

Specialist in Cardiology
Cholesterol: Lower is Better. But What is the Best Way to Get There?
“The 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias” recommends more intensive reduction of LDL-C across cardiovascular risk categories, listing a revised concept of LDL-C goal of <1.4 mmol/L and <1.8 mmol/L for very-high risk patients and high risk patients respectively.
Blood lipid disorders have become global health concerns in the 21st century1. In previous guidelines for managing dyslipidaemias, the importance of low-density lipoprotein cholesterol (LDL-C) lowering to prevent atherosclerotic cardiovascular disease (ASCVD) has repeatedly been emphasised2. The latest guideline for the management of dyslipidaemias by European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) recommends more intensive reduction of LDL-C across cardiovascular risk categories, listing a revised concept of LDL-C reduction of ≥50% from baseline or a LDL-C goal of <1.4 mmol/L and <1.8 mmol/L for very-high risk patients and high risk patients respectively (Table 1)2,3. The new recommendation is particularly based on meta-analyses which confirm the dose-dependent reduction in ASCVD with LDL-C lowering agents, suggesting a strong correlation between LDL-C level and cardiovascular risk2.
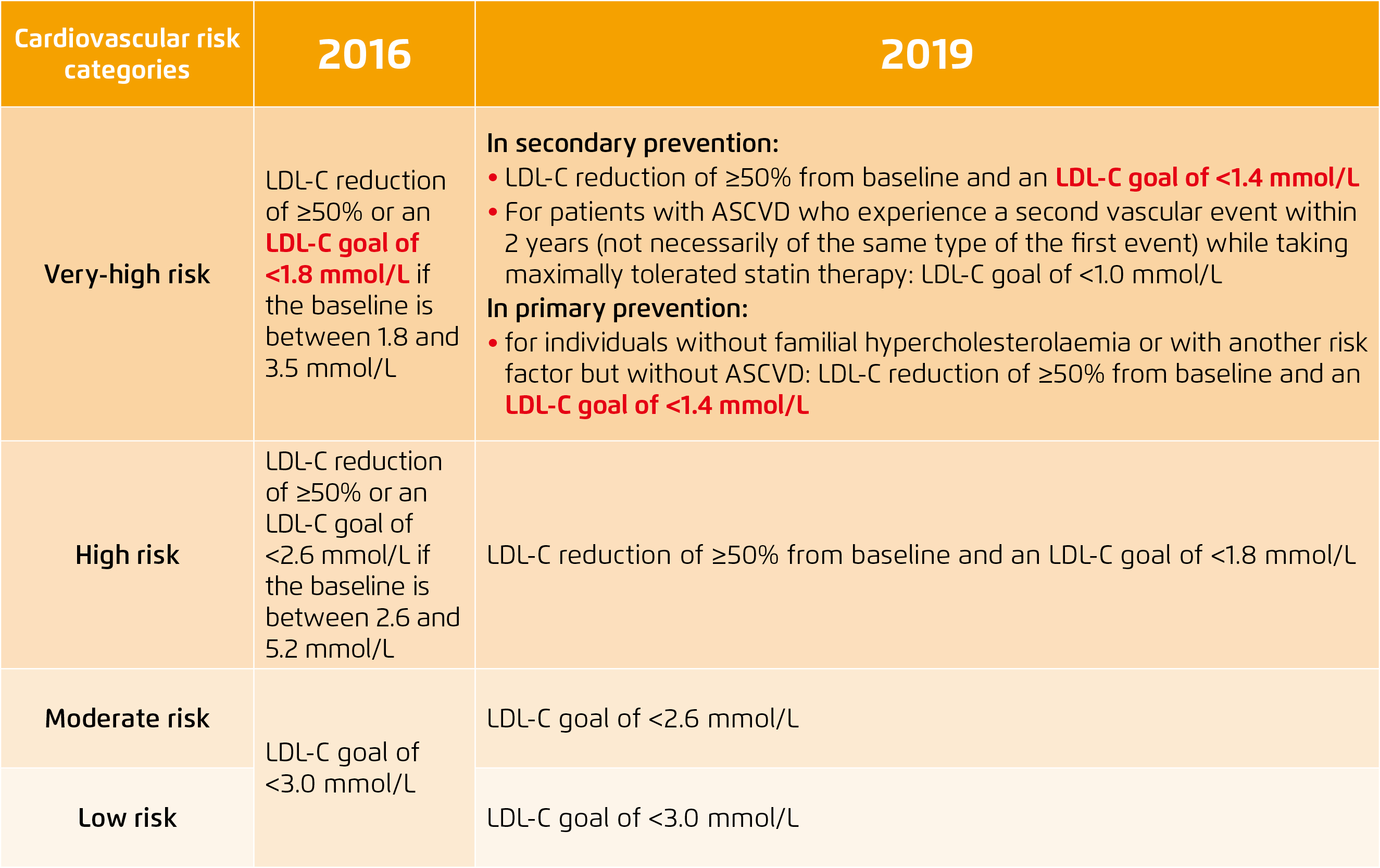
Table 1. Comparison of LDL target recommendations for cardiovascular disease prevention between 2016 and 2019 ESC/EAS guideline for the management of dyslipidaemias 2,3
Disease Overview in Hong Kong
As known, hypercholesterolaemia is one of the major modifiable risk factors for ASCVD, leading to heart complications and peripheral vascular diseases4. In 2017, 4.32 million deaths attributed to high LDL-C level globally1. In Hong Kong, according to the Population Health Survey 2014/15 by the Centre for Health Protection, 49.5% and 35% of the population aged 15 to 84 surveyed reported having hypercholesterolaemia and had a borderline high or above level of LDL-C respectively1. The prevalence increased with age and peaked at age 55 to 64, revealing relatively high cardiovascular risk among the middle-aged population1.
