
Specialist in Radiology
Preventing Faulty Alarm - Enhanced Diagnostic Accuracy with Gadoxetic Acid-enhanced MRI
Hepatocellular carcinoma (HCC) is the most common malignant tumour of the liver, whereas the occurrence of the disease is often unaware until progression to advanced stages leading to suboptimal prognosis1. With the recent advancement in diagnostic imaging technologies and instrumentations, the diagnostic performance of imaging modalities has been substantially improved. Nonetheless, technical limitations on sensitivity and accuracy are still clinical challenges for early detection and hence timely treatment of HCC. Meanwhile, there are emerging clinical data supporting the effectiveness of gadoxetic acid-enhanced magnetic resonance imaging (EOB-MRI) in liver imaging which enables early HCC detection with high accuracy. To demonstrate the enhanced diagnostic accuracy of imaging practically, Dr. Solomon Ka shared some clinical cases of improved HCC diagnosis with EOB-MRI.
Diagnostic Imaging for HCC in Local Clinical Practice
Currently, local guideline on diagnostic imaging for HCC is yet to be developed, whereas various international diagnostic guidelines such as the Asian Pacific Association for the Study of the Liver (APASL)2 and the European Association for the Study of the Liver (EASL)3 have recognised gadoxetic acid-enhanced magnetic resonance imaging (EOB-MRI) as one of the first-line imaging modality options for diagnosis of HCC. Dr. Ka stated that routine imaging surveillance for liver nodules often starts with ultrasound (US) imaging in consideration of invasiveness, availability and cost. Nodules detected by US will then be examined with dynamic computed tomography (CT) or MRI. He further commented that one of the potential reasons for not following international guidelines in local practice is the availability of the imaging modalities.
Although EOB-MRI is readily available in the private sector, further optimisation in the multi-disciplinary communication would be needed. Often, the discussions between radiologists and the referral physicians occur after the imaging process. Yet, advices on optimal imaging protocol provided by radiologists before imaging would likely improve diagnostic outcomes.
Problematic Lesions Mimicking HCC
The application of positron emission tomography coupled with CT (PET/CT) in the evaluation of liver lesions is common in local practice. While 18F-fluorodeoxyglucose (FDG) is one of the most commonly used metabolic probes for PET evaluation, dual-tracer PET/CT with 2 metabolic probes such as FDG and 11C-acetate (ACT) is recently available. The dual-tracer PET/CT not only improves sensitivity as compared to FDG-PET/CT, but can also indicates the differentiation status of HCC lesions4.
However, FDG is not a cancer-specific agent and false positive signals in benign disease can be developed. For instance, active inflammation or infection would lead to false positive signals. Inflammatory cells such as neutrophil and activated macrophages at the site of inflammation or infection show increased FDG accumulation5. Besides, focal nodular hyperplasia (FNH) is a benign hyperplastic lesion of the liver and is generally believed to have no potential for malignant transformation. Nonetheless, some cases of FNH have been reported to show mildly increased metabolism6. Thus, FNH could be a potential cause of false positive signals in FDG-PET imaging.
Dr. Ka shared a case of FNH detection, in which a large liver lesion was detected on ultrasound imaging and was worrisome of HCC. The patient was subjected to subsequent EOB-MRI examination. While EOB-modified gadoxetic acid is actively taken up by hepatocytes, HCC lesions do not accumulate gadoxetic acid and thus appear hypointense in the hepatobiliary phase (HBP) as compared to normal liver parenchyma7. In this case, the hepatic lesion shows brisk arterial enhancement as well as gadoxetic acid uptake during HBP (Figure 1b), and hence the lesion was shown to be a FNH.
