

Specialist in Dermatology
Custom Approach to Manage Periorbital Dermatitis
Periorbital dermatitis, also known as eyelid dermatitis, is a manifestation of various ocular pathology, dermatological conditions, such as atopic dermatitis, seborrheic dermatitis, allergic contact dermatitis, irritant dermatitis, rosacea and psoriasis, etc, and sometimes the reaction to ophthalmological medications1,2. In Hong Kong, there is no recent epidemiological data on its prevalence, yet reports from Germany suggest the incidence of periorbital dermatitis ranges from 3.9% to 4.8%2. Though the prevalence is not subtle, significance of a meticulous periocular dermatitis management approach remains undernoted.

Specialist in Cardiology
The Sooner the Better:
Timely Control on Hypercholesterolaemia
Hypercholesterolaemia has been a subject undergoing intense study whilst constant breakthrough in medical management is continuous as figure shows an increased prevalence of the issue. According to the Population Health Survey 2014/15 by the Centre for Health Protection, nearly half of the population aged 15-84 surveyed in Hong Kong have reported having hypercholesterolaemia1. The prevalence increased with age and peaked at 55-64 years old1.
While the general public are often told that “bad diet” is the culprit of high cholesterol, most of the patients have missed the crunch time to manage it through lifestyle modification until condition gets worse or atherosclerosis and its impacts appear. At that time, modifying lifestyle is no longer adequate to turn the table. “Lifestyle developed in young age for example food choice and nutrition, physical activity and energy expenditure are contributing factors for variation in serum cholesterol level2. The middle age group is more prevalent in hypercholesterolaemia because they are the generation who grew up in the hardest era when education and community resource to support healthy lifestyle were scarce. Early screening and prompt medical intervention are therefore important to timely identify and manage soaring blood cholesterol,” said Dr. Wong Bun Lap Bernard, Specialist in Cardiology.
Early Intervention for Better Therapeutic Outcome
From public health perspective, effective and accessible mass screening is essential for early disease identification. In Hong Kong, mass lipid screening has been well done and has successfully identified hidden cases especially among the young to middle-age adults group, as well as rising the concern on underlying unhealthy lifestyle issue. Not only more efforts have to be put in primary health education, early intervention to reach the goal of reducing incidence, healthcare demand and expenditure, prevalence of risk factors, and later cardiovascular risk is of paramount importance1.
Ference BA, et al, 2012 had conducted a series of meta-analyses to estimate the effect of long term exposure to lower low-density lipoprotein cholesterol (LDL-C) on the risk of coronary heart disease (CHD) by mediating 9 single-nucleotide polymorphisms (SNPs) in 6 different genes which the alleles associated with lower LDL-C were used as proxy for treatment3. The study result has implied clinical benefit of early intervention to hypercholesterolaemia management by demonstrating a three-fold greater reduction in CHD risk per unit lower LDL-C than that observed during treatment with a statin started later in life (Figure 1), i.e. a 3 mmol/L reduction in LDL-C is required if treated later by statin to achieve the same magnitude of CHD risk reduction by early intervention, and a 54.5% (OR: 0.46, 95% CI: 0.41 to 0.51; p = 2.15x10-45) reduction in CHD risk for each mmol/L lower LDL-C under long-term exposure to lower LDL-C (Figure 2) 3. Furthermore, an approximately log-linear association between long-term exposure to lower LDL-C and CHD risk was observed, inferring that an early intervention to lower LDL-C level may results in a more substantial reduction on CHD risk3. In spite of this, further clinical research is required.
