
Editor-in-Chief, V·Pulse

Doctor at the National Health Services (NHS), United Kingdom (UK)
Obesity is a global pandemic and a growing public health concern due to the burden exhibited on the psychosocial and economy. Furthermore, global incidence of obesity has doubled over the last three decades1. Needless to say, obesity has been widely reported to increase the risk of cardiovascular disease (CVD) and is recognised as a key driver of various metabolic syndromes, including type 2 diabetes (T2D) and hypertension. More recently, obesity and diet-induced metabolic dysfunction have been identified as the risk factors behind the development of a wide range of neurological disorders2. More importantly, the detrimental effects of obesity have recently been shown to affect the cognitive functioning3,4 despite there are contradicting clinical data suggesting the protective effect of excess adiposity5. Given that obesity may play a role in the development of cognitive decline, the potential of physical activities and weight control to minimise obesity-associated neurological complications has attracted the interest of researchers and clinicians. The aim of this article is to review the evidence correlating obesity with cognitive function decline, in addition to substantiate the clinical performance of weight control measures in reducing the risk of cognitive decline.
The Pathophysiological Link between Obesity and Cognitive Decline
Although the mechanism underlying obesity-associated cognitive decline remains elusive, inflammatory process, oxidative stress, and microglia activation have been reported as the essential components behind the pathogenesis of many neurodegenerative disorders6. For instance, microglia cells found in the central nervous system (CNS) are responsible for the surveillance of baseline neuronal activity and provides rapid response to tissue damage. Recent literature suggested that microglia control the populations of other resident CNS cell types with their ability to induce cell death using reactive oxygen species (ROS) and nerve growth factor (NGF), as well as promote neuron survival by secreting trophic factors and cytokines7.
Microglia is also able to propagate inflammatory signals in the periphery by producing the proinflammatory cytokines interleukin 1- beta (IL1β), IL6, and tumour necrotic factor-alpha (TNFα). Accordingly, high levels of systemic TNFα can cross the blood-brain barrier (BBB) and activate more microglia cells trigger cascade of inflammation. This results in persistent and self-generated neuroinflammation (Figure 1)8. Of note, metabolic diseases, such as obesity and T2D are associated with chronic systemic inflammation and thus pose a higher risk of developing neurodegenerative diseases9.
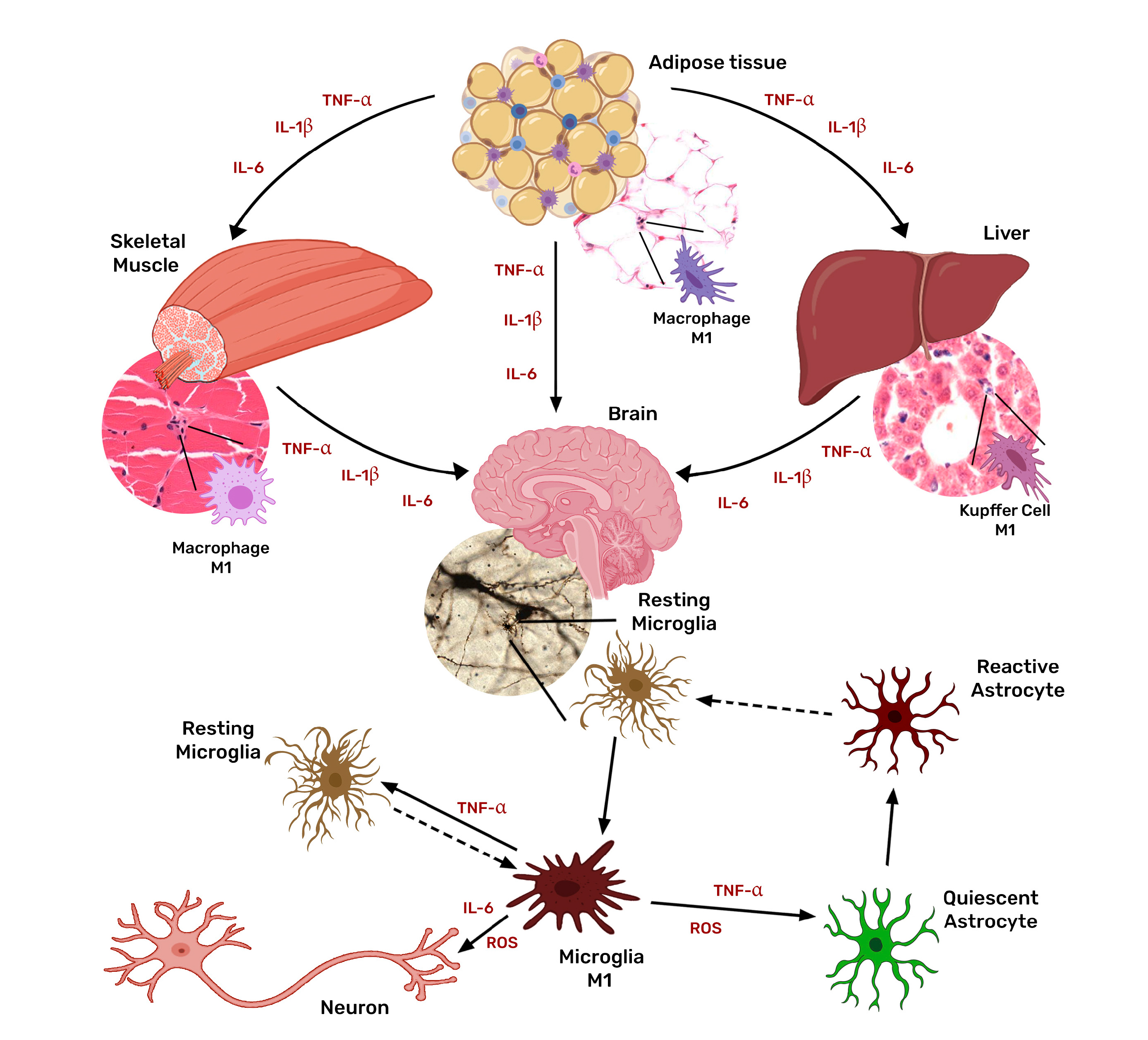
Figure 1. Neuroinflammation triggered by systemic inflammation-associated microglia activation8 (Source of figure: Salas-Venegas et al., [2022])