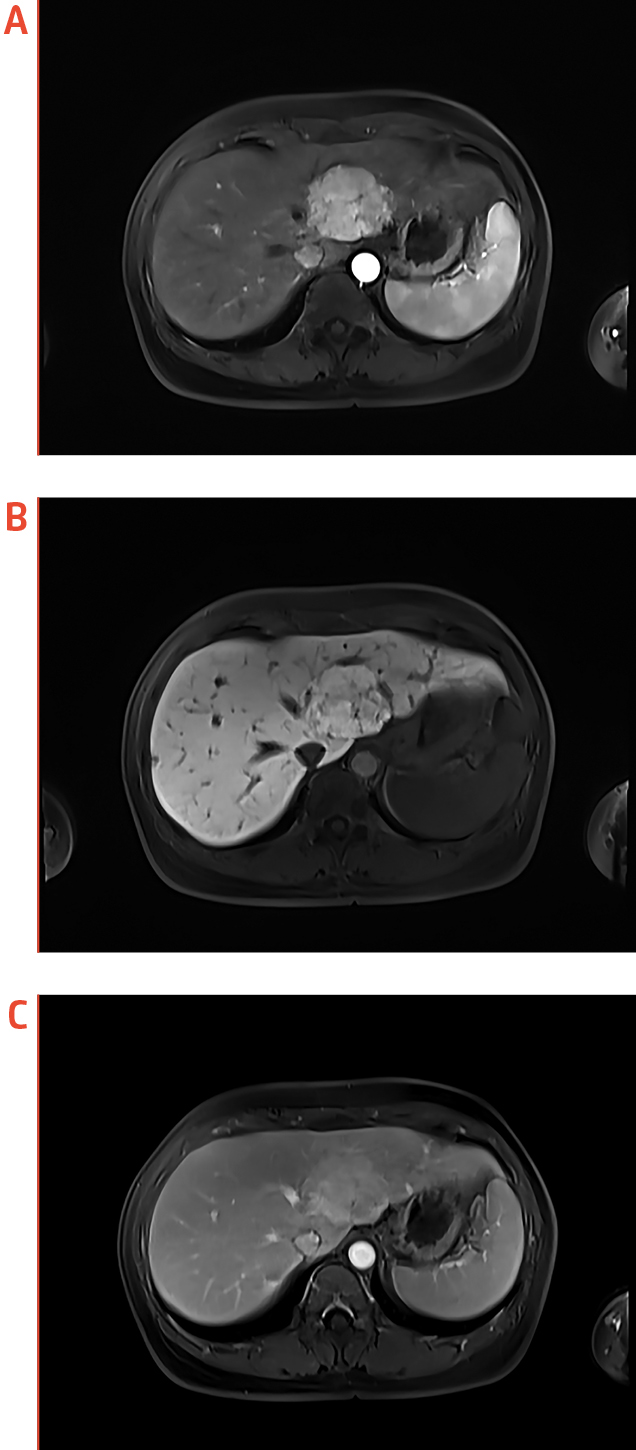
Figure 1. EOB-MRI identification of a FNH, (a) axial arterial phase, (b) axial HBP, and (c) axial portovenous phase
(images provided by Dr. Ka)
Beware of False Negative
In contrast to false positive signals, malignant tumours with low metabolic activity or small tumour volume can result in false negative results in FDG-PET imaging. Former opinion suggested that PET systems with 1-cm resolution are commonly used, whereas the spatial resolution limitation is likely a causative factor of false negative results in PET scans8. Notably, metastasis of tumours with a mucinous component can result in low FDG uptake9. While relative cellularity of tumours is important in the detection of disease using FDG PET, low cellularity in mucinous tumours caused by the presence of mucin would lead to lower FDG uptake10 and hence increasing the risk of false negative results.
In the second case shared by Dr. Ka, the patient with history of breast cancer was presented with deranged liver function. While FDG-PET reflected no significant abnormality in the liver, the patient received additional EOB-MRI examination. Remarkably, EOB-MRI showed numerous sub-centimeter enhancing foci which are hypointense in HBP, suggesting the occurrence of liver metastasis.