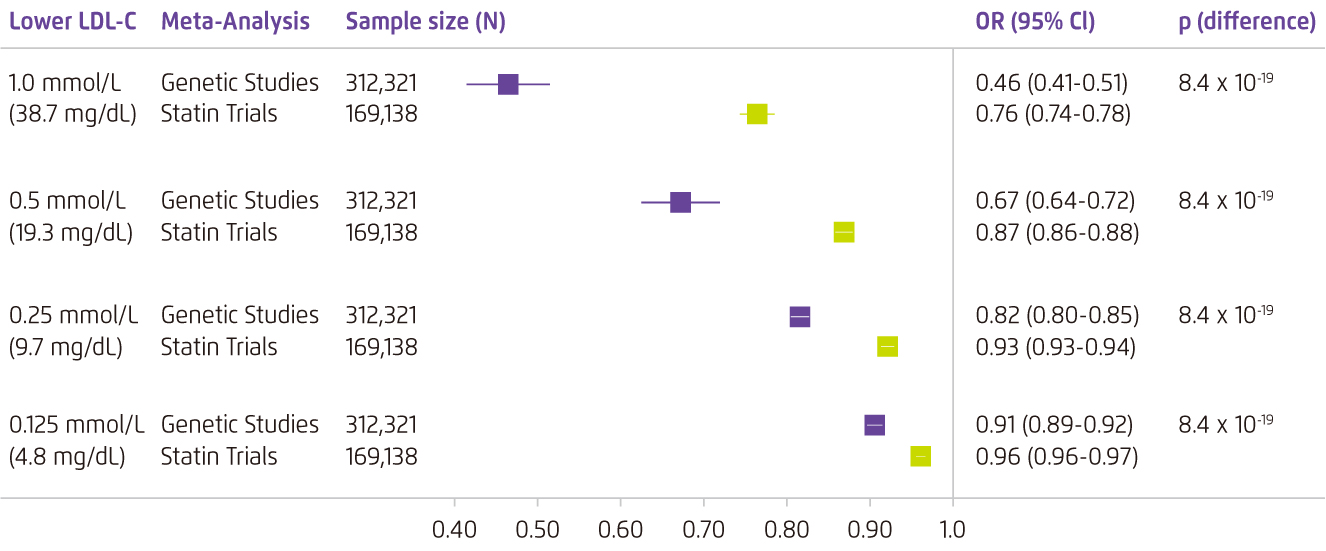
Figure 1. Comparative CHD risk reduction by early intervention and a later one3
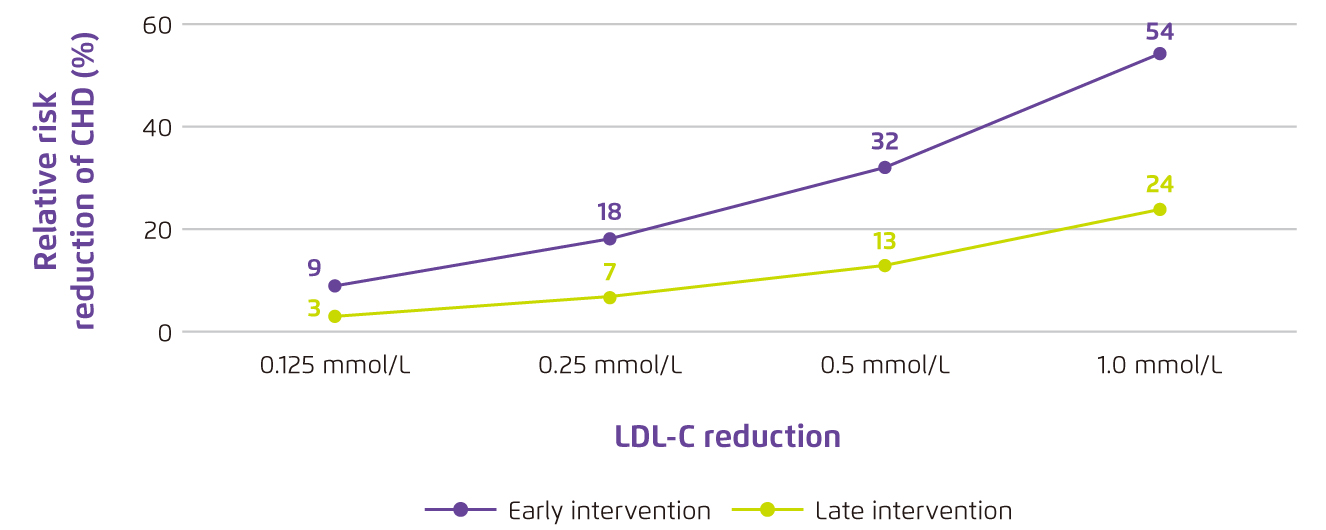
Figure 2. CHD risk reduction associated with LDL-C reduction by early intervention compared with late intervention3
Clinically, statin monotherapy is the mainstay of pharmaceutical intervention for hypercholesterolaemia by lowering blood lipid level through reducing the synthesis of cholesterol in liver and inhibiting HMG-CoA reductase4. Despite the established evidence, efficacy of statin to reach therapeutic goal in reducing LDL-C is dose-dependent and varies between different statins4. Side effect, however, is another issue raised general concern recently although it is inconsequential clinically as commented by Dr. Wong.
The 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk (2009) has given recommendation on selection of regimen according to patient’s profile. For example the initiation of high-intensity or increased intensity of statin therapy is recommended in statin-naïve acute coronary syndromes (ACS) patients and ACS patients who is receiving low or moderate intensity statin at presentation respectively4. In the meanwhile, an addition of non-statin lipid-modifying agent is recommended if patient’s clinical goal were not reached by statin therapy4. Based on this, more researches have been focusing on the feasibility and efficacy of early intervention utilising combination therapy to reach guideline recommended goal.
Ezetimibe plus Atorvastatin for Early Management
“Abundant established evidence has support and sustain the use of statin in treating hypercholesterolaemia , especially in severe cases. Yet recent studies on combination therapy has widen treatment choice. Combination therapy is a good alternative for early management of hypercholesterolaemia with remarkable end point performance and satisfying safety profile,” commented Dr. Wong.
Ezetimibe plus atorvastatin is a lipid-lowering combine therapy selectively inhibits the intestinal absorption of cholesterol and related plant sterols and inhibits the endogenous synthesis of cholesterol5. Double-blind study demonstrated that ezetimibe when added on to statin therapy could consistently produce significance additional lowering of LDL-C level for -54.5% than statin monotherapy (-42.4%, p < 0.01) with therapeutic effects observed as soon as week 26. Furthermore, similar efficacy of 50% and 51% LDL-C reduction and a comparable safety profile were achieved by ezetimibe 10 mg plus atorvastatin 10 mg and atorvastatin monotherapy in maximal dosing respectively6.
Selection of regimen is always case tailor-made. With a thorough consideration on patient’s health and treatment profiles, therapeutic goal and timeline, as well as patient’s accessibility to regimen, prompt intervention is feasible.
References:
1. Centre for Health Protection. Non-Communicable Diseases Watch. August 2019. 2. Soran H, et al. Arch Med Sci. 2018;14:1-21. 3. Ference BA, et al. J Am Coll Cardiol. 2012;60:2631-2639. 4. Mach F, et al. Eur Heart J. 2020;41:111-188. 5. Atozet. Hong Kong Prescribing Information. HKPC-MK0653C-T-042017 6. Ballantyne CM, et al. Circulation. 2003;107:2409-2415.