While there are mounting evidence linking obesity to the gut microbiota dysbiosis, the gut microbiota dysbiosis has also been proposed to contribute to the pathogenesis of neurodegenerative diseases via the gut-brain axis. Animal studies have shown that the absence of gut microbes is associated with structural alterations in the BBB, characterised by decreased expression of tight junction proteins, leading to increased permeability10. Hence, this provides a gateway for intestinal lumen-derived factors to reach the brain parenchyma, stimulating local immune cells and triggering neuroinflammation11.
Moreover, there are two primary driving factors between obesity and the development of neurological disorders. Firstly, obesity contributes to the increased secretion of inflammatory cytokines by adipose tissue and immune cell infiltration, leading to chronic low-grade inflammation. Secondly, obesity is associated with changes in gut microbiota composition, increased gut-vascular barrier (GVB) and BBB permeability. The low-grade inflammation seen in obesity alters the gut-brain axis allowing inflammatory molecules to reach the CNS, promoting the neuroinflammation and cognitive decline.
The neuroinflammatory response during obesity occurs in different areas of the CNS, such as the cerebral cortex, hypothalamus, cerebellum, and the amygdala. Nonetheless, neuroinflammation generated in the hippocampus became the subject interest of recent studies since high-fat diet (HFD)-induced obesity has shown to cause learning and memory deficits with impaired executive functioning in animal models within the hippocampal areas2. Apart from hippocampal structural alterations, HFD feeding also results in decreased expression of neurogenesis markers, synaptic plasticity, and neuronal growth, including the brain-derived neurotrophic factor12,13.
Clinical Evidence on the Association between Obesity and Cognitive Decline
Although the exact pathophysiological mechanism remains unclear, there are emerging clinical data advocating the association between obesity and cognitive impairment. Accordingly, the older population has been studied in particular for its higher susceptibility to cognitive decline.
The cross-sectional study involving 9,189 participants, with a mean age of 57.8 years, by Anand et al. (2022) reflected that generalised and visceral adiposity were significantly associated with reduced cognitive scores after adjustment for cardiovascular risk factors, educational level, and vascular brain injury (Figure 2). Remarkably, for every one-standard deviation increase in body fat percentage (9.2%) or visceral adipose tissue volume (VAT, 36 mL), the Digital Symbol Substitution Test (DSST) score was lower by 0.8 points (p <0.001). The population-attributable risk for reduced DSST score for higher body fat percentage was 20.5%. Nonetheless, the results revealed no significant association between the higher body fat percentage and VAT and Montreal Cognitive Assessment (MoCA) scores (p=0.19)14.
