

Specialist of Endocrinology,
Diabetes and Metabolism
Beyond Prevention of Stroke and Systemic Embolism - Managing the Unmet Needs in Diabetes Mellitus with Atrial Fibrillation
Diabetes mellitus is a risk factor for stroke and systemic embolism (SE) in patients with atrial fibrillation (AF)1. Essentially, patients with type 2 diabetes mellitus (T2DM) complicated with AF-associated stroke are reported to have worse clinical outcome as compared to those without T2DM2. Clinically, long-term anticoagulation is indicated in majority of T2DM patients with AF to prevent adverse AF-associated embolic events2. While warfarin is widely used as anticoagulant therapy to prevent primary and secondary thromboembolic events, several adverse effects of warfarin therapy on the kidney have been reported3. In a recent sharing,
Dr. Choi Cheung Hei highlighted the essentials in the clinical applications of nonvitamin K antagonist oral anticoagulants (NOACs) in T2DM with AF.
The Complication of T2DM with AF
Prolonged elevation in blood glucose level would result in various health complications including cardiovascular diseases (CVDs) and kidney diseases4. In particular, T2DM was found to be a strong and independent risk factor for AF. The increase in the risk of developing AF for diabetic patients was reported to be about 30%, whereas the increased risk for pre-diabetic patients was 20%5. Dr. Choi outlined that the development of AF in diabetes is associated with insulin resistance, chronic inflammation, metabolic changes, obesity and hypertension6.
As compared to non-DM patients, higher risk and severity of stroke can be observed in patients with co-existing T2DM and AF2. Dr. Choi added that significant chronic kidney disease (CKD) develops in about 20% of this group of patients, even worse is that renal impairment would further exacerbate AF. Thus, effective and timely management of T2DM with AF is crucial.
Challenges in Managing T2DM with AF
In addition to the increased risk of comorbidities and mortality2, the co-existence of T2DM and AF would complicate the management protocol for the patients6. In particular, Dr. Choi reminded that the potential bleeding risk associated with oral anticoagulants has to be taken into account in selecting the appropriate therapeutics. He further addressed that a substantial proportion of diabetes and AF cases are asymptomatic. Hence, timely treatment for diabetes and AF is sometimes difficult. Nonetheless, Dr. Choi advised that anticoagulation should be prescribed for all of the patients with diabetes in clinical practice in consideration of their risk of stroke. Moreover, in view of the substantial proportion of renal impairment among diabetic patients, the renal function of patients should be considered.
Clinical Evidence on Benefits of NOACs
NOACs are commonly prescribed for AF patients to prevent stroke, whereas the efficacies of the 4 major NOACs, i.e. dabigatran, rivaroxaban, apixaban and edoxaban, have been proven in the 4 landmark randomised control trials (RCTs)7-10. Interestingly, in reviewing the baseline characteristics of the patients recruited, the proportion of patients with diabetes in the ROCKET-AF trial for rivaroxaban, about 40%8, was substantially higher as compared to those in the other 3 landmark trials, which ranged between 23%-36% (Table 1)7,9,10. Essentially, the benefits of rivaroxaban in preventing stroke were consistent in patients regardless of diabetes (Figure 1)11. These findings hence indicate the efficacies of rivaroxaban in diabetic AF patients.
