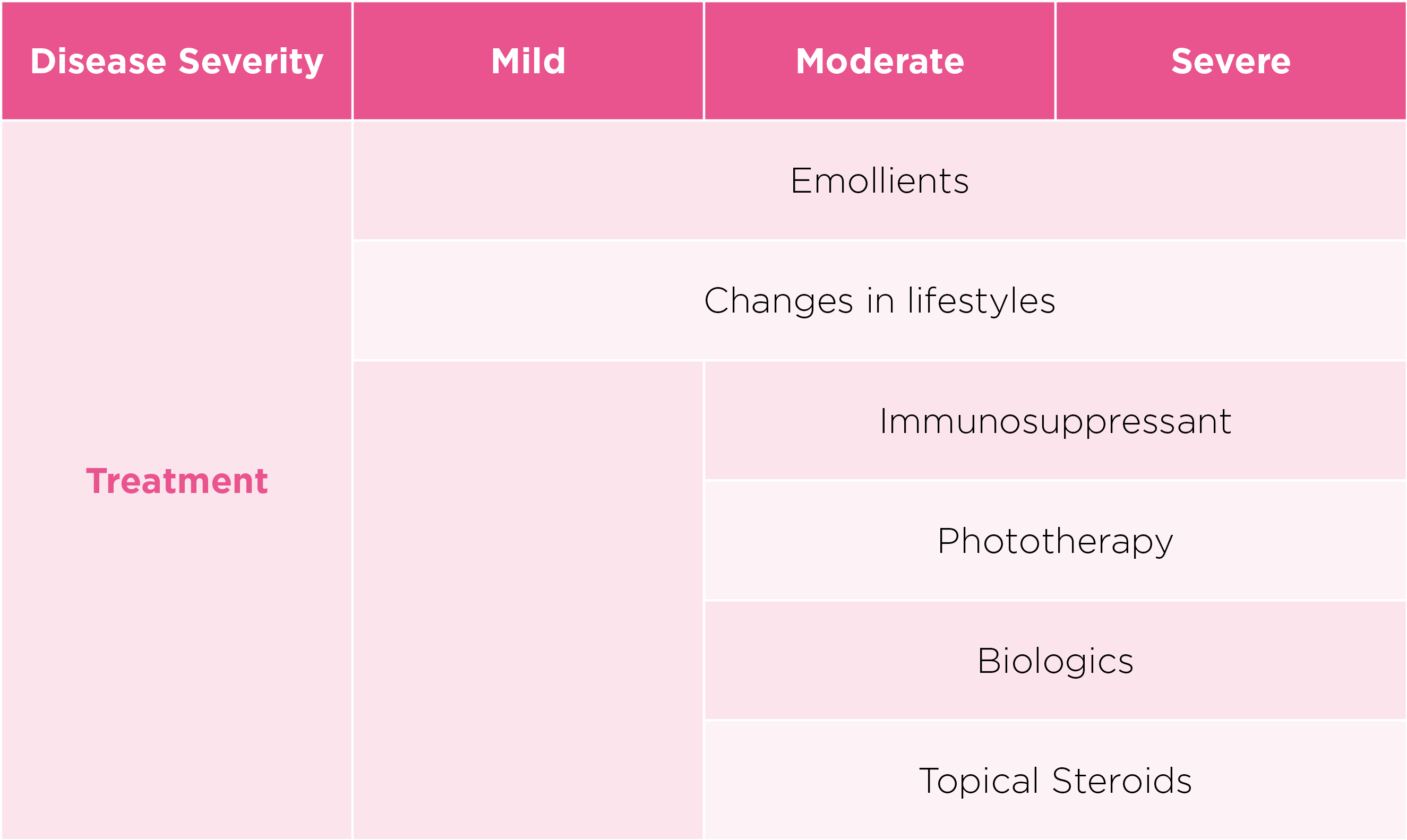
Pharmaceutical approaches are recommended if non-medication approach alone may be insufficient. Topical medications, which typically include different strengths of steroids, are prescribed based on patients’ conditions7. Topical steroids with low potency or diluted preparations are prescribed to manage mild lesions or applications over large areas, whereas stronger steroids are considered to be short-term use over areas with severe involvement7. Non-steroidal topical medications, on the other hand, are available for the face and areas with thinner skin7.
Dr. Chan also highlighted that systemic modalities can be considered as a second-line intervention to attain significant disease control when clinical manifestation become moderate-to-severe. Oral immunosuppressants, which can regulate the abnormal immune system systemically by acting on non-specific inhibition of T-cells and/or B cells, can be prescribed. Examples of immunosuppressive agents include methotrexate, cyclosporine and azathioprine. Although there are concerns about infective complications due to profound immunosuppression, regular conduction of blood tests helps monitoring renal and liver functions based on the drug-related side effect profile8.