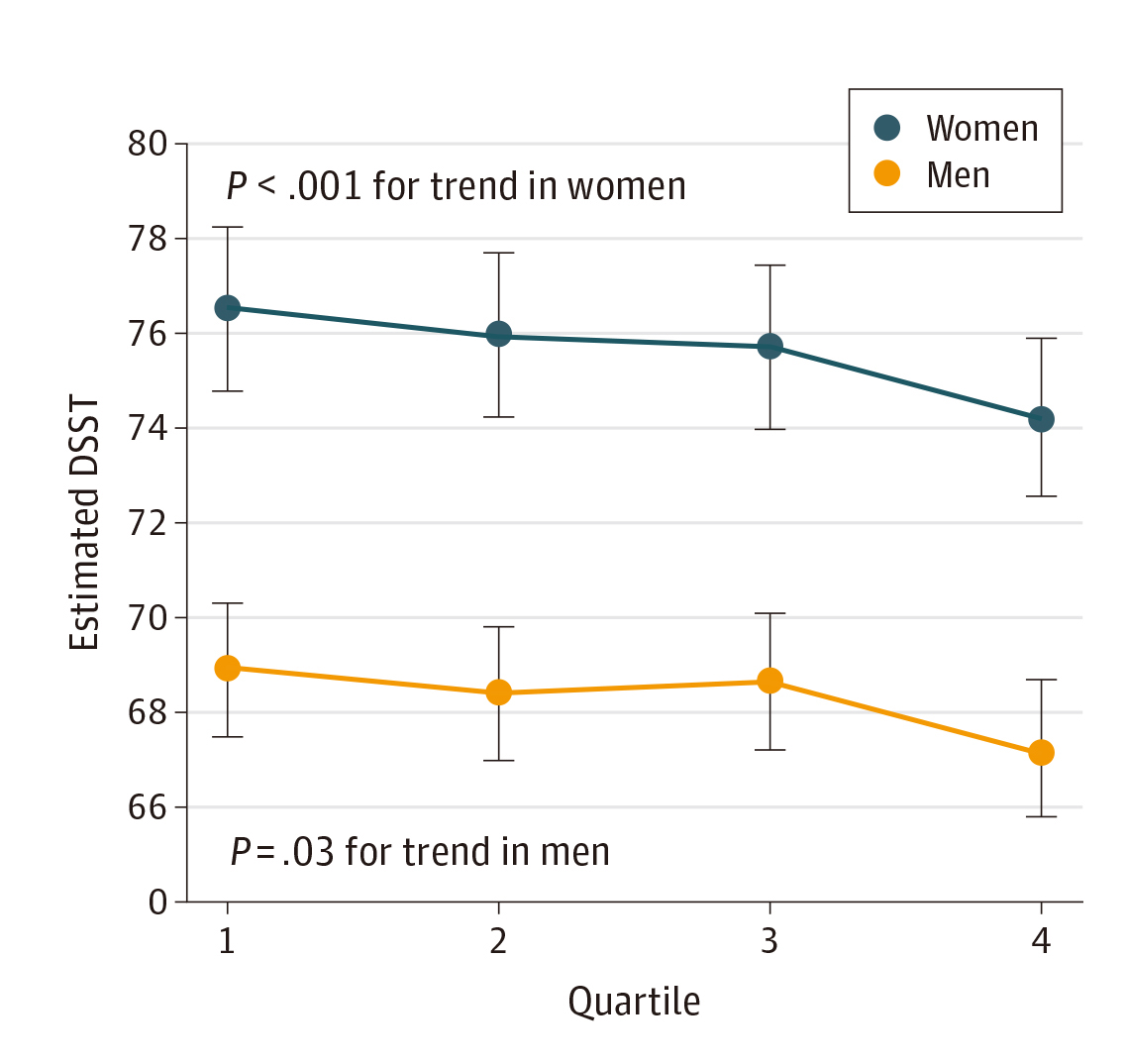
Figure 2. The association between estimated DSST score and sex-specific quartiles of body fat percentage14
In contrast to older adults, another cross-sectional study by Meo et al. (2019) investigated the effect of obesity on cognitive function among school adolescents. In the study, 400 healthy school adolescents, with a mean age of 13.9 years, were recorded as per the study tool of the Cambridge Neuropsychological Test Automated Battery (CANTAB). The results suggested that severely obese students showed a significant delay in cognitive functional development as compared to students with normal body mass index (BMI) and that the Attention Switching Task (AST)-Latency among students with normal BMI (647.88±137.59) was significantly lower than those with a high BMI (685.08±115.92, p=0.05). Strikingly, better AST-Percent correct trials were observed in students with normal BMI (84.31±10.45 vs 78.09±14.87, p=0.001)4.