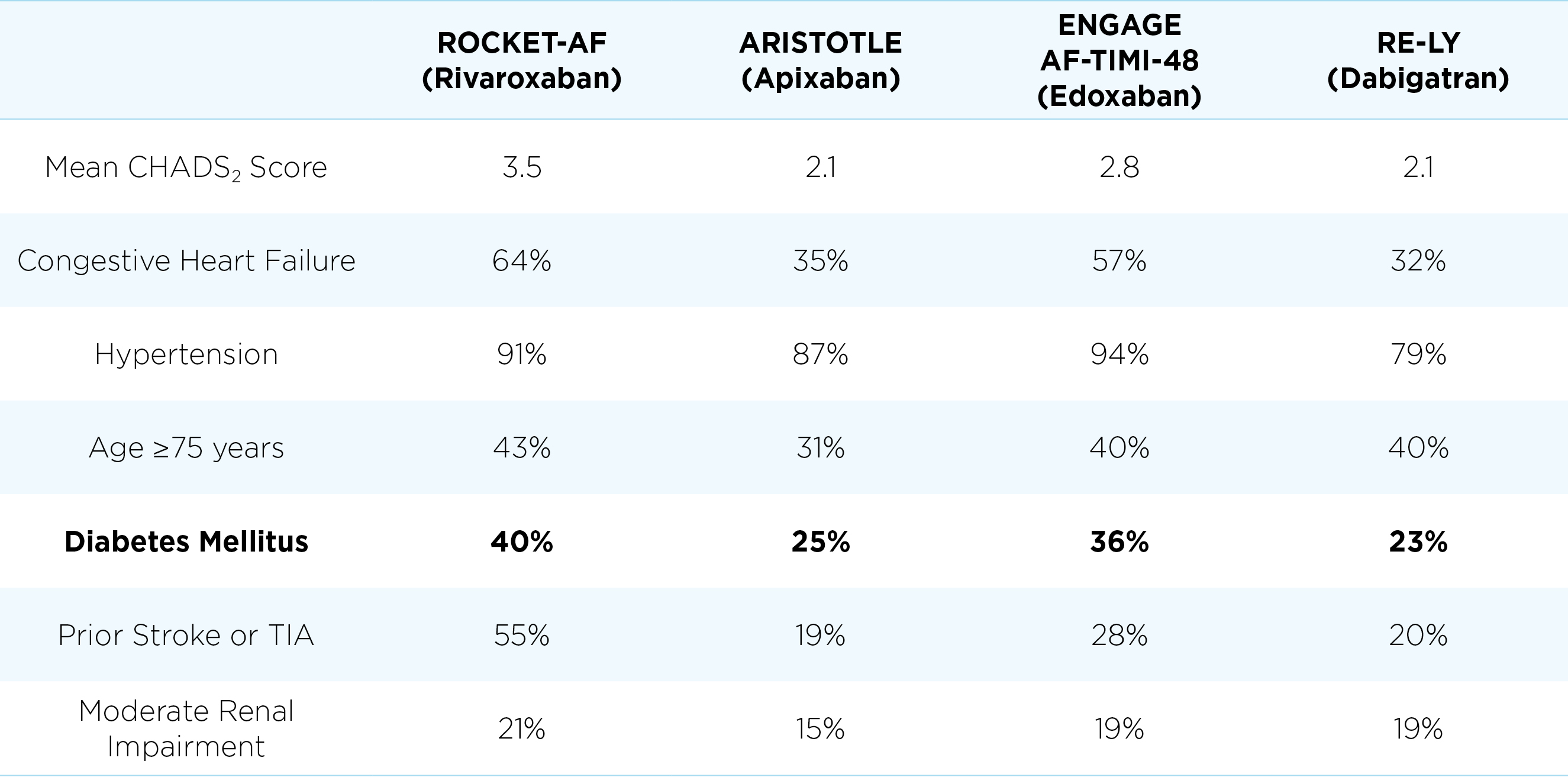
Table 1. Differences in patient characteristics in the 4 landmark RCTs7-10.
TIA: transient ischaemic attack
(Data in this table are not for head-to-head comparison)
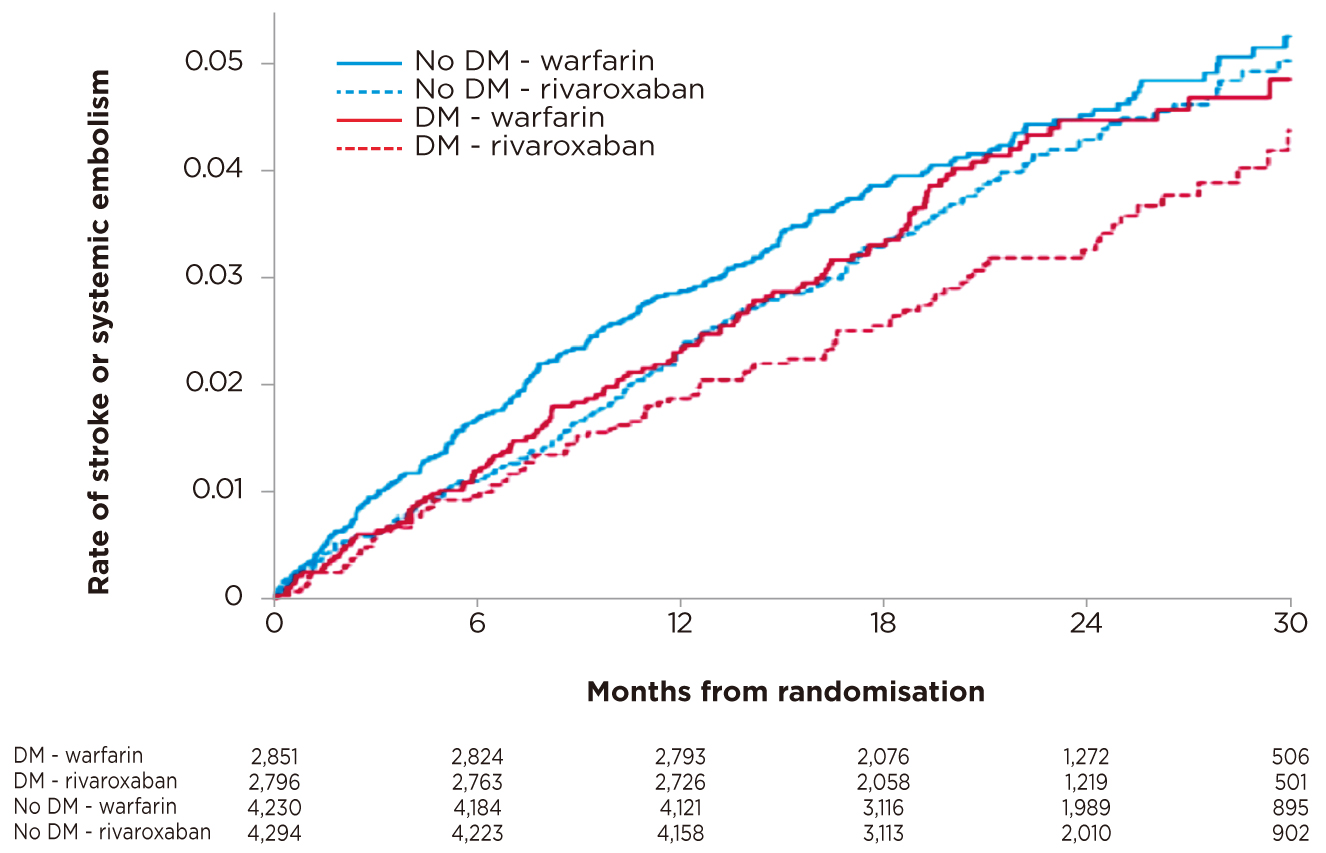
Figure 1. Rate of stroke and SE upon rivaroxaban or warfarin treatment11
Dr. Choi commented that, due to the differences in design and patient characteristics in the RCTs7-10, the results of the RCTs should not be compared directly. Nonetheless, he agreed that there is evidence showing rivaroxaban is effective in reducing the risk of stroke/SE in AF patients with diabetes as compared to warfarin while no increase in bleeding risk12. Of note, he emphasised that there is no solid evidence suggesting a certain NOAC is safer than the others.
Dr. Choi agreed that there are more observational data available for rivaroxaban on reducing risk of CVD, adverse limb events and slowing the decline in renal function among patients with diabetes. As mentioned, in a subgroup analysis of ROCKET-AF trial involving diabetic patients, rivaroxaban was shown to significantly reduce the risk of CV mortality among the patients by 20% as compared to warfarin (hazard ratio [HR]: 0.80, p = 0.037, Table 2)11. Dr. Choi noted that rivaroxaban would have advantage in term of evidence-supported treatment outcomes.
