
Specialist in Gastroenterology and Hepatology,
Honorary Secretary of The Hong Kong Association for the Study of Liver Diseases (HKASLD)
HCV Micro-elimination in Hong Kong,
Insights from AASLD the Liver Meeting
To deliver treatment and prevention intervention more efficiently using tailored methods, the European Association for the Study of Liver’s International Liver Foundation suggested setting up micro-elimination of hepatitis C virus (HCV) by breaking down national elimination goal into smaller goals for individual population segments in 20171. While the goal for Hong Kong is to reduce transmission of viral hepatitis and morbidity and mortality due to viral hepatitis, constant effort to keep strategies in pace is of paramount importance2. Recently, the American Association for the Study of Liver Diseases (AASLD) has delivered study highlights in the Liver Meeting 2020 which provide valuable insights into HCV elimination for Hong Kong.
“The current progress of HCV elimination in Hong Kong is a bit left behind, yet latest strategies and policy have loosen access criteria for Direct-Acting Antiviral (DAA) therapies, making it possible for Hong Kong to catch up with other countries by 2030,” said Prof. Grace Lai Hung Wong, Specialist in Gastroenterology and Hepatology and Honorary Secretary of The Hong Kong Association for the Study of Liver Diseases (HKASLD). In Hong Kong, viraemic HCV infection prevalence is 0.3%, according to a latest territory-wide epidemiological study2. However, a modelling study has revealed that diagnosis rate was merely 22% and treatment coverage rate of those diagnosed was 6% only2, suggesting that access to HCV treatment has remained limited. Since injecting drugs is the known major route of transmission in Hong Kong2, identifying barriers to test and treat people who inject drugs (PWIDs) and simplifying service delivery are ways to step forward.
Lesson to Learn from AASLD Highlights
Studies presented in AASLD covered themes including the efficacy and safety of DAA therapies, examples of successful streamlined patient journey by tailored test-to-treatment strategies, and the impacts of COVID-19 to HCV elimination action worldwide.
Steady DAA therapies Efficacy and Safety
Newest data presented have further ascertained the efficacy and safety of DAA therapies. Glecaprevir/Pibrentasvir (G/P) therapy has been effective and well-tolerated in different populations, with sustained virologic response after 12 weeks of treatment (SVR12) of 97.7% (modified ITT [mITT], n/N=256/262, retrospective observational cohort study) in Korean patients3, 99.3% (mITT, n/N=133/134, integrated analysis) and 99.4% (mITT, n/N=1085/1092, integrated analysis) in Hispanic/Latino and non-Hispanic/Latino patients respectively who are treatment naïve4, 97.0% (n/N=357/368, real-world analysis) in patients with substance abuse disorders (Figure 1) 5, and 96.5% (n/N=547/567, real-world analysis) in PWIDs with varies of comorbidities6. Besides, SVR12 of 100% were achieved in homeless patients treated by Sofosbuvir/Velpatasvir therapy (n/N=122/122, real-world analysis)7 and adolescents treated by Sofosbuvir/Velpatasvir/Voxilaprevir therapy (n/N=21/21, open-label study)8.
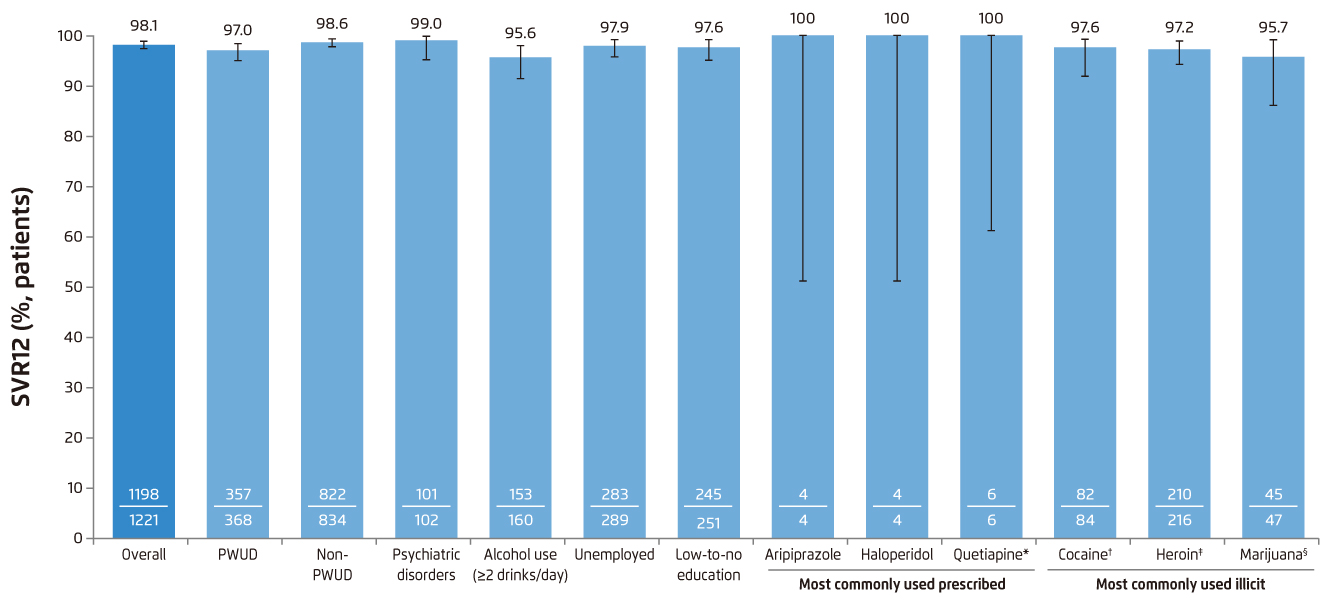
Figure 1. SVR12 rates of 8-week G/P treatment overall and by subgroups of interest in the core population with sufficient follow-up5
Recently, the HKSAR Government has released an action plan for viral hepatitis, which stated a further expansion of DAA and was aimed at all patients diagnosed with HCV infection regardless of their degree of fibrosis. “Resource has been allocated for hepatologist to prescribe DAA therapy to patients diagnosed with HCV soon after the announcement. While DAA therapies is central to HCV elimination, long waiting time for medication is the bottleneck and we have to find out some way to streamline service provision and simplify cascade of care, “ commented Prof. Wong. Result of studies from Italy and New Zealand have also demonstrated the importance of short-duration therapy to reduce healthcare resource burden and increase treatment capacity9, as well as to strengthen cascade of care to enhance diagnosis and treatment uptake10.