Similarly, Rukadikar et al. (2023) investigated how obesity adversely affects the cognitive function of healthcare professionals (HCPs). Among the HCPs recruited, the average percentages of body fat of males (n=194) and females (n=281) were 38.19% and 42.26%, respectively. Essentially, the results demonstrated a significant positive correlation between BMI and percentages of body fat and the scale of general frequency of forgetting and seriousness of forgetting. On the contrary, a negative correlation was observed between the scale of retrospective functioning and mnemonics usage and the obesity parameters1.
Therefore, the result from these studies appears to suggest that obesity being independently associated with cognitive impairment regardless of the age or gender. Remarkably, while HCPs are expected to be more intellectually competent in general, the study of Rukadikar et al. highlighted the potential adverse cognitive impacts of obesity, in terms of memory loss, among HCPs.
The “Obesity Paradox” in Cognitive Functioning
Despite the published data on obesity-associated cognitive impairments, some reports have suggested a positive correlation between obesity and favourable cognitive outcomes in older adults, leading to the controversy of the "obesity paradox". The obesity paradox highlights the association between excess adiposity and favourable health outcomes, which has been reported in aged populations with clinical conditions such as coronary heart disease15 and T2D16. Yet, it remains unclear if this paradox persists for cognitive outcomes.
In this regard, a cross-sectional study by Skinner et al. (2017) included 331 adults aged >55 years, reported that participants who were obese had significantly better cognitive flexibility performance than those with normal weight (Trail Making Tests [TMT-B]: 4.0 [obese] vs 16.3 [normal weight], p=0.02). This association was not merely influenced by the age or race. However, adiposity was not associated with psychomotor speed (TMT-A), general cognition (Short Blessed Test [SBT]), or measures of physical function (all p>0.05)17.
These findings are not in isolation as Zhang et al. (2017) revealed a significant (p<0.001) association between higher BMI and less Mini-Mental State Examination (MMSE) decline, even after controlling for demographics and comorbidities in 16,791 hypertensive patients (Figure 3A and 3B)18. Hence, this may suggest that obesity had protective effect on cognitive impairment.
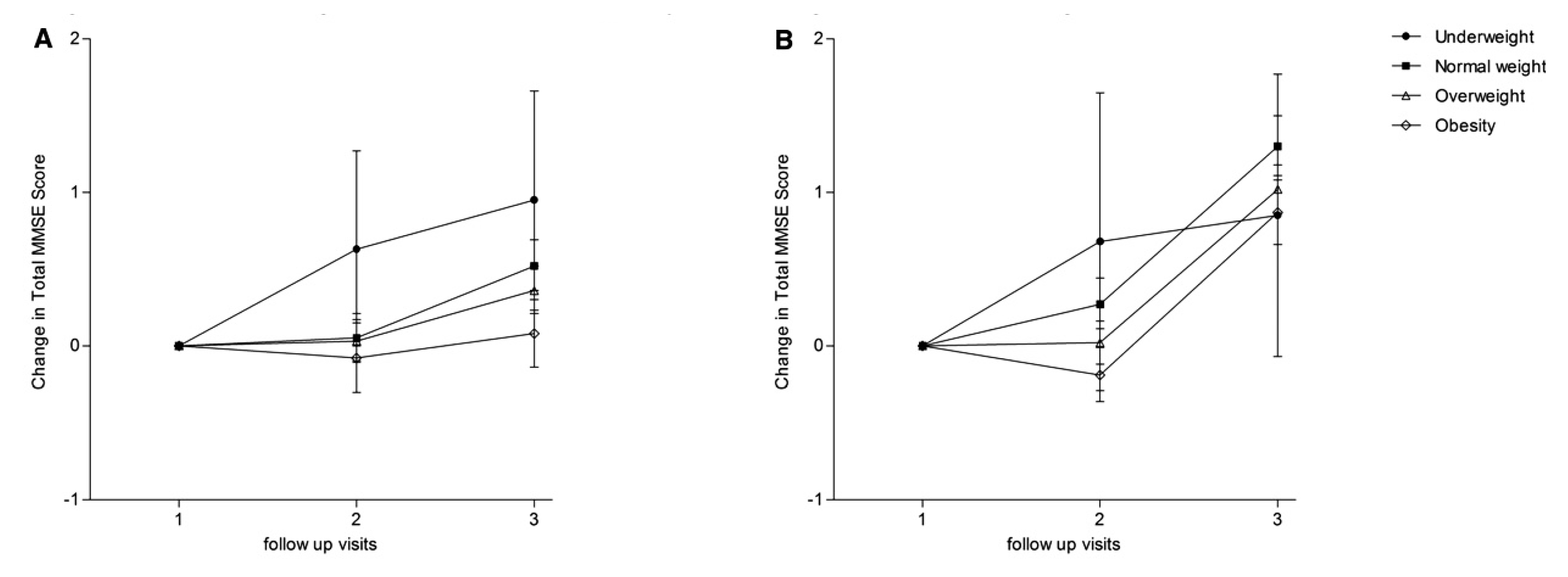
Figure 3. Mean change in total MMSE score by BMI during follow-up in A) men and B) women18
Although the controversy over the obesity paradox in cognitive functioning is not conclusive, it is crucial to be aware of the risk of other adverse health outcomes associated with obesity. Besides, former opinions criticised the study design of certain studies advocating the obesity paradox is flawed since the studies included measurement, selection, and survival biases, while possible confounders were not adequately adjusted19.