Phototherapy, another skin treatment harnessing the power of ultraviolet A or B, improves the conditions in patients with moderate-to-severe skin by suppressing the over-active immune system of the skin. Despite complaints about the limited accessibilities to facilities and time constraints, its skin-restricted diffusion ability ensure the safety of patients in general8.
With a better understanding of the pathophysiology of atopic dermatitis, biologic drugs emerge. They are treatments designed to block interleukins that tend to trigger inflammatory conditions. By specifically blocking the interleukins from binding to the receptors, biologic drugs curb the over-active immune system alleviate the symptoms of atopic dermatitis9.
Strategies to Stay Committed
Although there are increasing numbers of treatment options available and patients’ quality of life has dramatically disturbed, patients are still relatively vulnerable to medication non-compliance issues10. “Lacking motivation, poor time management skills and requirement of frequent medication deter patients from taking medication as prescribed. For patients with corticosteroid phobia, the fear of potential adverse effects such as thinning of the skin caused by prolonged use of steroids further discourages them to comply with treatment,” mentioned Dr. Chan.
As emollients are always regarded as the backbone of management, choosing appropriate emollients plays a crucial role during the management marathon. A right emollient, not only can alleviate patients’ conditions with the minimised chances of corticosteroids uses, but also can improve patients’ compliance11. “Since trans-epidermal water loss is significantly high in patients with atopic dermatitis, regular moisturisation helps in preventing water loss. Moisturisers can mainly be divided into three categories based on their functions. Humectants extract water from the environment whereas occlusives reduce water evaporation by exerting their barrier functions. Emollients containing dermal reconstructive ingredients, like ceramides tend to reserve water on the skin. Moisturisers designed with long-lasting feature, fresh and non-sticky texture is well-tolerated in patients,” explained Dr. Chan.
Doctors often have insufficient time to educate patients and their caregivers about the correct application of the treatment, which can adversely affect patients’ compliance. Dr. Chan commented that comprehensive explanation of disease management is essential as information on the internet can be misleading and raise the patient’s feeling of uncertainty. Before starting the treatment, doctors should reinforce the appropriate use and safety of disease management. Telling patients about what will happen during the therapy, sharing them with other similar clinical cases and when to seek the physician are measures to improve patients’ adherence.
Your Extra Actions Lead You to Achieve Better
Medications, skin care, lifestyle changes and allergens avoiding are necessary. However, patients should not neglect the importance of maintaining good hygiene practices as the cornerstone in the management journey. For instance, using an allergen-proof bed and pillow covers while washing bedding regularly can prevent the allergens from closely contacting your body. Regularly cleaning your home with diluted household bleach can keep dust and mold away and minimise the risk of sensitisation12. With no curable therapies available nowadays and the possibilities of recurrence, a holistic approach regarding long-term management of the skin is vital.
References
1. Siegfried EC and Hebert AA. J Clin Med. 2015;4:884-917. 2. The Hong Kong Allergy Association. Eczema. 2020. Available at: https://www.allergyhk.org/?page_id=317 (Access on 3 November 2020). 3. National Eczema Association. Students with Eczema Have Lowered Self-Esteem Due to Bullying. Available at: https://nationaleczema.org/students-with-eczema-have-lowered-self-esteem-due-to-bullying/ (Access on 3 November 2020). 4. National Eczema Association. Atopic Dermatitis. 2020. Available at: https://nationaleczema.org/eczema/types-of-eczema/atopic-dermatitis/ (Access on 3 November 2020). 5. Yeung CK and Chan HHL. HK J Paediatr 2007;12:270-282. 6. National Eczema Association. Eczema Treatments. 2020. Available at: https://nationaleczema.org/eczema/treatment/ (Access on 3 November 2020). 7. HKSH Healthcare. Eczema. Available at: https://www.hksh-healthcare.com/en/clinical-services/dermatology-centre/eczema.php (Access on 3 November 2020). 8. Tsuyuki RT, et al. Can Pharm J. 2017;150:285-297. 9. National Eczema Association. Dupixent for Atopic Dermatitis FAQ. Available at: https://nationaleczema.org/eczema/treatment/dupixent/dupixent-faq/ (Access on 3 November 2020). 10. Arkwright PD, et al. J Allergy Clin Immunol: In Practice. 2013;1:142-51 11. Galli E et al. Italian Journal of Pediatrics. 2016;42:26 12. Allergy UK. 2020. Available at: https://www.allergyuk.org/about/latest-news/1181-keeping-it-clean-between-the-sheets (Accessed on 9 November 2020).