Streamline Patient Journey with Tailored Test-to-Treatment Strategies
Taking reference from strategies used in other countries, a study from Philadelphia has compared navigation model (NM) with embedded treatment model (ETM) which embedded HCV treatment within a substance use disorder treatment programme. Significant increases in treatment initiation rate (NM: 26%, n=8 vs. ETM: 75%, n=55; p<0.0001) and treatment completion rate (NM: 16%, n=5 vs. ETM: 58%, n=42; p<0.0001) have been reported11. Another study from London which adopted opt-out testing model in primary care homeless centre has shown a 90.3% testing uptake rate, of which 46.5% of those had treated or started therapy12, giving support to the efficacy of opt-out testing and the importance of streamlined care cascade to reduce loss to follow up. Other strategies such as using HCV model in homeless shelters have also been presented13.
Looking back to the situation in Hong Kong, the Center for Liver Health of the Chinese University of Hong Kong has collaborated with a non-government organisation to launch a liver programme since 2009. It provides HCV screening and education to high-risk populations and serves as the cornerstone of HCV elimination in Hong Kong. “The expanded access to DAA therapies has opened a new chapter to HCV elimination in Hong Kong. What to do next is to decentralise HCV management by incorporating fast-track clinic and well-trained hepatitis nurse who can penetrate into the communities,” shared Prof. Wong.
Impacts of COVID-19 to HCV Elimination Action
While COVID-19 epidemic is damaging the world’s economy as well as human activities, its impact on HCV elimination is another concern. Several studies presented have highlighted its retrograde impacts, including fewer treatment referral and treatment initiation, and more lost-to-follow-up case during the epidemic (8%, n/N=6/75 during COVID-19 vs. 5%, n/N=7/149 one year prior to COVID-19)14. However, the situation is better in Hong Kong. “Most patients adhere to treatment schedule because they have been waiting for about two years to be medicated. In addition, the high efficacy, good safety profile and short treatment duration of DAA therapy have made treatment easier to complete than ever,” said Prof. Wong.
Surmount All Difficulties to Reach the Goal
Although there are existing barriers and new challenges due to current strike of epidemic, HCV micro-elimination is always a mission to achieve. Increased involvement and collaboration of different stakeholders, as well as training and education to decentralise HCV management in community level should be helpful.
References:
1. Lazarus JV, et al. J Hepatol. 2017;67:665-666. 2. Department of Health, et al. Hong Kong Viral Hepatitis Action Plan. 2020-2014. 3. Park YJ, et al. AASLD Abstract no. 887. Hepatology. 2020;72:543A-544A. 4. Gutlerrez JA, et al. AASLD Abstract no. 879. Hepatology. 2020;72:537A-538A. 5. Rizzardini G, et al. AASLD Abstract no. 929. Hepatology. 2020;72:568A-569A. 6. Larrey D, et al. AASLD Abstract no. 927. Hepatology. 2020;72:567A. 7. Rodriguez-Tajes, et al. AASLD Abstract no. 916. Hepatology. 2020;72:560A-561A. 8. Bansal S, et al. AASLD Abstract no. 932. Hepatology. 2020;72:571A. 9. Andreoni M, et al. AASLD Abstract no. 860. Hepatology. 2020;72:524A. 10. Howell J, et al. J Gastroenterol Hepatol. 2019;34:40-48. 11. Addish E, et al. AASLD Abstract no. 657. Hepatology. 2020;72:397A. 12. Shin Y, et al. AASLD Abstract no. 897. Hepatology. 2020;72:548A. 13. Khalili M, et al. AASLD Abstract no. 935. Hepatology. 2020;72:573A. 14. McDaniel KB, et al. AASLD Abstract no. 464. Hepatology. 2020;72:291A.