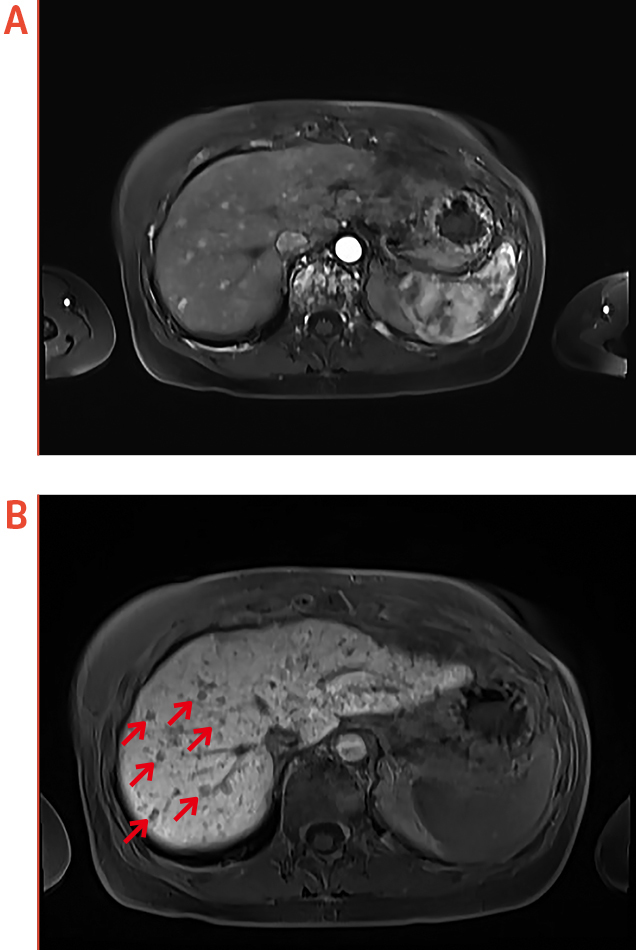
Figure 2. Liver metastasis identified by EOB-MRI, (a) axial arterial phase, (b) axial HBP
(red arrows indicate hypointense foci, images provided by Dr. Ka)
Optimised Diagnostic Accuracy with EOB-MRI
Metabolic imaging with FDG-PET plays an important role in the management of HCC. Nonetheless, the reported sensitivity of FDG-PET in detecting HCC is relatively low1 and the issues of false positive and false negative pose further risk on inaccurate diagnosis. Clinical opinion suggested that in examining diseases located near the physiologic uptake sites, such as heart, bladder, kidney, and liver, FDG-PET should be complemented with other imaging modalities to confirm results8. Essentially, awareness of the conditions and the mechanisms by which false positive and negative signals develop will facilitate accurate interpretation on imaging findings.
The clinical cases shared by Dr. Ka demonstrated the effectiveness of EOB-MRI in ruling out suspected false positive liver lesions and identifying small liver metastasis which are not detected by FDG-PET. Of note, while PET/CT might be limited by spatial resolution, the reported sensitivity of detecting small lesions by EOB-MRI is higher than 90%11.
In reality, each imaging modality has its advantages and limitations. Interestingly, previous investigation demonstrated that add-on EOB-MRI would significantly improve the sensitivity of FDG-PET/CT in detecting small liver nodules as compared to FDG PET/CT alone12. This finding not only showed the enhanced diagnostic accuracy of EOB-MRI, but also highlights the potential benefits of combining imaging modalities.
References
1. Lu et al. World J Gastroenterol. 2019;25(32):4682-4695. 2. Omata et al. Hepatol Int. 2017;11(4):317-370. 3. Galle et al. J Hepatol. 2018;69(1):182-236. 4. Ho et al. J Nucl Med. 2007;48(6):902-909. 5. Alavi et al. Semin Nucl Med. 2002;32(4):293-321. 6. López et al. Clin Nucl Med. 2005;30(9):636-637. 7. Fahlenkamp et al. PLoS One. 2019;14(3):e0213408. 8. Chang et al. Korean J Radiol. 2006;7(1):57-69. 9. Kim et al. Am J Roentgenol. 1998;170(4):935-939. 10. Berger et al. Am J Roentgenol. 2000;174(4):1005-1008. 11. Sun et al. Invest Radiol. 2010;45(2):96-103. 12. Oh et al. Biomed Res Int. 2016;2016.