Conventional Treatment for Hypercholesterolaemia is Sometimes Suboptimal
Conventional treatment includes statins, bile-acid-binding resins, cholesterol absorption inhibitors and some injectable medications, for example PCSK9 inhibitors. These medications lower blood cholesterol levels through different mechanisms of action and provide a choice of treatment regimens to meet clinical needs. Among those, statins have been an indisputable first-line medication recommended by international guidelines2. However, there is significant on-treatment residual cardiovascular risk and some patients fail to achieve LDL-C targets by taking a stain alone5,6. Previous studies also described the “rule of six”, which depicts that every doubling of statin dose can only further reduce LDL-C by 6% on average6. “If patients is taking a medium dose treatment, doubling of statin dose might exert a further but limited reduction of LDL-C. However, since statins work by blocking HMG-CoA reductase that is involved in the synthesis of a sterol precursor, LDL reduction achieved depends on the level of enzyme,” commented Dr. Adrian Cheong, Specialist in Cardiology. Apart from concerns about efficacy, side effects attributable to statins are generally dose-related and are a major concern during titration to higher doses of statins to reach therapeutic goals. According to an international survey by Waters et al. in 2016, the incidence of statin intolerance varies between 2 to 12% across nations, which is a significant hurdle in the management of hypercholesterolaemia7.
Ezetimibe Add-on to Statin to Hit LDL-C Goal
In clinical practice, combination therapy is often prescribed when first-line medication fails to attain clinical goal. Ezetimibe add-on to statin therapy is prescribed if statin or other monotherapy is not able to attain targeted LDL-C level. Ezetimibe is a lipid-lowering agent that selectively inhibits the intestinal absorption of cholesterol and related plant sterols and inhibits the endogenous synthesis of cholesterol8. According to the Ezetimibe Add-on to Statin for Effectiveness (EASE) trial, ezetimibe added to stain therapy can additionally reduce LDL-C by 25.8%, compared with an additional 2.7% by placebo and statin (treatment difference: -23.1%, p<0.001); and 70.1% of patients taking ezetimibe reached their National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) target LDL-C level compared with 20.6% of patients taking placebo (p<0.001)9. Moreover, treatment adherence is affected by treatment schedule, administration method and drug safety profile. Thus combination therapy to achieve maximal therapeutic efficacy with minimal toxicity and drug side effects should be an effective treatment option. The EASE trial shows a similar safety profile for ezetimibe verse placebo, when added to background statin therapy6,9.
Setting Our Sights on Lower Goals
Revisiting the revised guideline on intensive LDL-C lowering goals, combination therapy is potentially more effective at bringing more at-risk patients to guideline recommended LDL-C levels. Studies from the past two decades generally demonstrated evidence of improved cardiovascular health. For instance, a lower level of serum cholesterol is associated with correspondingly low cardiovascular risk in rural China and Japan4. “Clinical studies show that plaque can shrink when LDL-C levels are reduced to <1.8 mmol/L, and a LDL-C level <1.4 mmol/L is even more favourable,” commented Dr. Cheong. “Early use of combination therapy is feasible and beneficial to disease management. I had a treatment-naïve patient aged 50 with baseline LDL-C level measured at 3.6 mmol/L successfully reduced LDL-C level to 1.3 mmol/L in one month by taking atorvastatin 20 mg and ezetimibe 10 mg in a fixed dose combination pill. The patient reported no side effects and expressed a willingness to make lifestyle changes to the benefit of his cardiovascular health,” shared Dr. Cheong.
Translating new guidelines into clinical practice often takes time, as the clinician needs to gradually accept the safety and efficacy of the proposed treatment algorithm. Moreover, patient expectations need to be accounted for in the process. Change takes time, but the best way to achieve lowered cholesterol level is just there.
References
1. Non-Communicable Diseases Watch. August 2019. Center of Health Protection. 2. Mach A, et al. European Heart Journal. 2019;00:1-78. 3. Catapano AL, et al. European Heart Journal. 2016;37:2999-3058. 4. Soran H, et al. Arch Med Sci. 2018;14:1-21. 5. Ballantyne CM, et al. Circulation. 2003;107:2409-2415. 6. Nodari S, et al. Heart International. 2007;3:12-17. 7. Waters DD, et al. JAMA. 2016;315:1571-1572. 8. Atozet. Hong Kong Prescribing Information. HKPC-MK0653C-T-042017 9. Pearson TA, et al. Mayo Clin Proc. 2005;80:587-595.