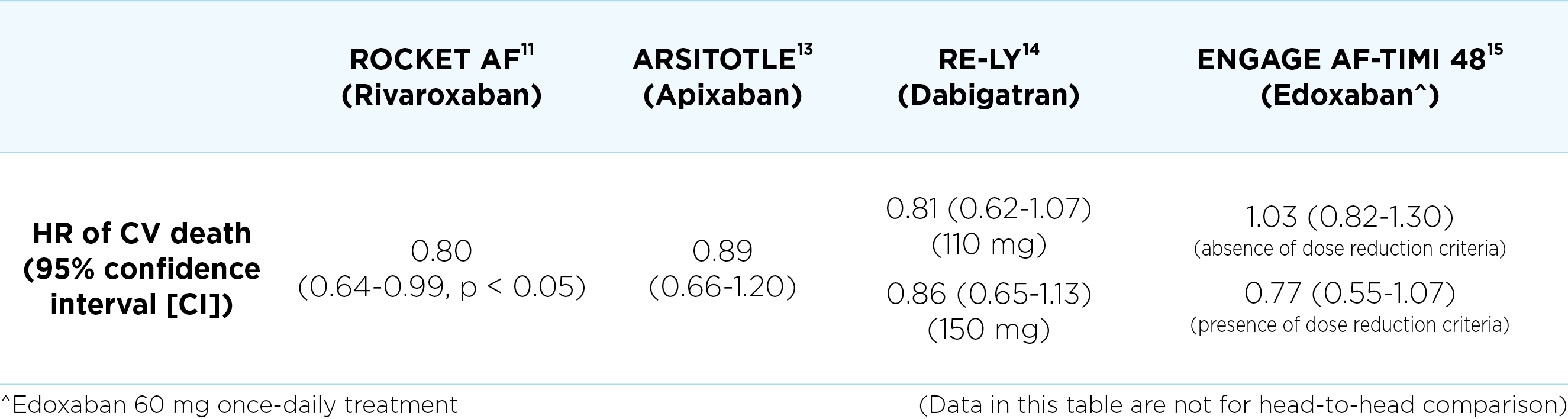
Table 2. Hazard ratios of CV deaths of NOACs in diabetes subgroup in landmark trials
Evaluating the Risks of Major Bleeding
Recently, the first real-world observational and prospective study involving 1,443 AF patients confirmed the good profile of NOACs in terms of safety and effectiveness. Particularly, the results suggested that rivaroxaban was associated with the lowest rate of major bleeding (0.8 events per 100 patient-years) as compared to other NOACs (dabigatran: 1.8 events per 100 patient-years; apixaban: 1.7 events per 100 patient-years; edoxaban: 1.2 events per 100 patient-years, p = 0.04 rivaroxaban vs the other NOACs)16. Nonetheless, Dr. Choi highlighted that matching is not possible in the prospective study and the baseline characteristics of patients were different, which limit the accuracy of results. On the other hand, he commented that previous studies suggesting the lowest bleeding risk of apixaban were not randomised and thus selection bias and confounding factors would be involved.
“In ordinary patients, there is no convincing evidence suggesting which NOAC is better between apixaban and rivaroxaban. For edoxaban, clinical data are limited and hence no conclusive comment can be made,” addressed Dr. Choi. According to Dr. Choi, the bleeding risk of apixaban and rivaroxaban is similar practically.
The Keys for Optimal Treatment Outcomes
In the management of T2DM in AF, Dr. Choi highlighted the implication of patients’ compliance. “The difference between once and twice daily is significant practically since diabetic patients take many medications daily, and can be up to 10 different medications,” he addressed. This results in a complicated schedule for medication intake as the drugs are taken at different times. In Dr. Choi’s observations, nearly half of the patients are non-compliant. “In general, once daily therapy is more welcomed and hence can achieve better compliance comparing to multiple doses per day,” noted Dr. Choi.
Anticoagulation is important for patients with T2DM and AF. To enhance compliance, Dr. Choi advised to explain to patients why the medication is important and the consequences of not compliant to the treatment. He reminded that most of the patients fear the consequences of stroke and the related complications. He suggested frontline clinicians to make notes or reminders on medication intake for the patients and/or their family or caregivers. He further quoted that some doctors would count the remaining drugs provided for the patients in order to evaluate if the patients have adhered to treatment. On the other hand, a well-designed schedule for medication intake would encourage compliance.
In summary, Dr. Choi outlined 5 essential clinical measures in managing patients with T2DM and AF, which are featured as the “ABCDE” elements. Briefly, “A” refers to active stroke prevention by prescribing anti-coagulants; “B” is the better rate control; “C” means CV risk factor prevention; “D” refers to diabetes control and “E” is early identification. Moreover, Dr. Choi advised that close monitoring of patient’s renal function is important. In selecting therapeutics for patients, the patient’s risk of stroke has to be estimated. He advised that AF patients with longer duration of diabetes and uncontrolled blood glucose level are already at high risk, whereas non-compliance will further increase the risk. Based on the established evidence, rivaroxaban is preferred for the high-risk patients with T2DM and AF.
References
1. Oladiran et al. J Community Hosp Intern Med Perspect 2019; 9: 113-20. 2. Prídavková et al. J Diabetes Res 2019; : ID 5158308. 3. Ishii et al. CEN case reports 2018; 7: 198-203. 4. Petrie et al. Can. J. Cardiol. 2018; 34: 575-84. 5. Aune et al. J. Diabetes Complications. 2018; 32: 501-11. 6. Tadic et al. Arch. Cardiovasc. Dis. 2015; 108: 269-76. 7. Connolly et al. N Engl J Med 2009; 361: 1139-51. 8. Patel et al. N Engl J Med 2011; 365: 883-91. 9. Granger et al. N Engl J Med 2011; 365: 981-92. 10. Giugliano et al. N Engl J Med 2013; 369: 2093-104. 11. Bansilal et al. American Heart Journal. 2015: 675-682.e8. 12. Lip et al. Mayo Clin Proc 2020; 95: 929-43. 13. Ezekowitz et al. Eur Hear J - Cardiovasc Pharmacother 2015; 1: 86-94. 14. Brambatti et al. Int J Cardiol 2015; 196: 127-31. 15. Plitt et al. Int J Cardiol 2020; 304: 185-91. 16. Cerdá et al. J Comp Eff Res 2019; 8: 165-78.