Regular Physical Activity Protects Cognitive Functioning
In regard to the contradicting findings related to the association between obesity and cognitive functioning, the insightful report by Kronschnabl et al. (2021), which examined the longitudinal data of 58,389 participants from 15 countries aged >50, indicated that the positive association between BMI change and change in cognitive performance observed was dominantly driven by BMI decrease while weight gain was on average not significantly related to cognitive performance20.
In line with Kronschnabl et al., a longitudinal study involving 1,028 cognitively unimpaired older adults by Pitrou et al. (2022) reported no correlation between the weight and cognitive decline. However, individuals with overweight reporting high physical activity had lower odds of cognitive decline (odds ratio [OR]: 0.25). Thus, it is likely that the physical activity may be the missing link between being overweight and cognitive decline in individuals21.
More recently, an analysis by Xu et al. (2024) that included 7,392 participants aged ≥45 between 2011 and 2018 indicated that vigorous physical activity significantly explained 5.94% of the relationship between obesity and cognitive decline22. Thus, alternative factors may serve as mediators in the relationship between obesity and cognitive decline, and further exploration of the potential factors is warranted.
In conclusion, although the pathophysiological mechanism remains eluded, and there are contradicting evidence between obesity and cognitive decline, one thing remains substantial and that is obesity is an established risk factor for a wide range of comorbidities. In this context, based on the potential benefits of physical activity has on cognitive functioning, it is highly recommended that this should be implemented in daily routine, especially for the older population, to prevent cognitive decline and other health disorders.
References
1. Rukadikar et al. Cureus 2023; 15. DOI:10.7759/CUREUS.42926. 2. O’Brien et al. Lancet Neurol 2017; 16: 465. 3. Gandhi et al. Int J Res Med Sci 2022; 10: 1100–4. 4. Meo et al. Obes Facts 2019; 12: 150–6. 5. Skinner et al. Ethn Dis 2017; 27: 387–94. 6. Ugalde-Muñiz et al. Oxid Med Cell Longev 2020; 2020. DOI:10.1155/2020/4807179. 7. Karczewski et al. International Journal of Molecular Sciences 2022, Vol 23, Page 6145 2022; 23: 6145. 8. Salas-Venegas et al. Front Integr Neurosci 2022; 16: 798995. 9. Yaffe et al. JAMA 2004; 292: 2237–42. 10. Braniste et al. Sci Transl Med 2014; 6: 263ra158. 11. Parker et al. Gut Microbes 2020; 11: 135. 12. Lindqvist et al. Eur J Neurol 2006; 13: 1385–8. 13. Farr et al. Endocrinology 2008; 149: 2628–36. 14. Anand et al. JAMA Netw Open 2022; 5: e2146324–e2146324. 15. Niedziela et al. Eur J Epidemiol 2014; 29: 801–12. 16. Doehner et al. Int J Cardiol 2012; 162: 20–6. 17. Skinner et al. Ethn Dis 2017; 27: 387–94. 18. Zhang et al. J Am Heart Assoc 2017; 6. DOI:10.1161/JAHA.117.005561. 19. Roderka et al. Clin Geriatr Med 2020; 36: 631. 20. Kronschnabl et al. PLoS One 2021; 16: e0249651. 21. Pitrou et al. European Review of Aging and Physical Activity 2022; 19: 1–13. 22. Xu et al. BMC Geriatr 2024; 24: 1–10.
Answers for CME quiz of Feature Story Issue 23:





